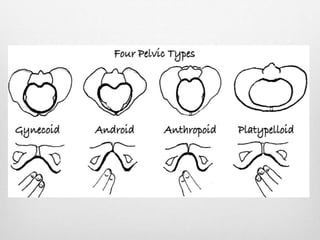
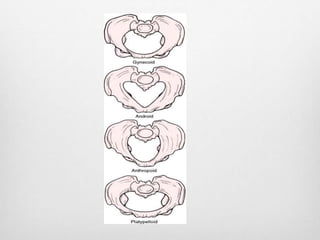
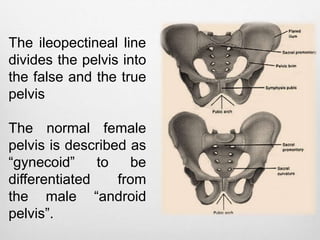
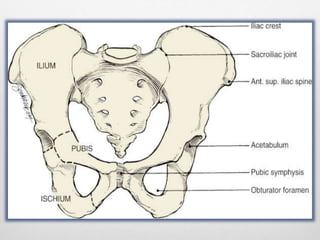
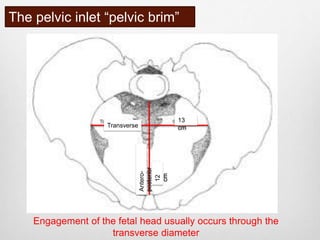
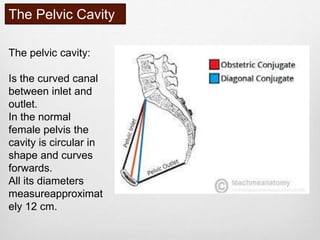
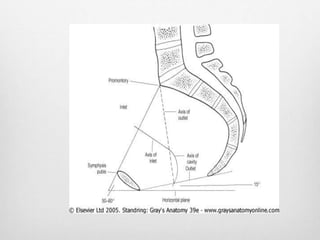
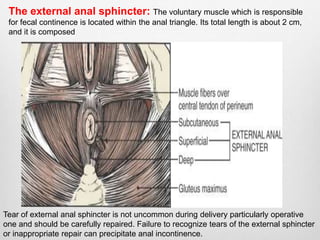
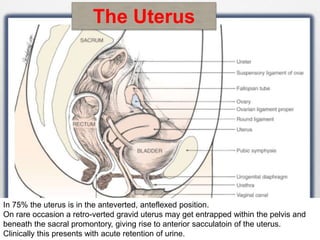
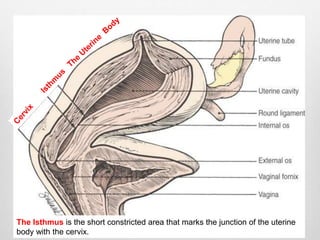
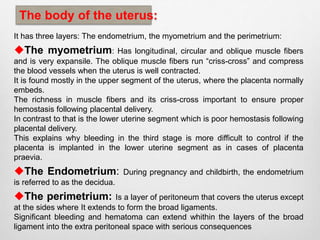
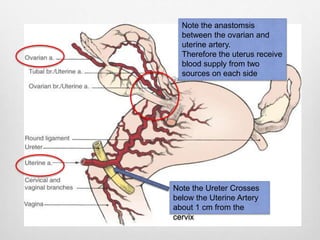
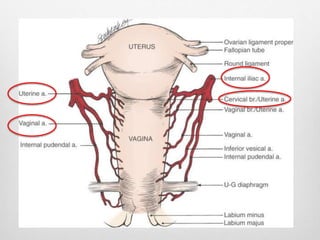
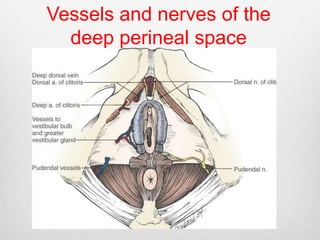
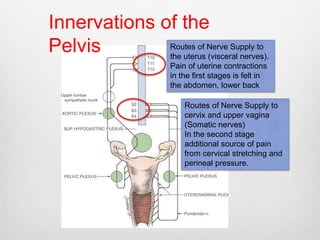
The document provides an overview of the clinical anatomy of the female pelvis for obstetricians. It describes the bony pelvis, pelvic cavity, pelvic outlet, ligaments, diaphragm, perineum including the urogenital and anal triangles. It also details the uterus, cervix, vascular supply, and innervation of the pelvis. Key points include the divisions of the pelvis, diameters for fetal engagement, levator ani muscles, pudendal neurovascular bundle, layers of the uterus, vascular anastomoses supplying the uterus, and nerve routes for uterine and cervical pain.