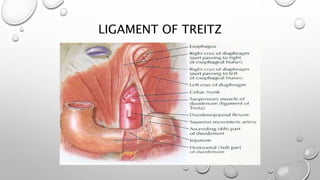
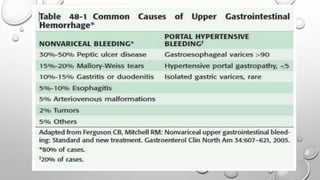
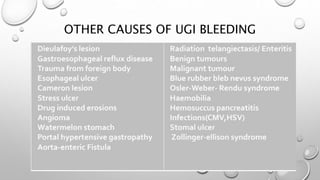
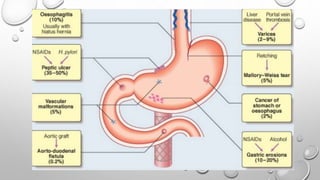
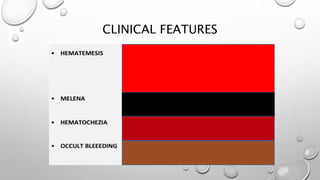
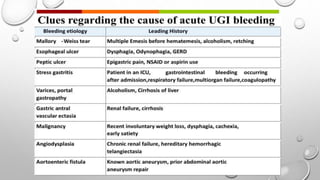
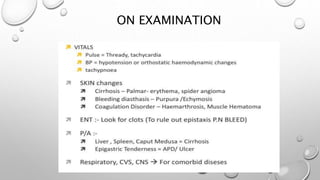
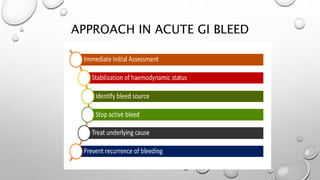
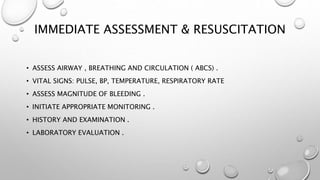
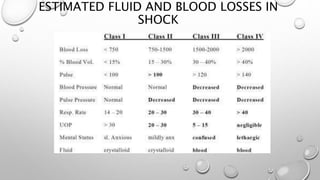
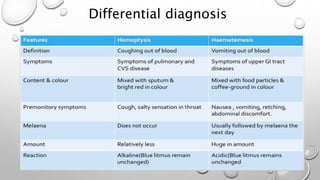
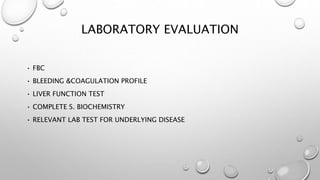
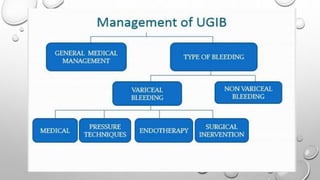
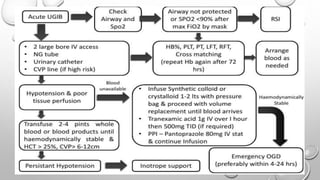
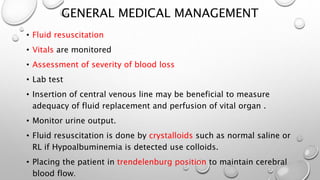
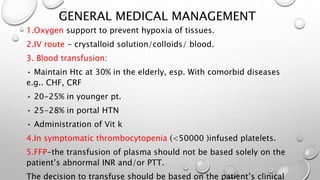
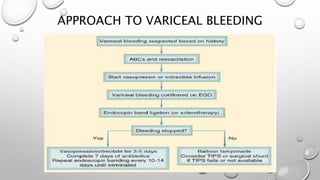
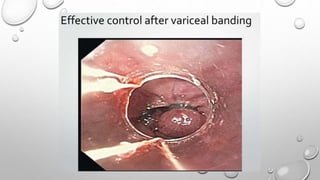
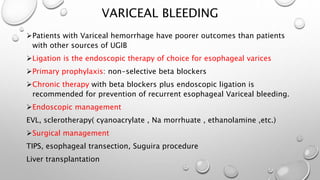
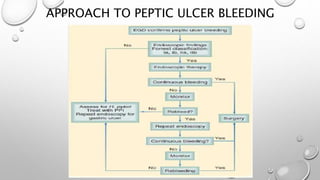
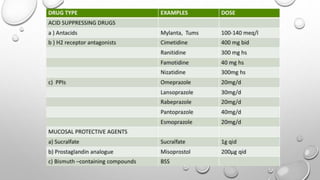
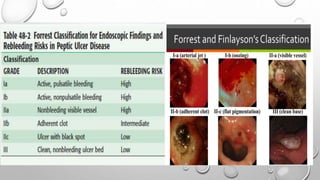
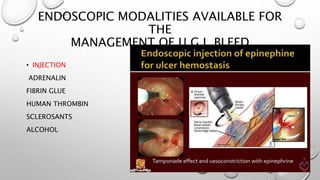
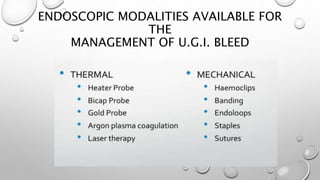
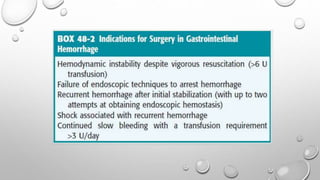
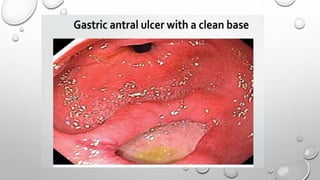
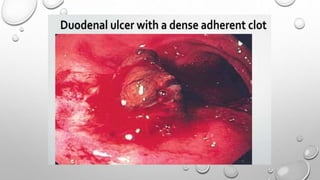
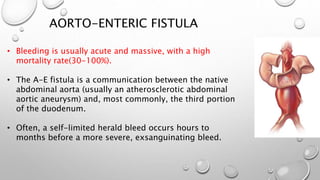
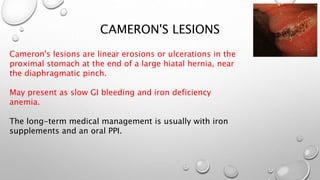
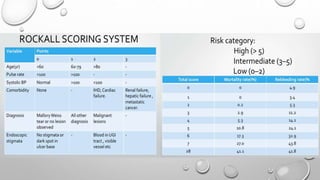
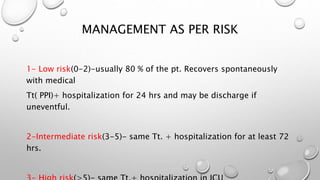
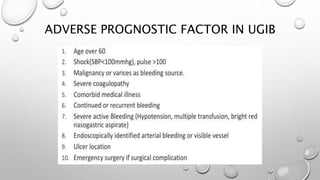
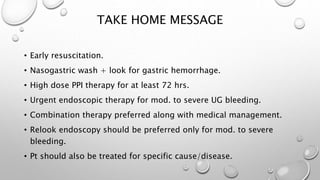
Upper GI bleeding can occur anywhere in the GI tract proximal to the ligament of Treitz. The majority of cases are non-variceal upper GI bleeding, with peptic ulcers being the most common cause. Initial management involves resuscitation, monitoring, lab tests, and fluid replacement. Patients are then risk stratified as low, intermediate, or high risk to guide further treatment and length of hospital stay. Endoscopic intervention is preferred for moderate to severe bleeding to achieve hemostasis through methods like injection, cauterization, or clips. Ongoing treatment depends on the underlying cause but generally involves acid suppression and management of comorbidities.