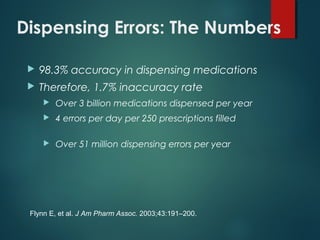
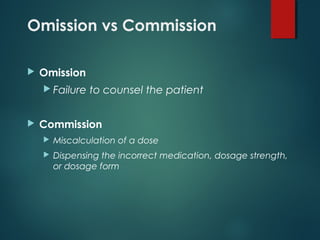
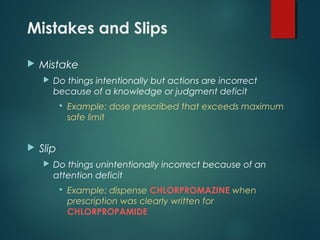
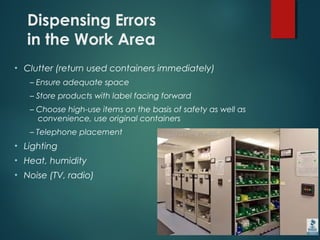
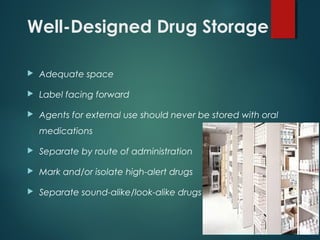
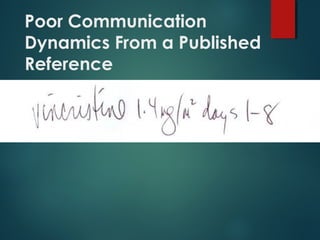
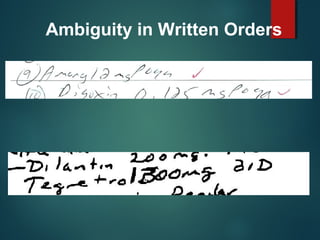
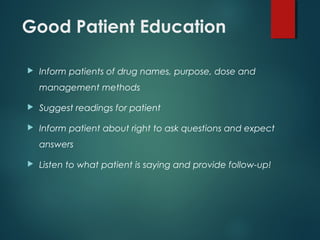
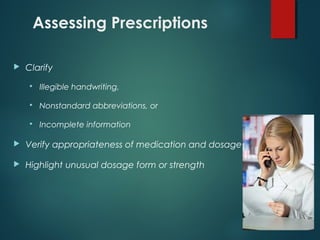
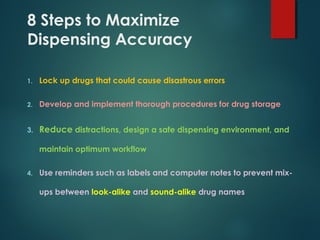
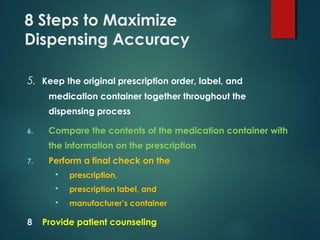
This document discusses ways to prevent dispensing errors in pharmacies. It begins by providing dispensing error rates and examples of common errors like incorrect medications or dosages. Environmental factors that can cause errors like distractions, workload, and poor storage are described. The roles of mistakes versus slips and omission versus commission errors are defined. Methods to reduce errors through better organization, labeling, counseling, verification processes and limiting distractions are recommended. Computerized systems can help but also introduce new risks. The importance of education and communication are emphasized for minimizing dispensing inaccuracies.