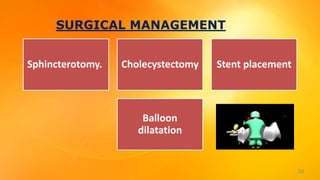
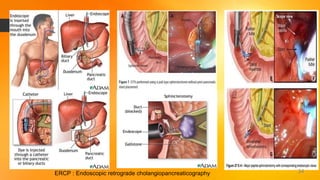
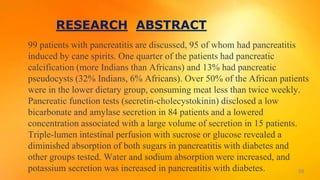
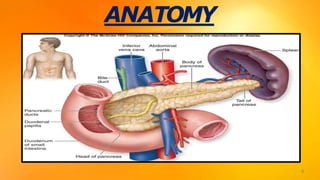
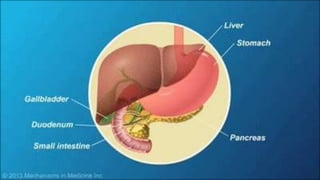
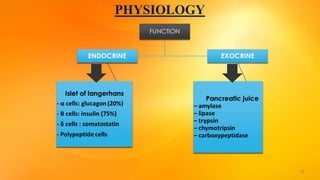
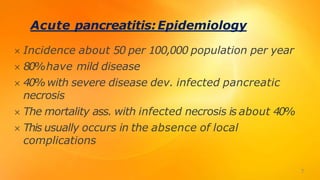
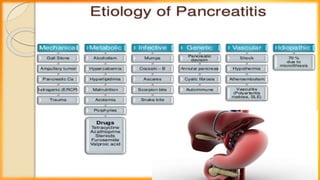
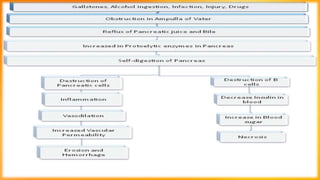
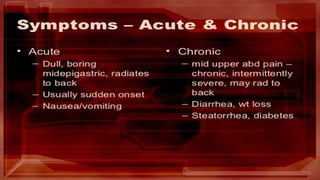
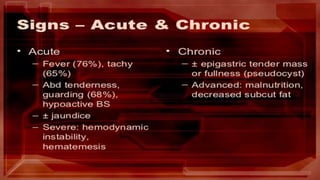
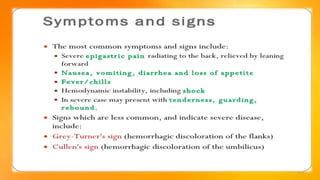
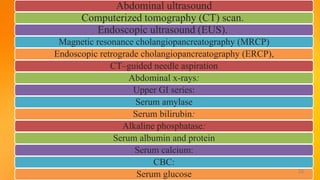
This document discusses pancreatitis, including its definition, types, causes, pathophysiology, signs and symptoms, diagnostic studies, complications, and management. Pancreatitis is inflammation of the pancreas that can damage the organ through premature activation of digestive enzymes. It can be acute, with rapid onset but potential reversibility, or chronic, resulting from irreversible structural changes over many years. Gallstones and alcohol are major causes. Diagnostic tests include blood tests, imaging like CT scans, and procedures like ERCP. Complications involve infection, pancreatic cancer, or nutritional issues. Treatment involves managing pain, treating underlying causes, and surgery in some cases. Nursing care focuses on pain management, fluid and nutrition management, and addressing related risks




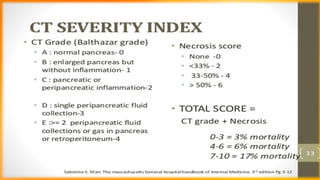
![Baseline CT scanning is indicated in the
following situations:(1) the diagnosis is in
doubt;(2) severe pancreatitis is suspected
because of high fever (higher than 38.8°
C[102°F]), distension and leukocytosis
CT Severity Index (Balthazar Score) in Acute
Pancreatitis
Helpful in assessing complications related to
acute pancreatitis or as a follow-up study in
patients who are clinically deteriorating](https://image.slidesharecdn.com/pancreatitis-191020123747/85/Pancreatitis-27-320.jpg)