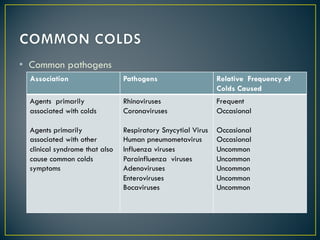
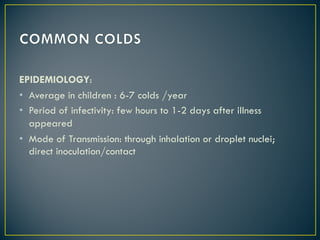
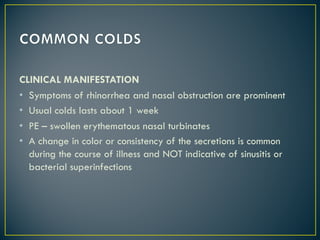
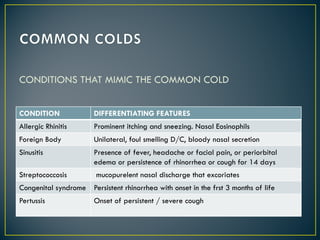
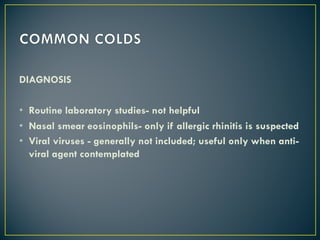
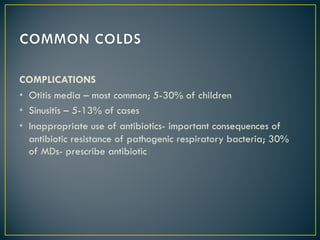
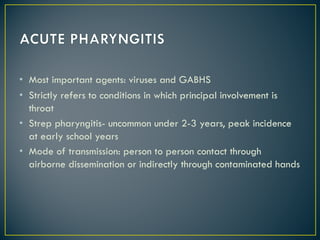
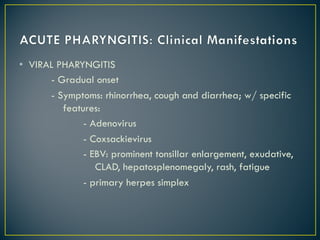
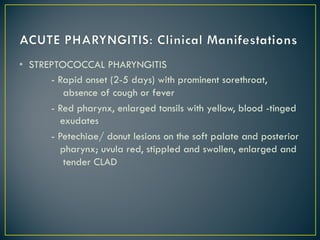
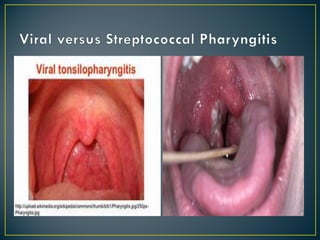
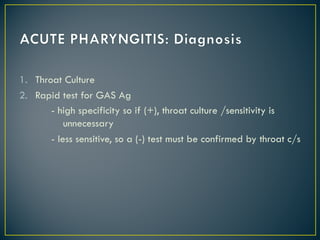
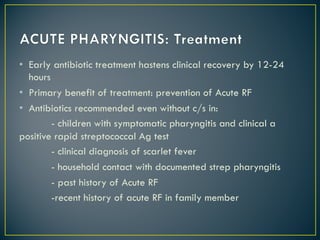
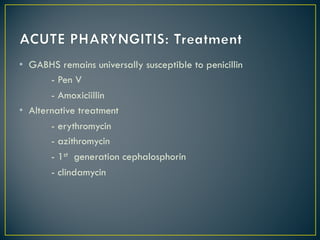
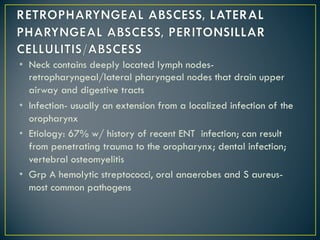
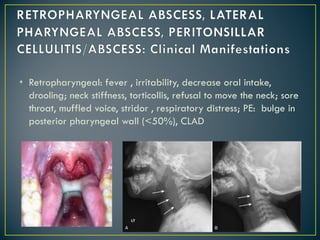
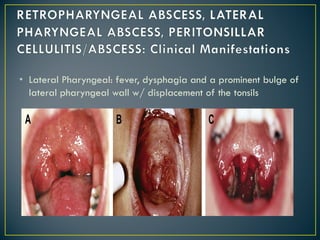
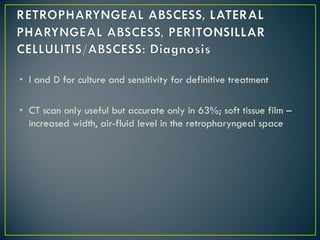
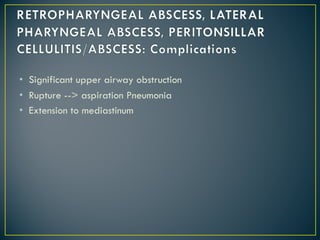
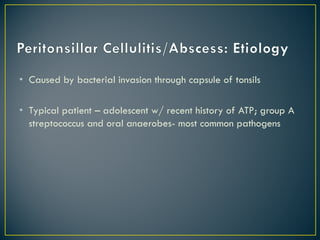
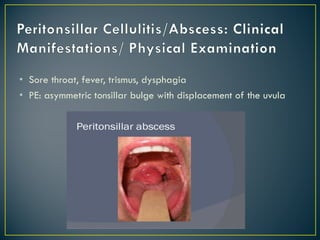
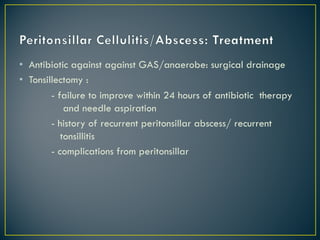
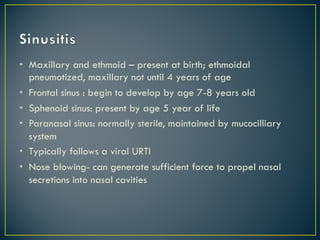
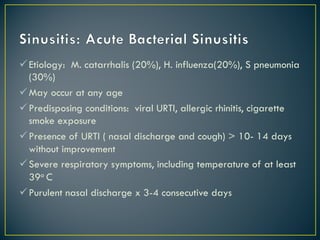
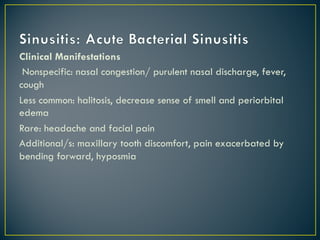
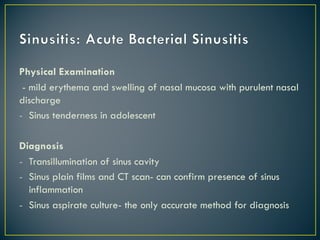
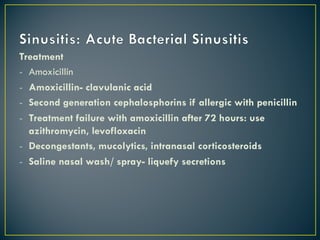
This document discusses common upper respiratory conditions in children including the common cold, pharyngitis, neck infections, tonsillitis, and sinusitis. It provides details on the typical pathogens, clinical manifestations, diagnosis, and treatment of each condition. The common cold is usually viral in origin while pharyngitis can be viral or strep-related. Neck infections include retropharyngeal and lateral abscesses. Tonsillitis can lead to peritonsillar abscess. Sinusitis typically follows a viral upper respiratory infection. Symptoms, exams, and appropriate antibiotic treatment are outlined for each condition.