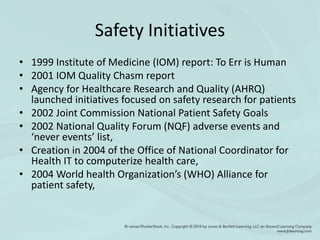
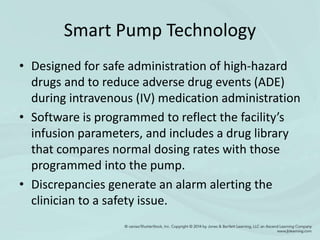
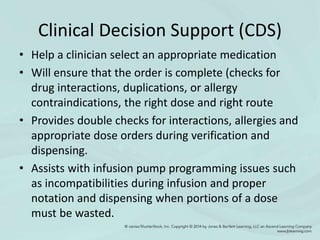
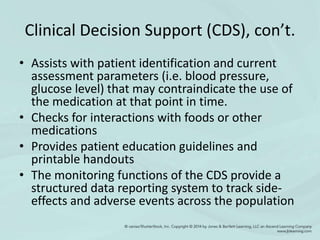
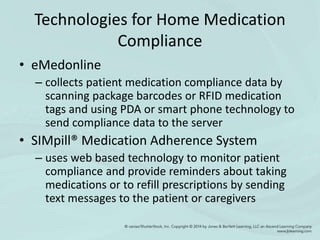
Nursing professionals have an ethical duty to ensure patient safety. Various safety initiatives and technologies have aimed to promote safety and reduce errors. Informatics tools can integrate into the medication administration cycle through technologies like computerized physician order entry, barcoded medication administration, smart pumps, and clinical decision support. These technologies perform checks, provide alerts, and assist with decisions to help ensure the five rights of medication administration and reduce human errors.