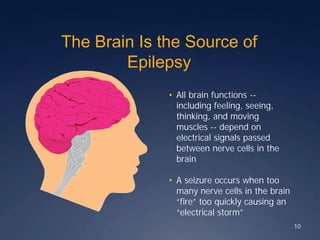
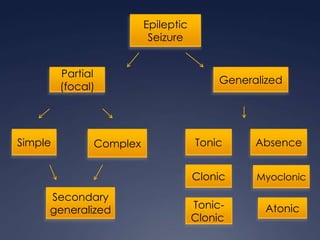
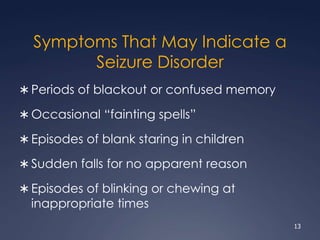
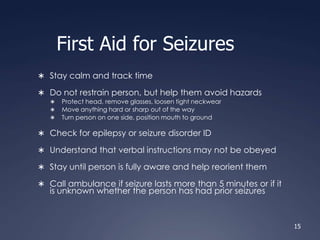
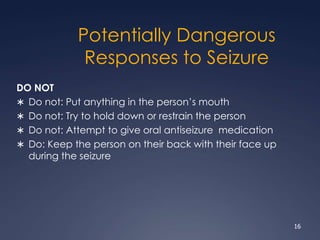
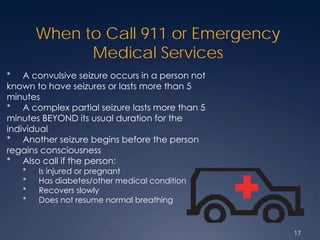
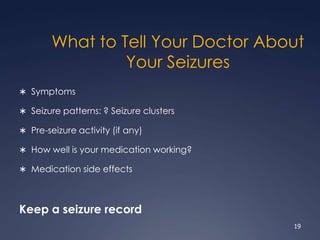
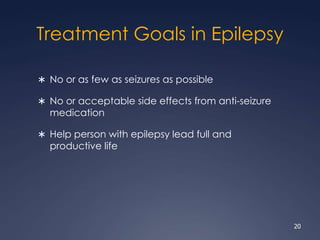
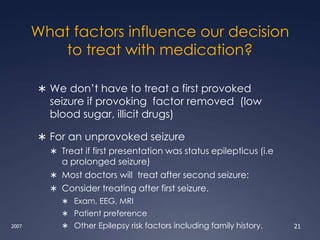
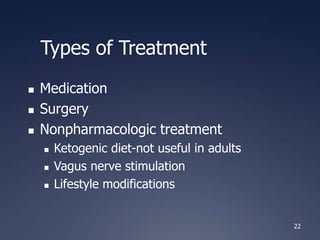
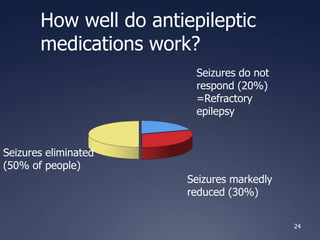
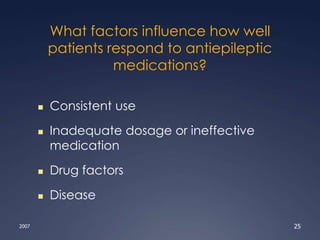
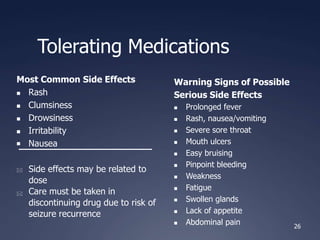
The document provides an overview of epilepsy and seizures, including the differences between the two, prevalence rates, risk factors, potential causes, and types of seizures. It also outlines diagnostic methods, treatment options such as medications and surgery, and the effects of epilepsy on individuals and families. Additionally, specific considerations for women and older adults with epilepsy are discussed, along with guidance for managing seizures and when to seek emergency help.