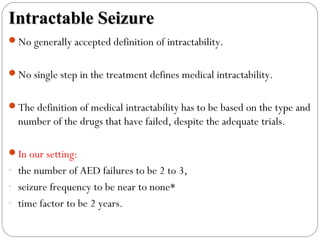
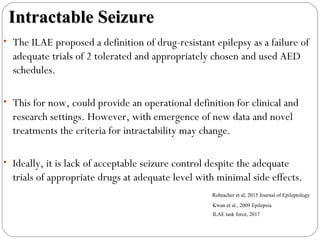
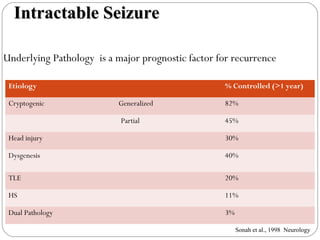
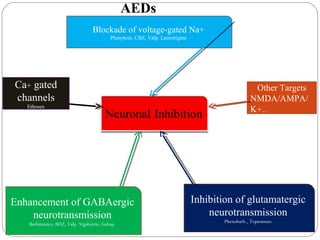
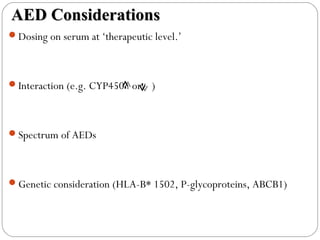
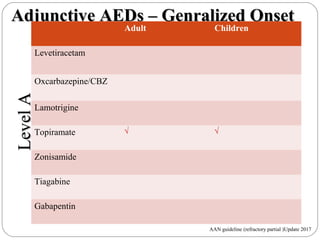
This document discusses the classification, management, and treatment of intractable epilepsy. It begins with summaries of the 2017 ILAE classification of seizure types and reminiscences of past classifications from 1981 and 2010. It then discusses definitions of intractable epilepsy, risk factors, current treatment approaches including antiepileptic drugs, surgery, diet, and ideal drug characteristics. Newer adjunctive drugs and their effectiveness are reviewed based on clinical studies and guidelines. The impact of uncontrolled seizures on quality of life and risks are highlighted. Controlled trials showing significantly better outcomes of surgery compared to continued medical therapy are also summarized.