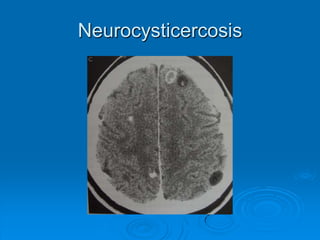
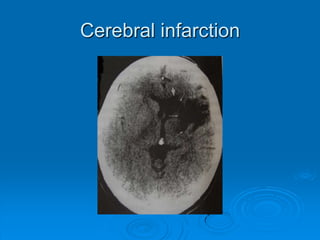
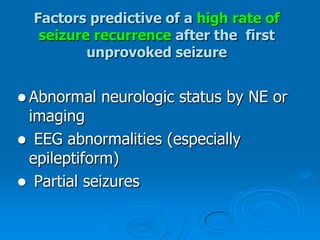
This document defines seizures and epilepsy, describes different types of seizures, and outlines evaluation and treatment approaches. It summarizes that seizures are caused by sudden bursts of electrical activity in the brain, epilepsy is defined as two or more unprovoked seizures, and evaluation involves medical history, physical exam, EEG, and sometimes neuroimaging to classify seizures and determine underlying causes and treatment.