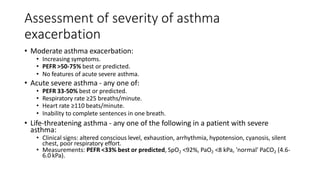
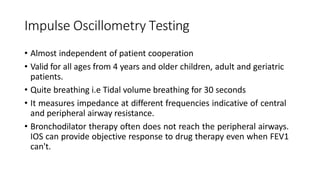
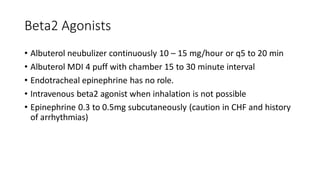
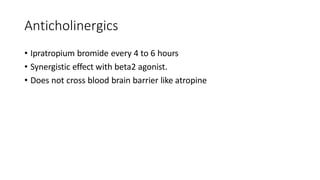
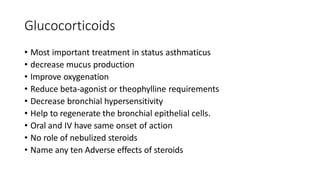
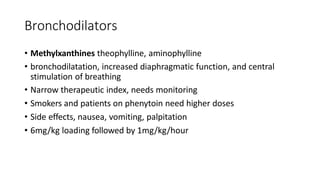
Status asthmaticus is a severe exacerbation of asthma that is unresponsive to initial treatment. It involves both an early bronchospastic component and later inflammatory response leading to airway obstruction. Treatment goals are to reverse airway obstruction, correct hypoxemia, and prevent complications. Mainstay treatments include nebulized beta-2 agonists, systemic steroids, theophyllines, and mechanical ventilation if needed. Impulse oscillometry testing can objectively monitor response to treatment. With aggressive treatment, prognosis is generally good except when combined with other conditions.