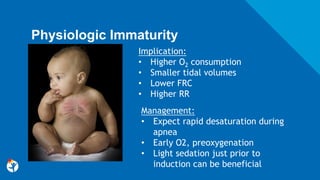
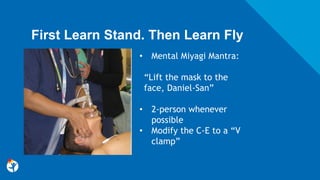
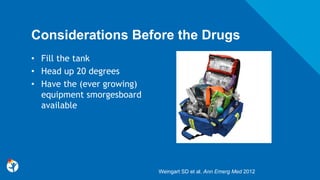
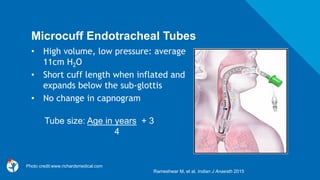
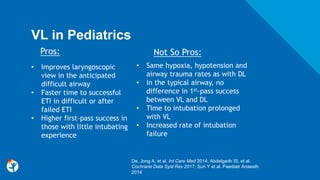
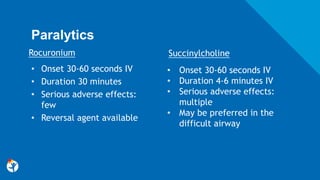
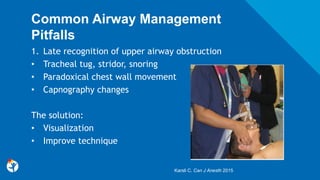
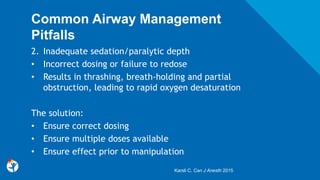
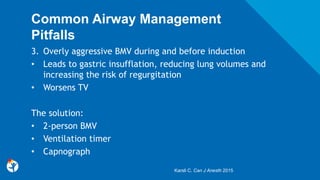
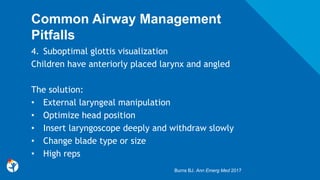
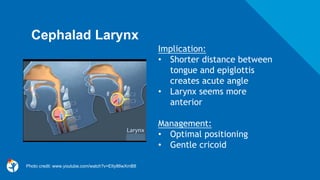
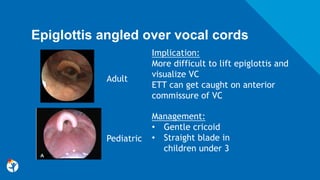
This document discusses best practices for pediatric airway management. It begins by outlining differences between pediatric and adult airways that make intubation more challenging in children, such as a prominent occiput, cephalad larynx, large tongue, and elliptical larynx. Predictors of difficult pediatric intubation are identified as age under 1, congenital anomalies, low BMI, and history of difficult intubation. The document then reviews optimal pre-oxygenation, induction agents like ketamine and etomidate, paralytics like rocuronium, and equipment like microcuffed tubes and video laryngoscopy that can facilitate intubation. Common pitfalls like inadequate sedation and aggressive bag-mask ventilation are




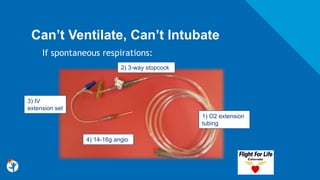
![Shape of larynx
Management:
• Critical to have
multiple sizes of
ETT
Implication:
• Elliptical shape of
cricoid ring
• ETT may seem
“stuck” just
beyond cords
Harless, J et al. Int J Crit Illn Inj Sci 2014Photo credit: In Coté CJ, Ryan JF, Todres ID, et al [eds]: A
Practice of Anesthesia for Infants and Children.](https://image.slidesharecdn.com/pediatricairway-180420155808/85/Pediatric-Airway-Management-12-320.jpg)