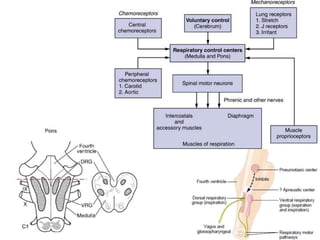
This document discusses the regulation of respiration through central and peripheral chemoreceptors. It covers:
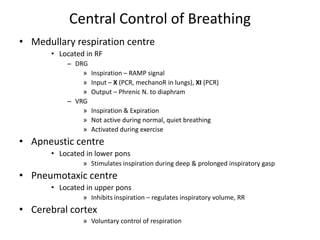
1) The central control of breathing located in the medulla including the dorsal respiratory group (DRG), ventral respiratory group (VRG), apneustic center, and pneumotaxic center.
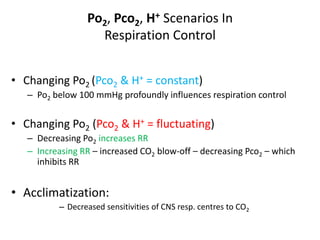
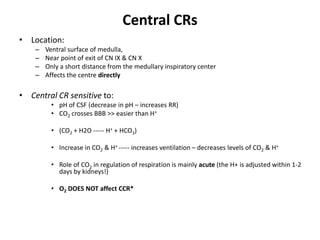
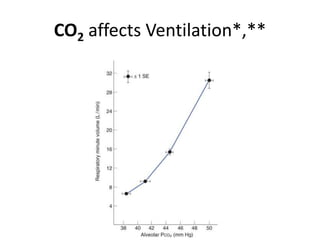
2) The central chemoreceptors (CCR) located in the medulla which are sensitive to changes in pH and CO2 levels in the cerebrospinal fluid and blood. Increased CO2 and decreased pH stimulate increased ventilation.
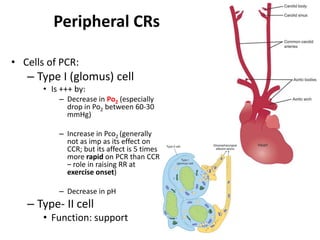
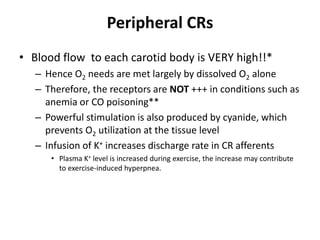
3) The peripheral chemoreceptors (PCR) located in the carotid bodies which are stimulated by decreased oxygen levels and increased CO2 and hydrogen ions. The PCR

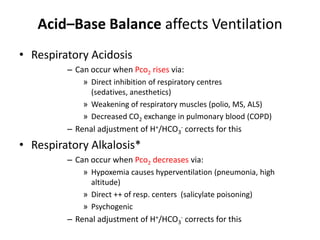
![Acid–Base Balance affects VentilationRespiratory response in Metabolic Acidosis E.g due to accumulation of acid ketone bodies DMResponse: Pronounced respiratory stimulation (Kussmaul breathing) The hyperventilation decreases alveolar PCO2 ("blows off CO2") Thus produces a compensatory fall in blood [H+]Respiratory response in Metabolic AlkalosisE.g: protracted vomiting with loss of HCl from bodyResponse:Ventilation is depressed Arterial PCO 2 rises, raising the [H+]toward normal](https://image.slidesharecdn.com/respupload3-110623135953-phpapp02/85/Resp-upload3-10-320.jpg)