This document discusses common childhood diseases, with a focus on respiratory illnesses. It covers:
1. Common respiratory diseases in children include respiratory infections (ARI), pneumonia, and diseases like asthma that are exacerbated by respiratory infections.
2. Children are particularly vulnerable to respiratory illnesses due to developmental differences like smaller airways and fewer alveoli.
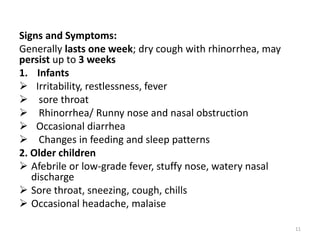
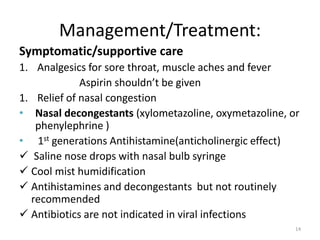
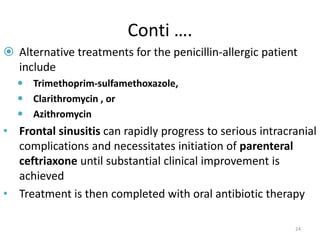
3. Specific respiratory diseases covered include the common cold, influenza, sinusitis, otitis media (ear infections), tonsillitis, and pneumonia. Signs and symptoms, diagnoses, and treatment approaches are discussed for each.

































![Etiology
• The most important agents causing pharyngitis
are Viruses
• Sore throat can be caused by many viruses and
bacteria.
• Mostly viral as parts of URTI:-(adenoviruses,
rhinoviruses, respiratory syncytial virus [RSV],
herpes simplex virus [HSV]).
• Group A ß-hemolytic streptococcus is the most
common and the most important bacterial
agent.
38](https://image.slidesharecdn.com/chapter4pedippt-220823144404-c176fb96/85/chapter-4-pedi-ppt-pptx-38-320.jpg)