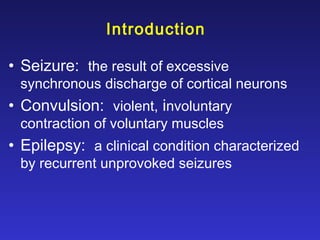
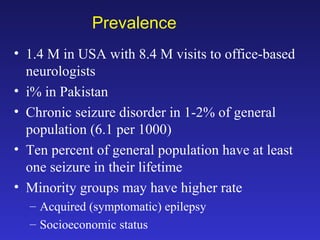
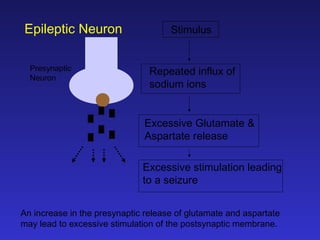
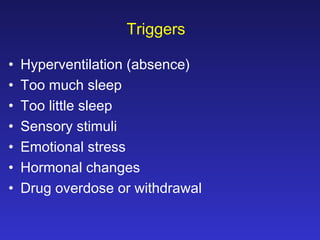
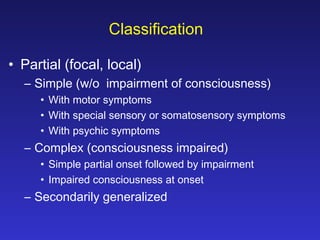
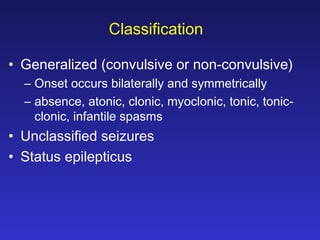
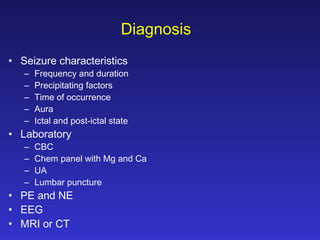
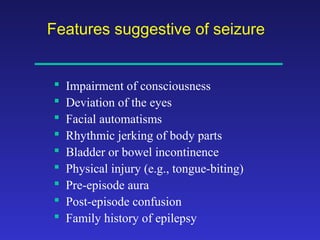
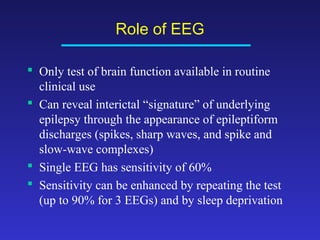
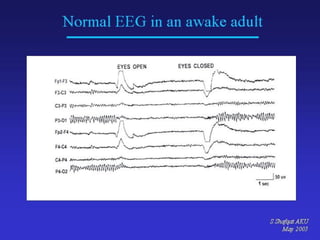
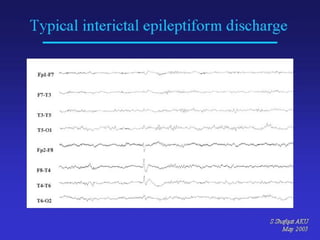
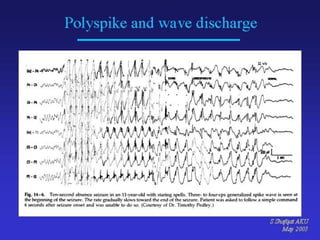
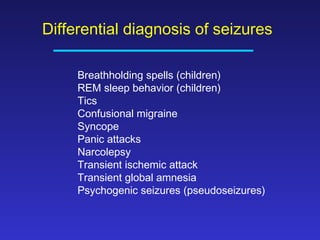
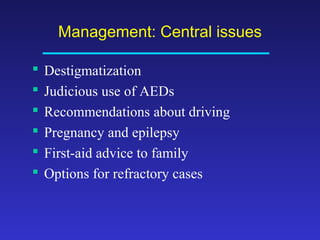
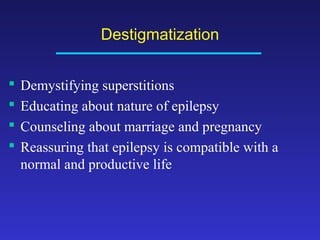
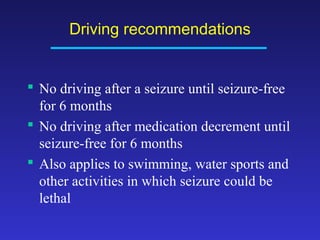
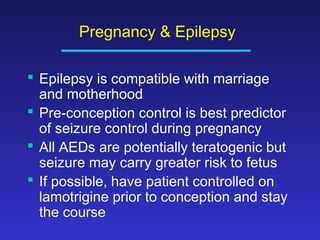
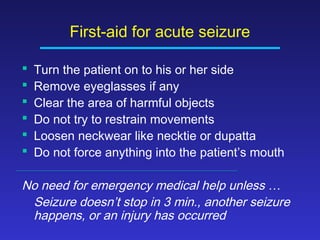
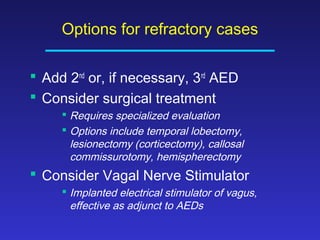
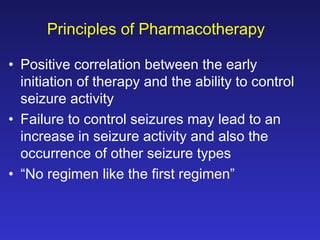
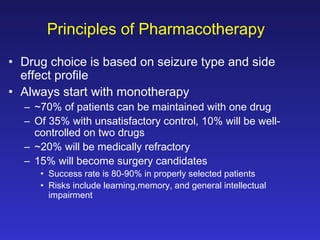
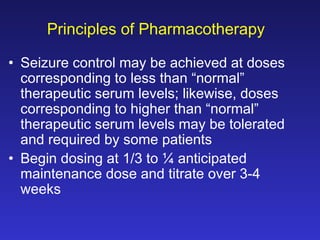
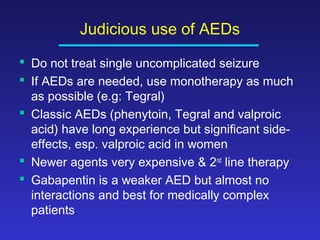
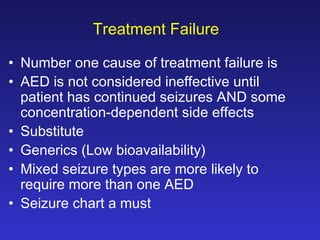
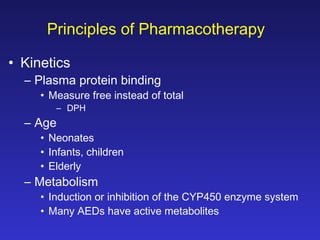
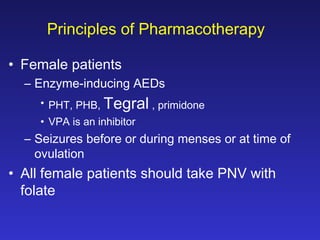
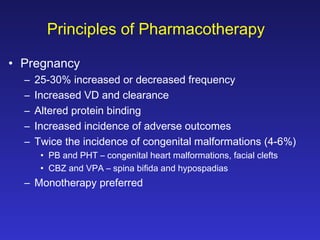
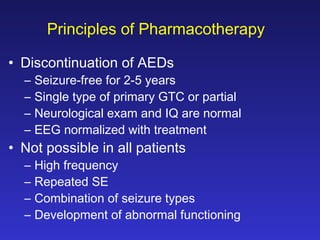
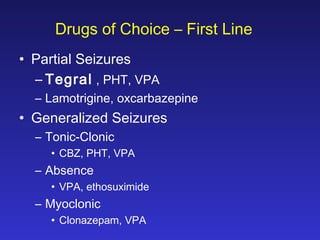
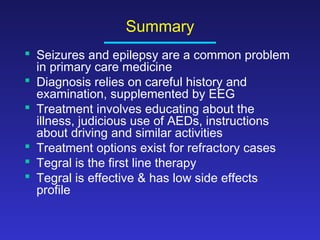
This document discusses epilepsy and seizure disorders. It defines key terms like seizure and epilepsy. It provides information on prevalence, classification, triggers, diagnosis and differential diagnosis. It discusses the role of EEG, evaluation, and management principles. These include destigmatization, driving recommendations, considerations during pregnancy, first aid, and options for refractory cases. Drug treatment focuses on monotherapy as first line using anti-epileptic drugs like Tegral which is effective with a low side effect profile.