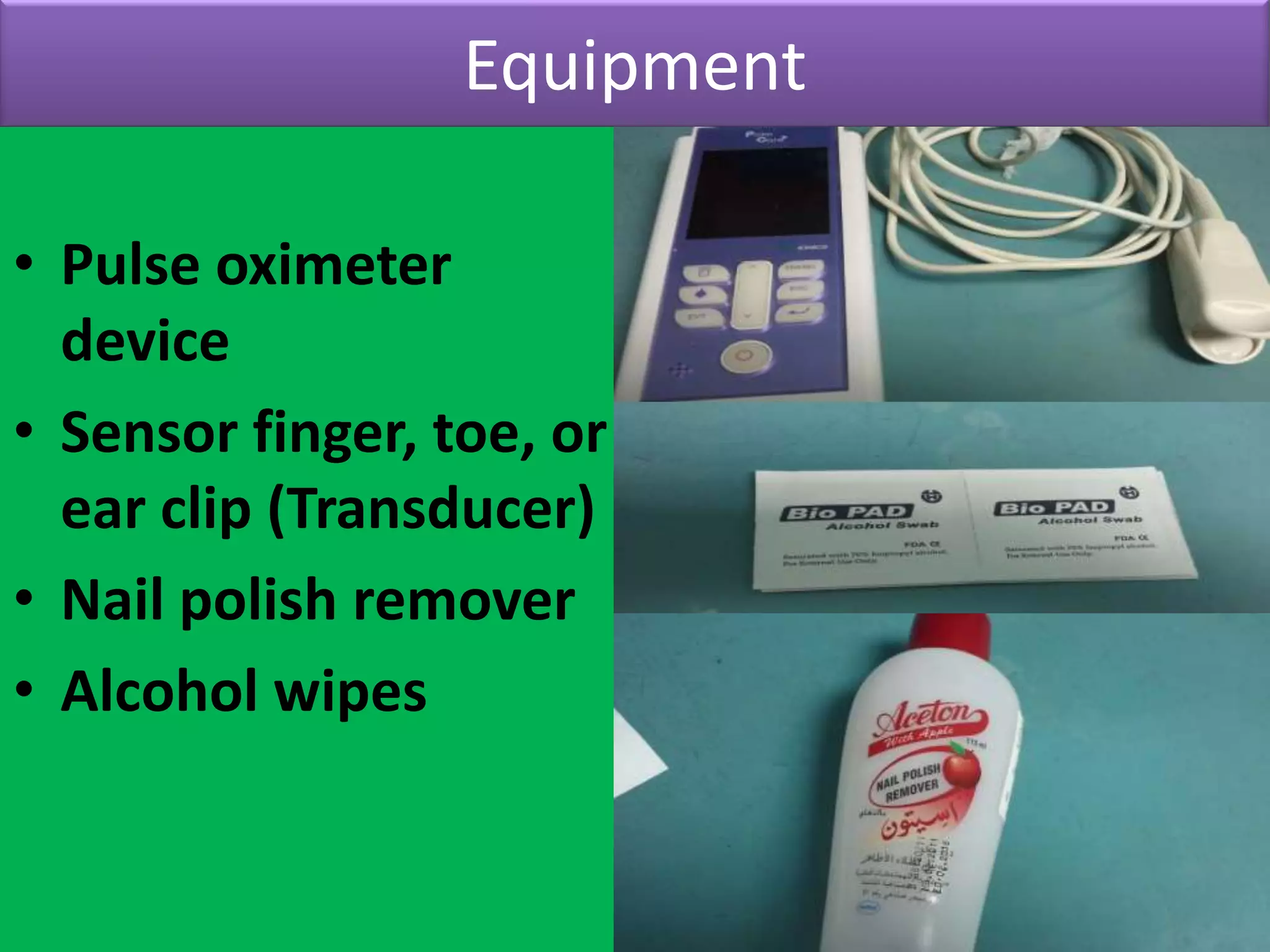
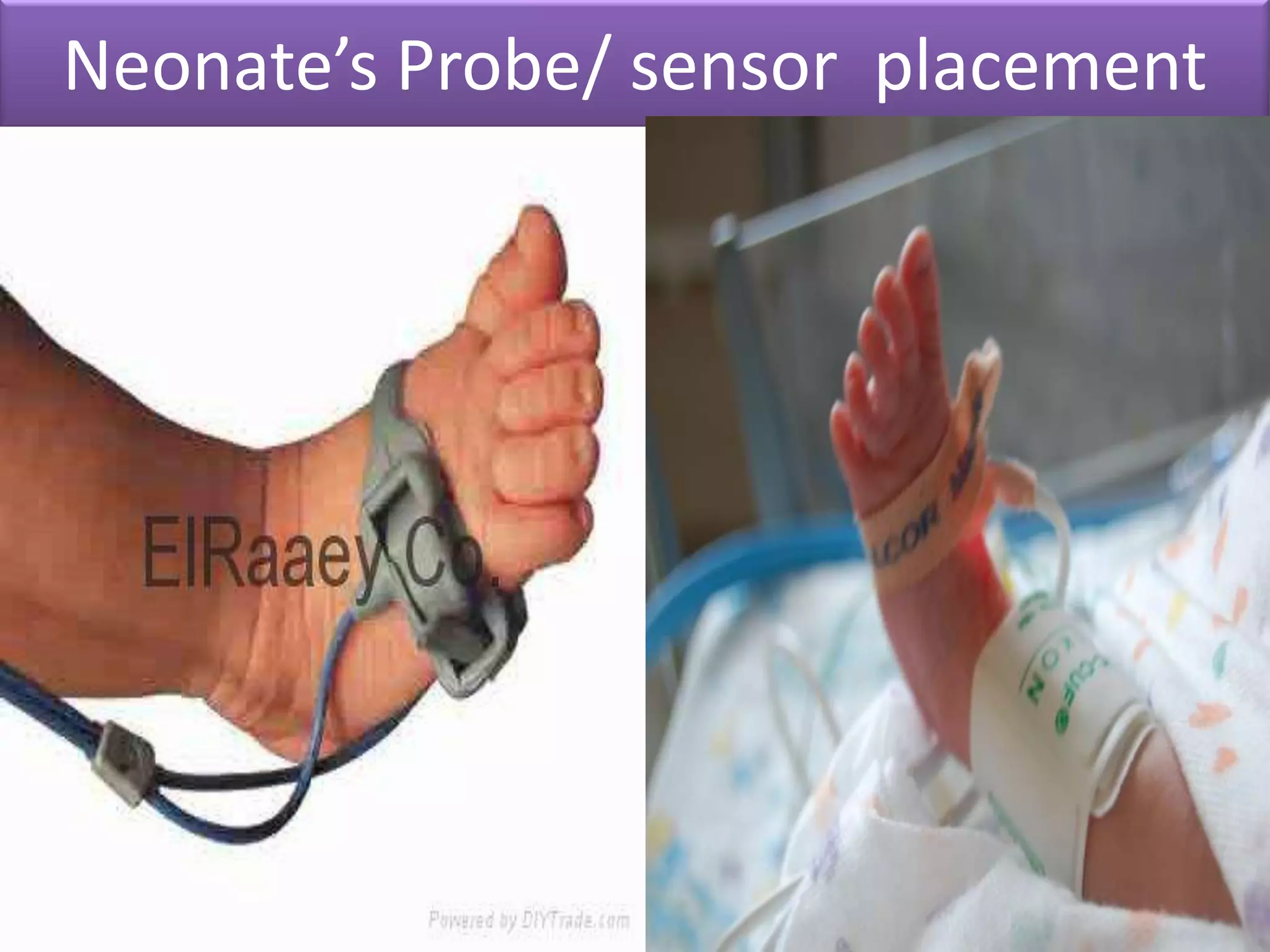
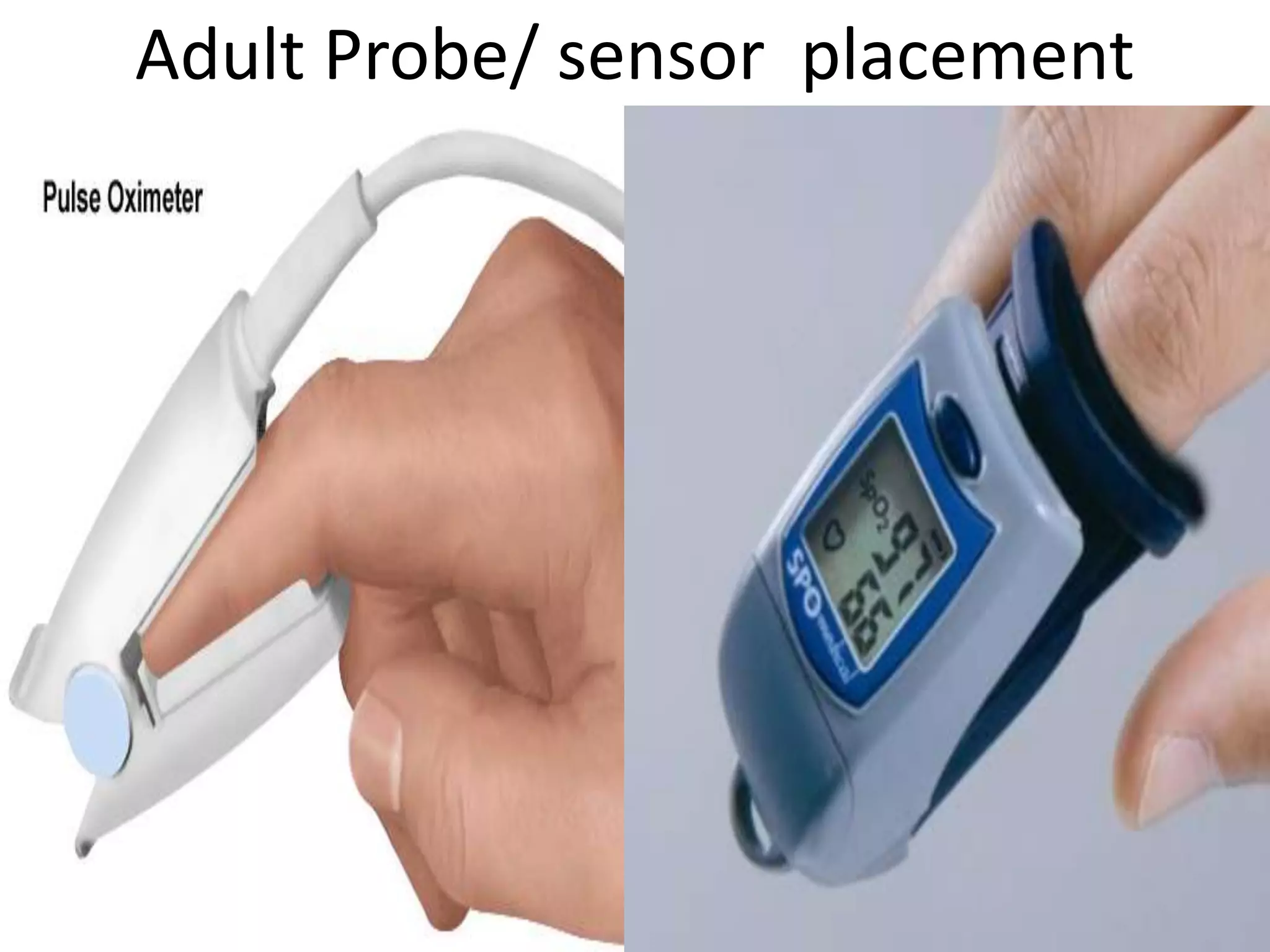
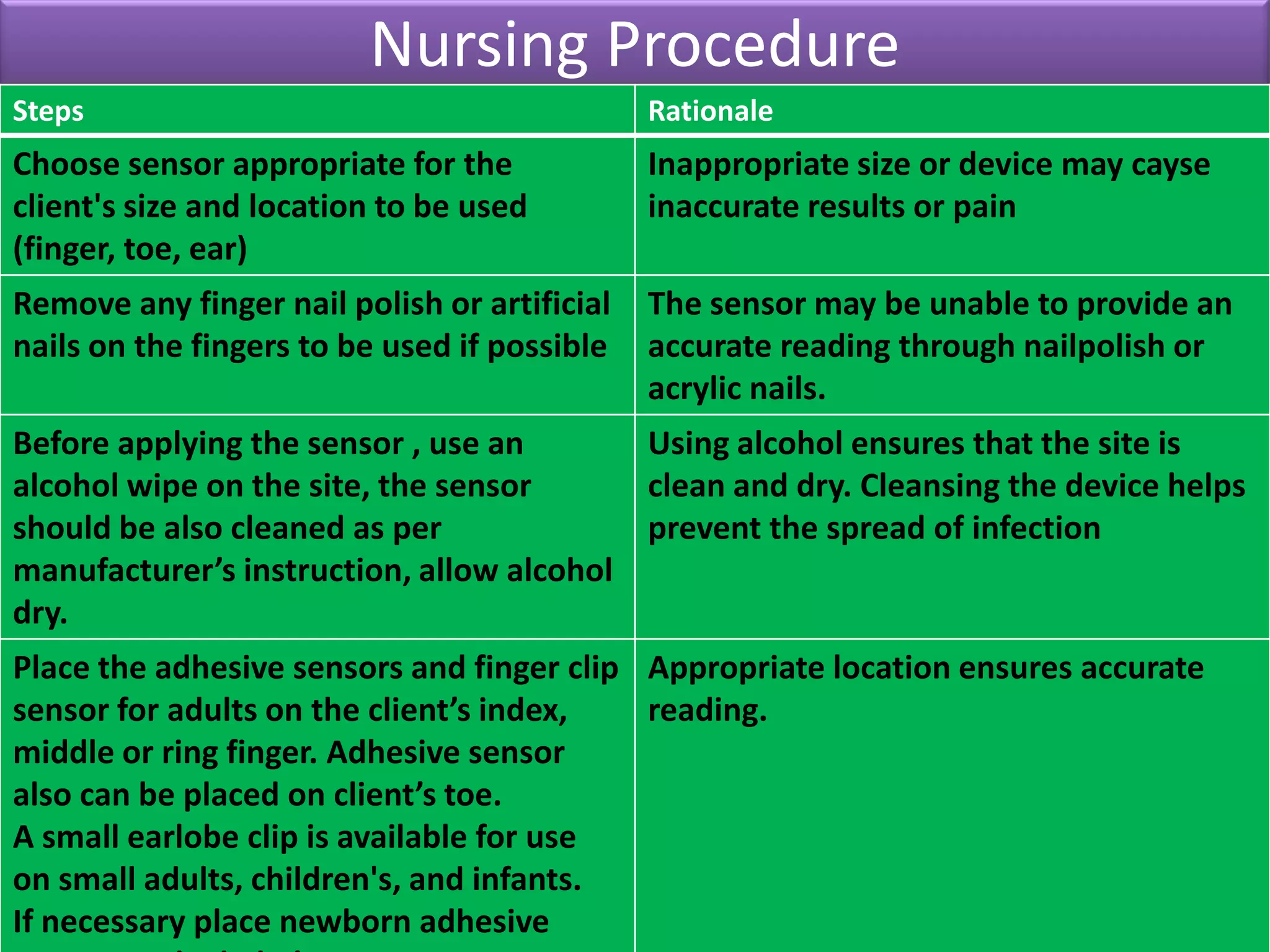
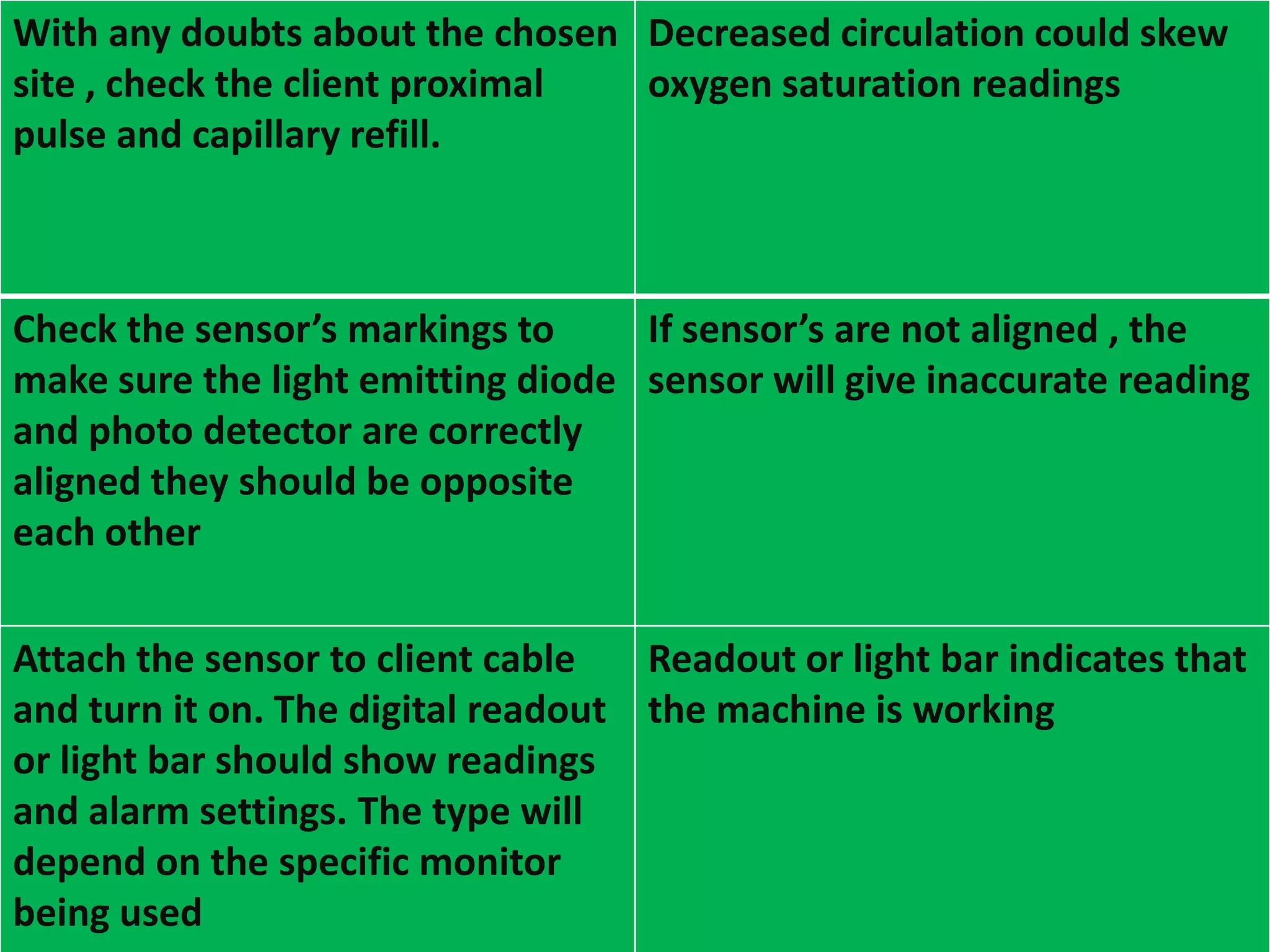
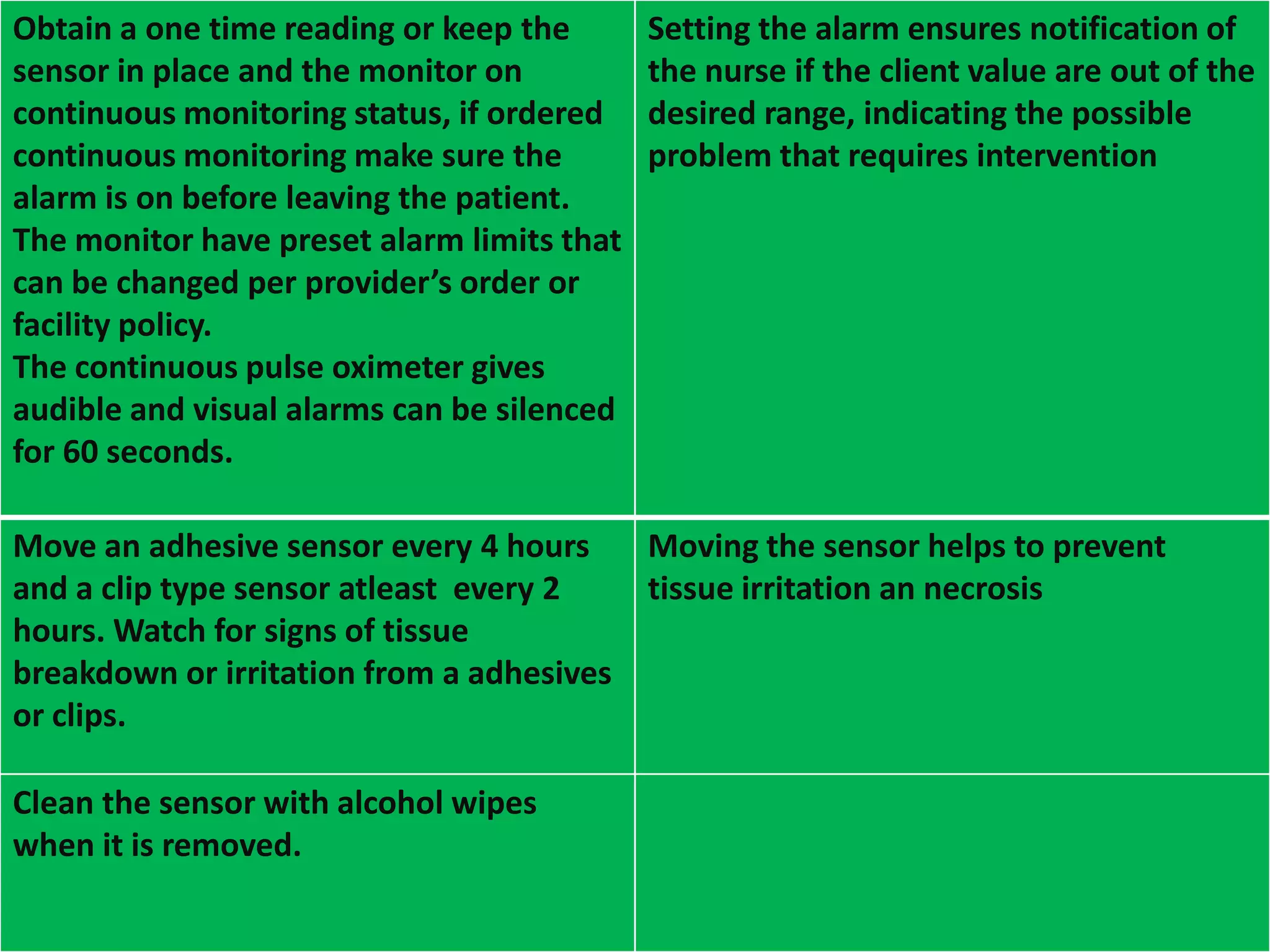
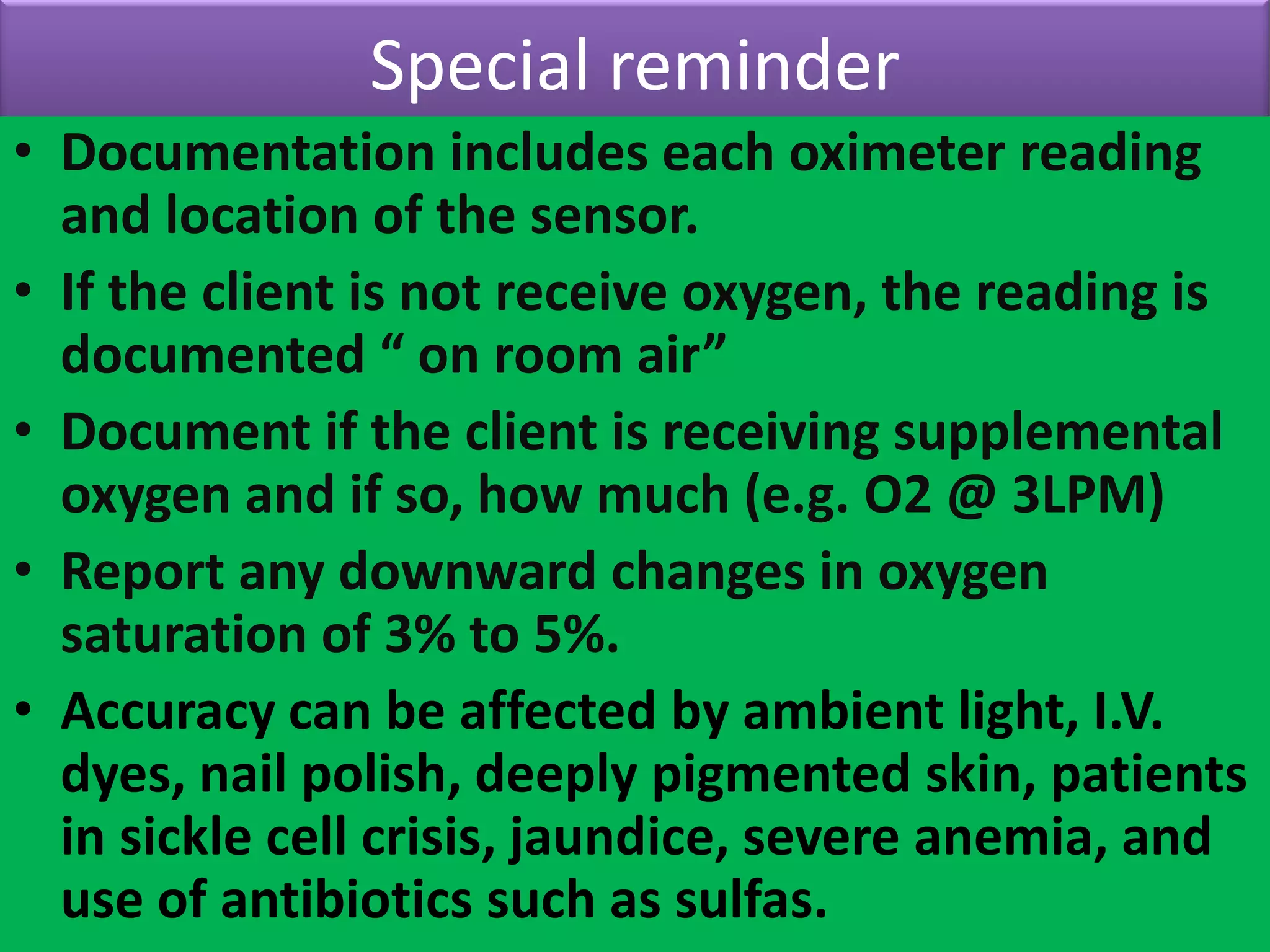
Pulse oximetry is a non-invasive method to estimate arterial oxygen saturation by passing light through tissue to measure oxygenated hemoglobin. It provides early detection of hypoxemia but values can be unreliable in certain conditions like shock or methemoglobinemia. Pulse oximetry is useful for monitoring critically ill patients, evaluating oxygen therapy effectiveness, and determining supplemental oxygen needs. Proper use requires cleaning areas and ensuring correct sensor placement and alignment.