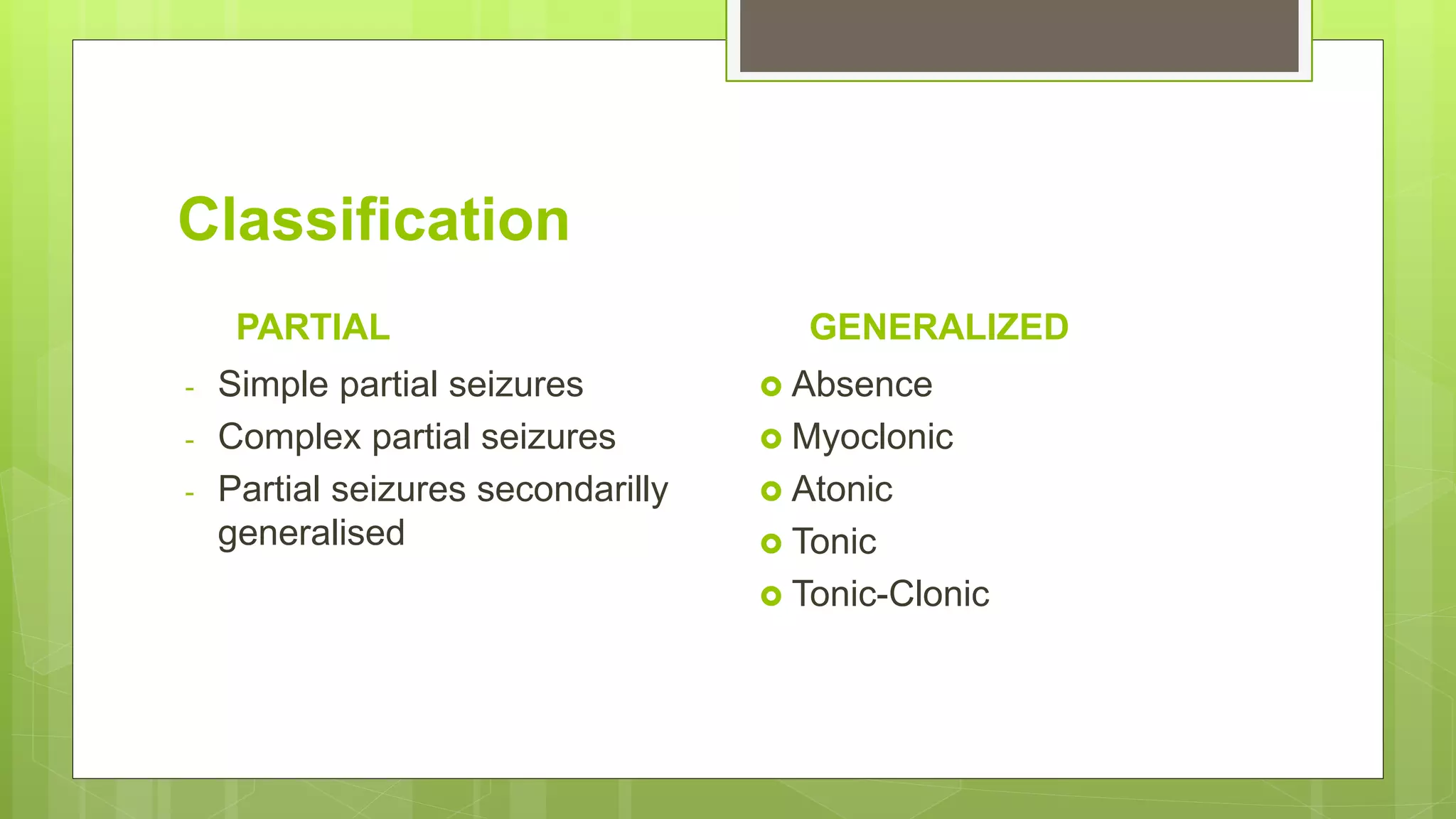
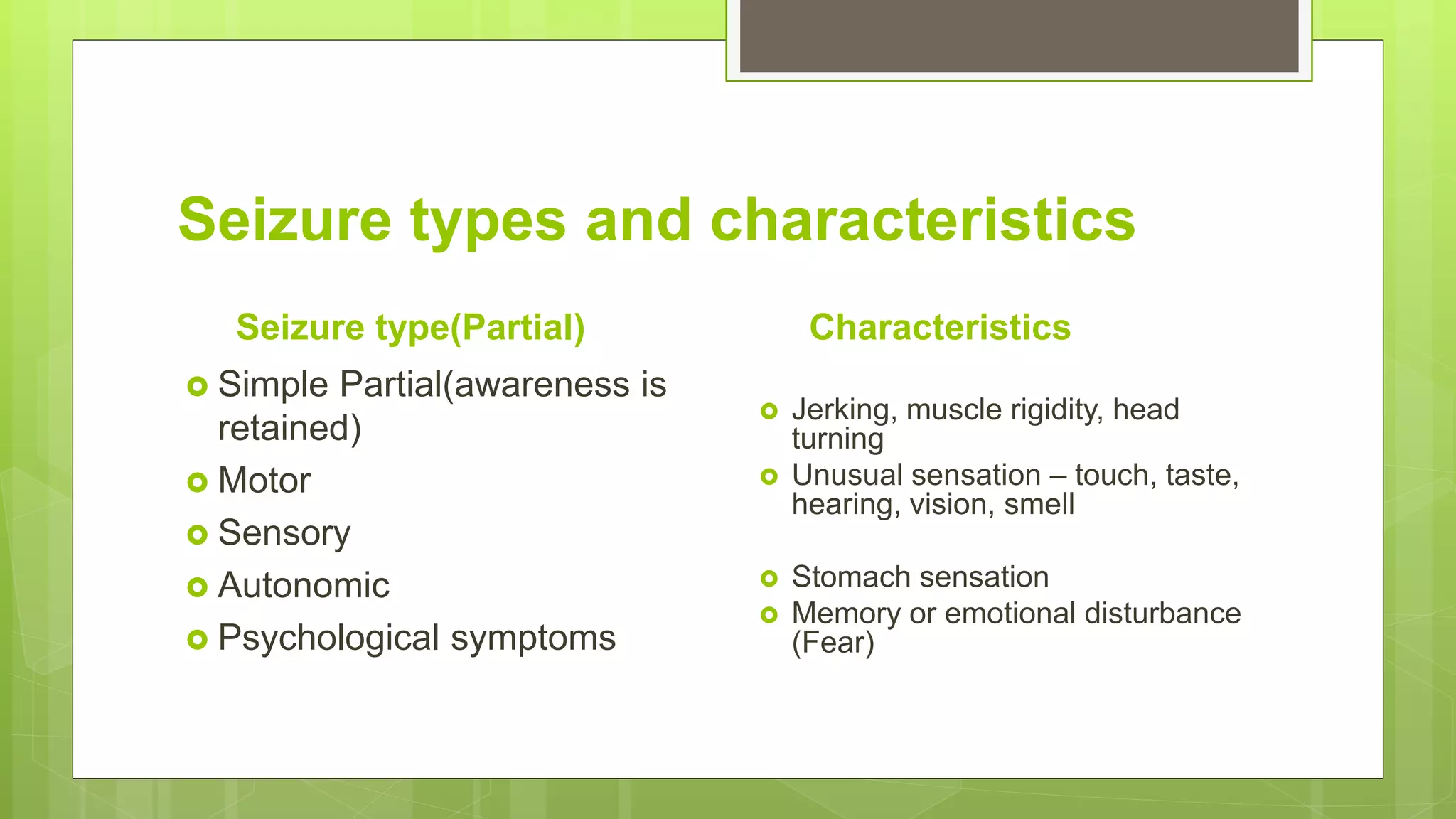
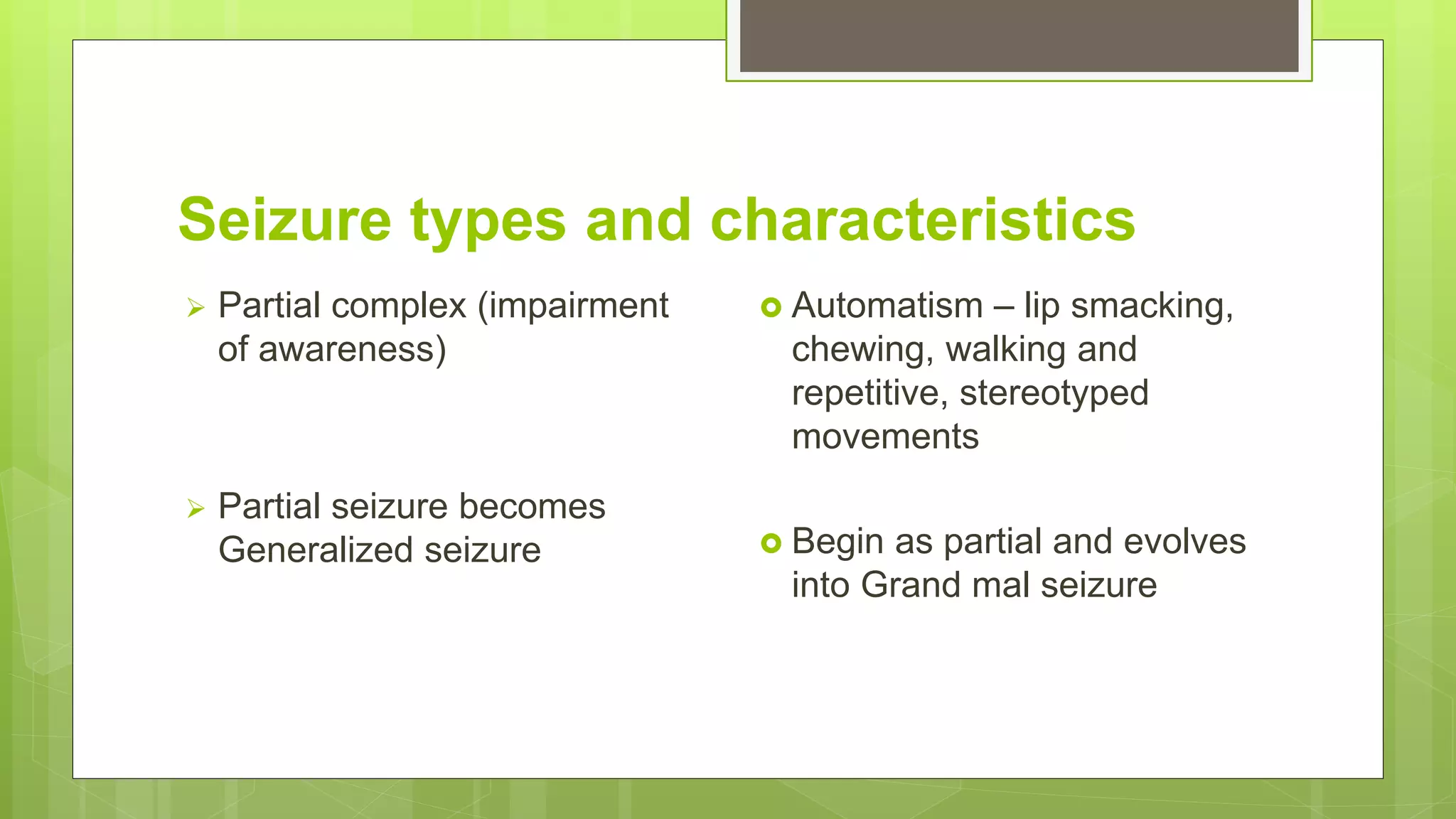
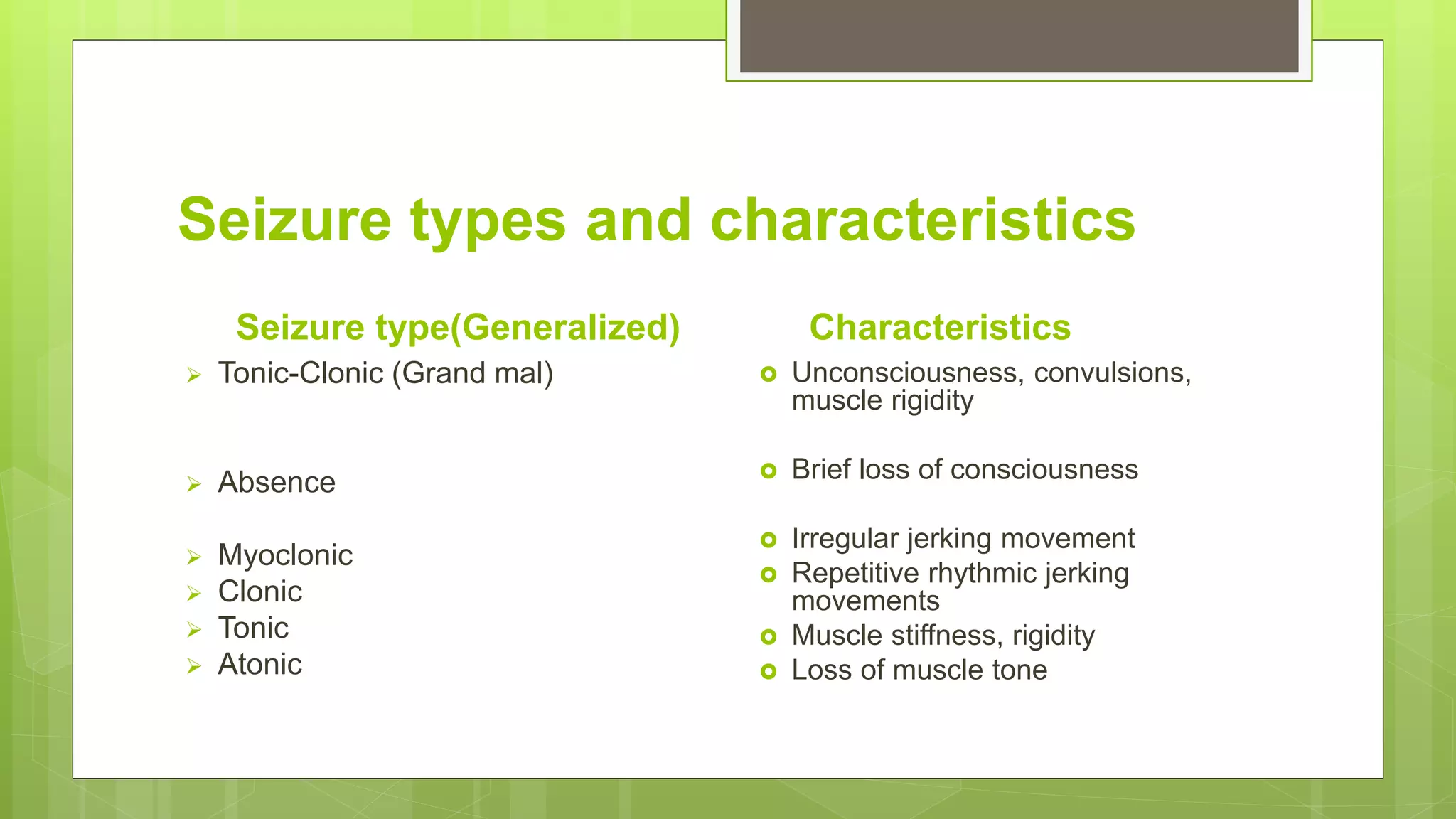
Epilepsy is a chronic neurological disorder characterized by recurrent seizures resulting from abnormal neuronal activity in the brain. It affects around 1% of the population. Seizures can vary from brief periods of lack of awareness to full motor convulsions. The cause is often unknown but may involve excessive glutamate signaling and reduced GABA inhibition in the brain. Epilepsy is usually treated with anti-seizure medications, though in refractory cases surgery may be an option. The goals of treatment are seizure freedom and improved quality of life with minimal side effects.