1. Respiration involves gas exchange, host defense, and metabolism. It includes pulmonary ventilation, diffusion of gases between alveoli and blood, and transport of gases through the body.
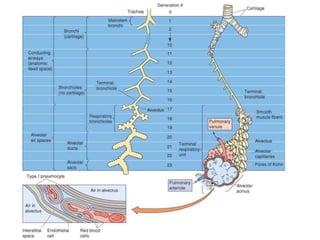
2. The respiratory system has an upper airway and lower airway. The lower airway is made up of the trachea, bronchi, and alveoli. The alveoli are the sites of gas exchange.
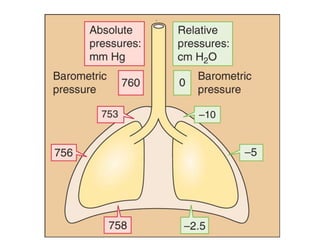
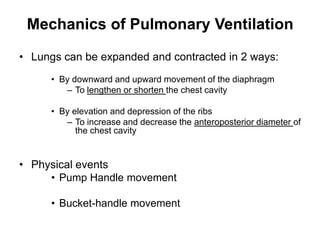
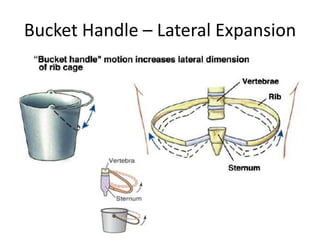
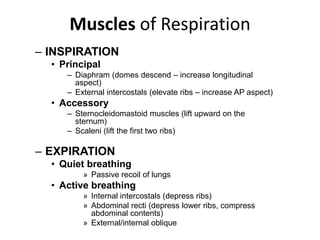
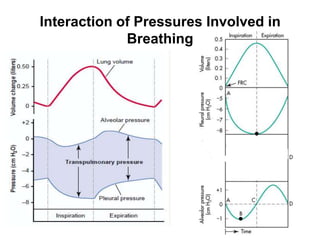
3. During inspiration, the diaphragm and external intercostal muscles contract to expand the lungs and lower intrapleural pressure. During expiration, elastic recoil of the lungs and chest wall passively return the lungs to the resting volume.