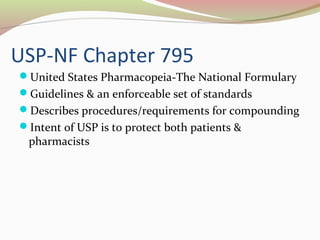
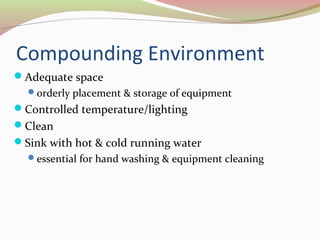
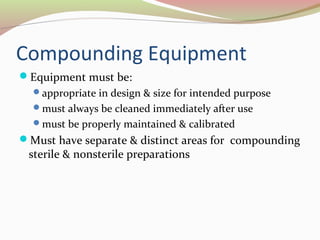
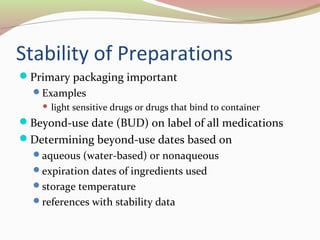
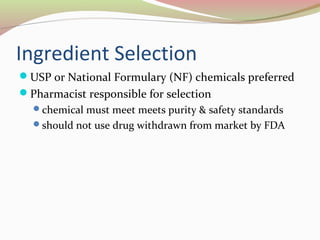
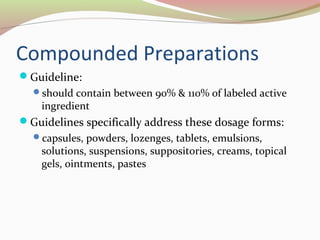
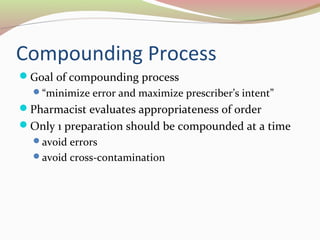
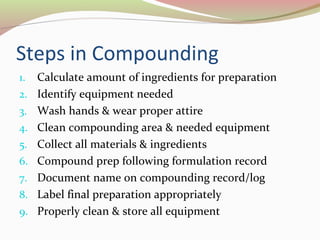
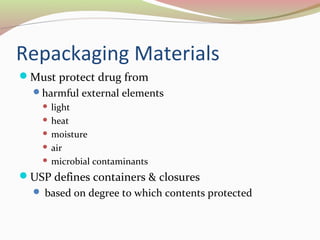
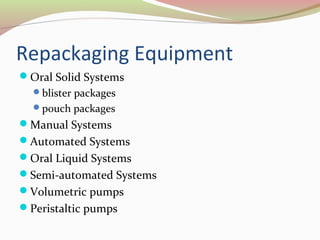
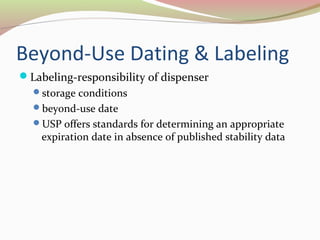
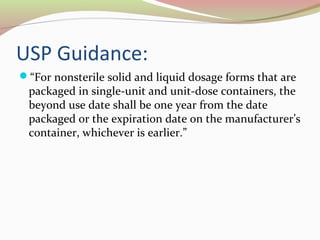
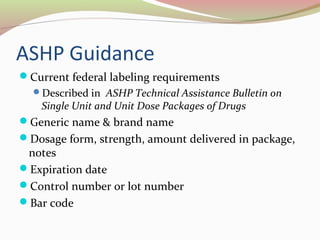
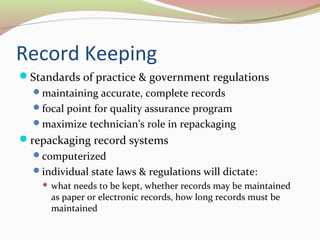
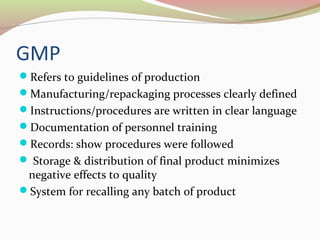
This document outlines key concepts regarding compounding and repackaging of medications. It defines compounding as preparing medications tailored to individual patients. The document describes common compounding equipment, formulations like ointments and capsules, and the importance of record keeping. It also explains that repackaging involves transferring medications from bulk containers into individual patient packages, with proper packaging, labeling, and expiration dating required. Maintaining high quality practices through adherence to standards and regulations is emphasized.