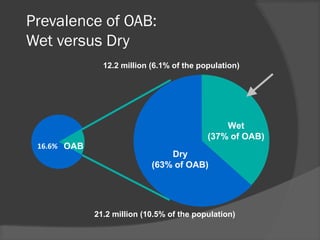
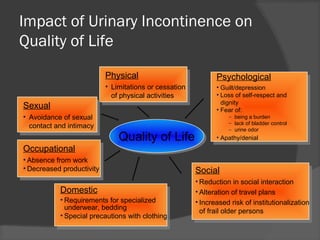
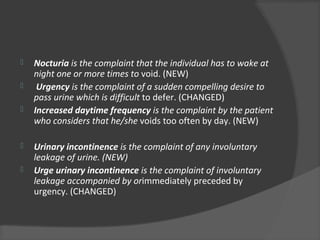
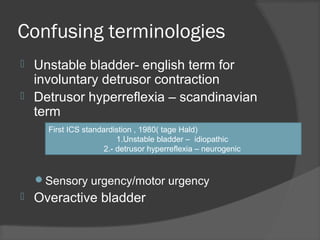
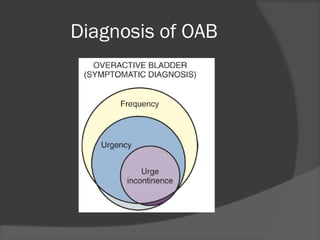
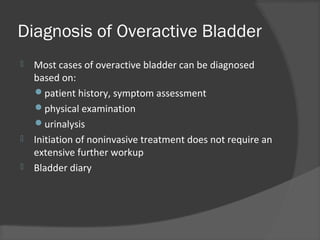
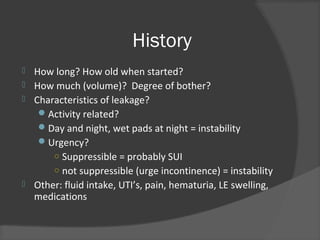
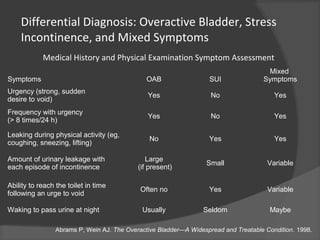
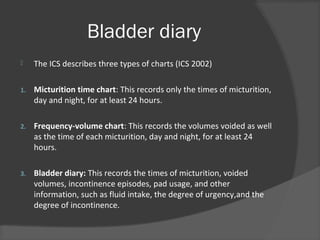
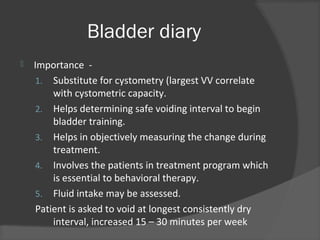
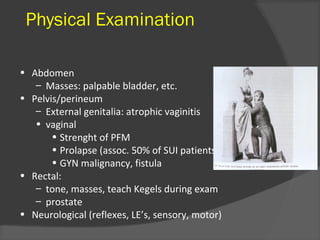
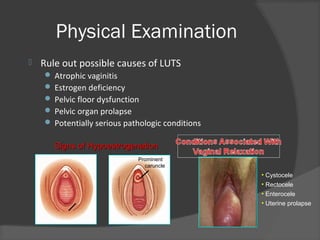
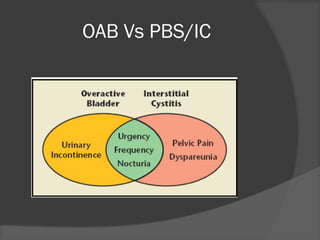
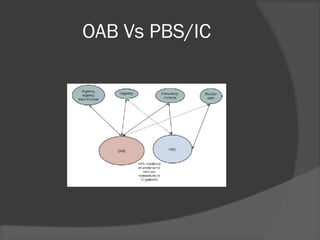
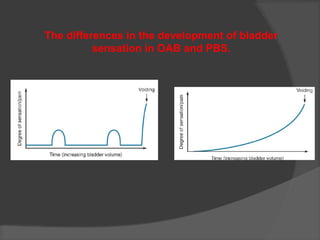
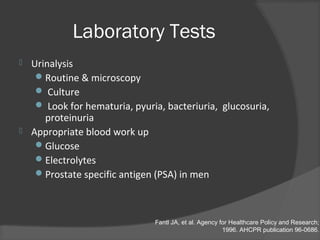
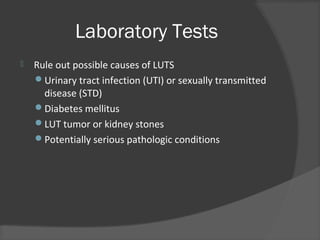
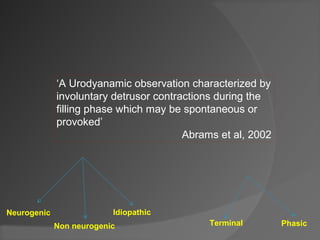
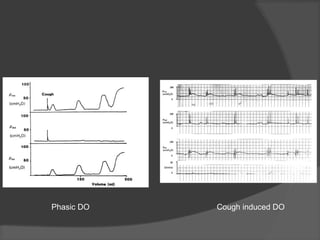
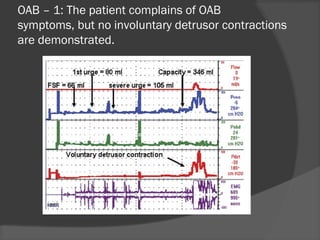
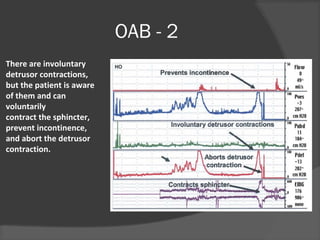
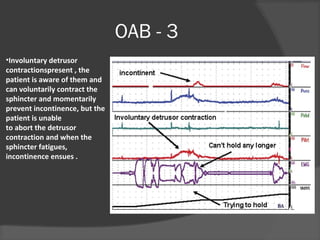
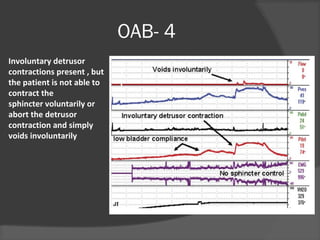
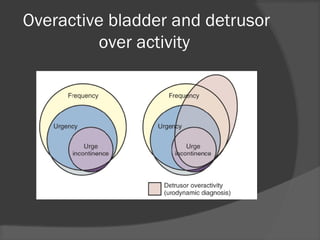
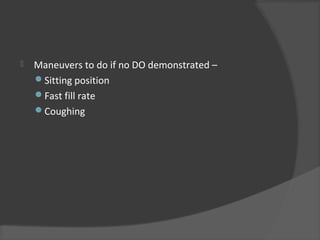
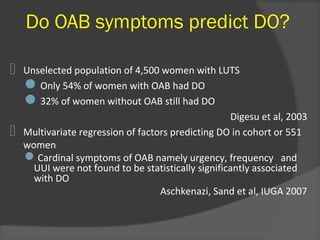
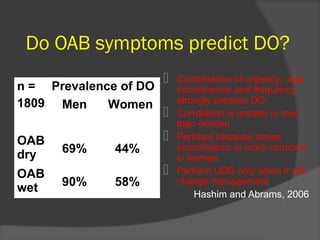
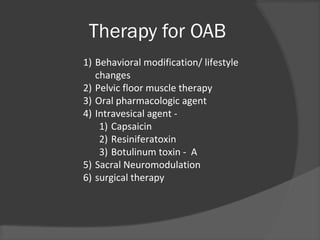
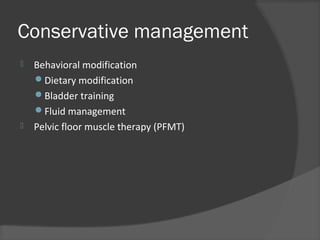
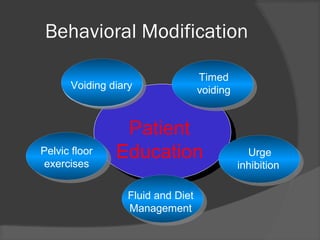
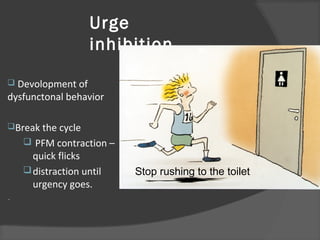
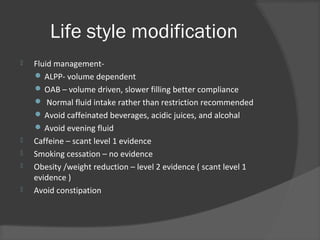
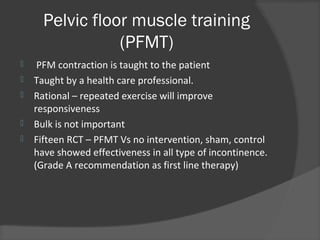
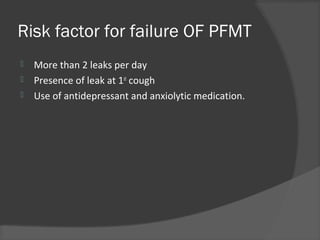
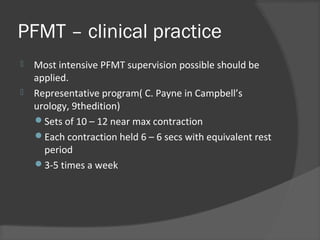
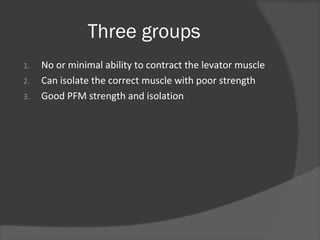
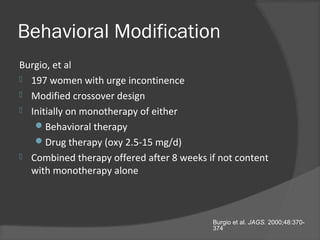
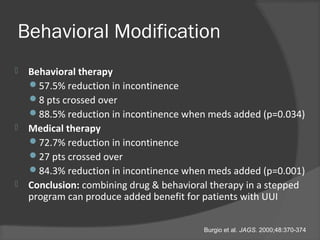
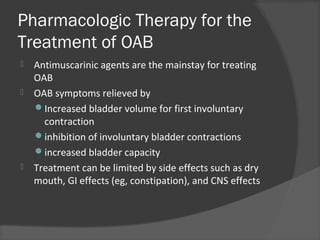
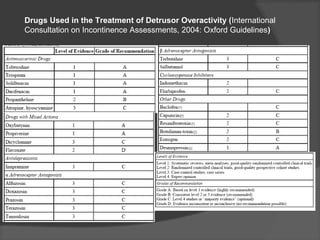
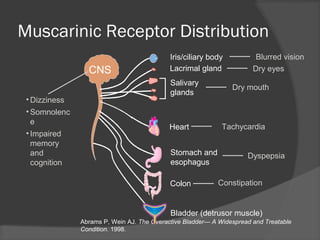
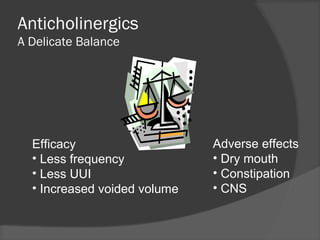
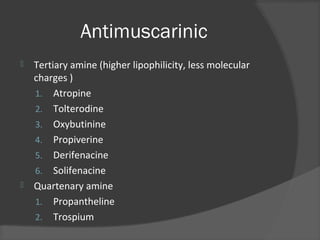
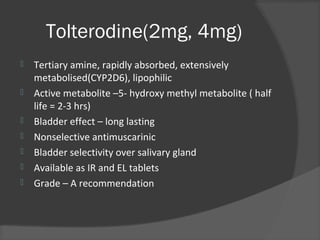
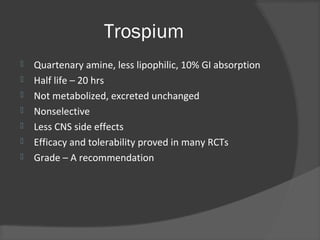
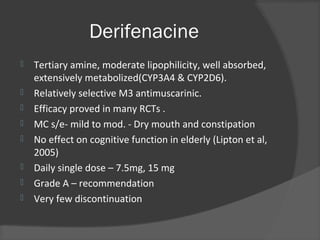
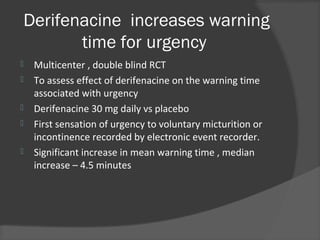
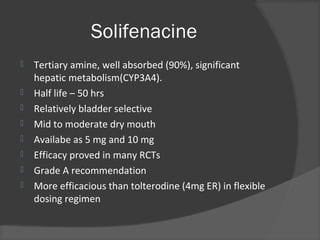
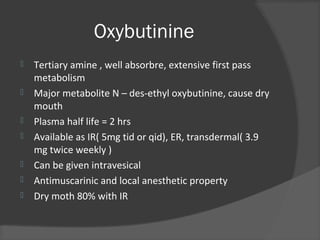
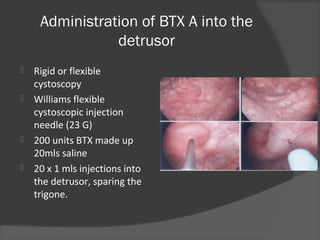
This document discusses Dr. Santosh Agrawal's background and credentials as a urologist and kidney transplant surgeon. It then provides information on overactive bladder (OAB), including definitions, prevalence statistics, quality of life impacts, incidence being underreported, and OAB classification systems. Diagnosis of OAB is discussed, covering patient history, physical exam, lab tests, bladder diaries, and urodynamics. Conservative management options like behavioral modification, bladder training, pelvic floor muscle therapy, and pharmacologic therapies are summarized. Specific drugs for treating detrusor overactivity like tolterodine are also mentioned.