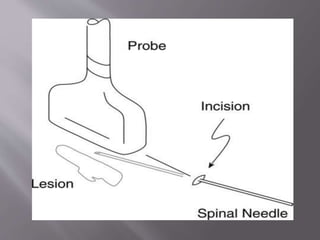
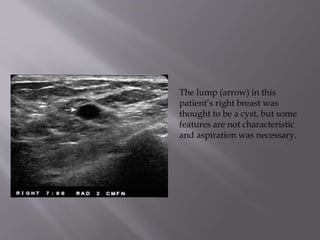
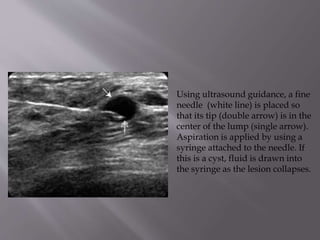
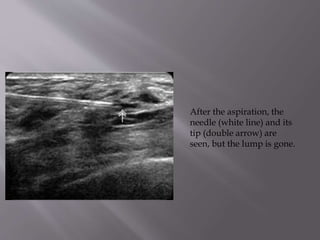
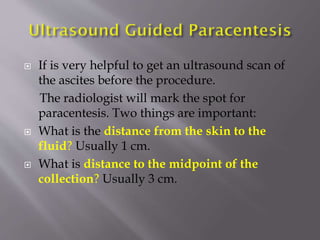
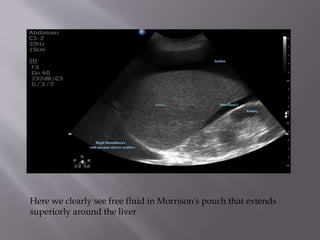
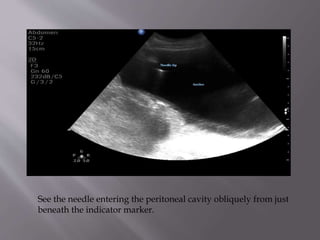
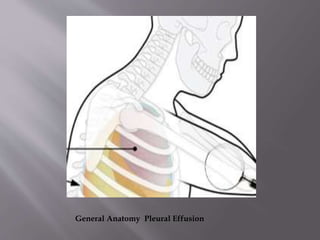
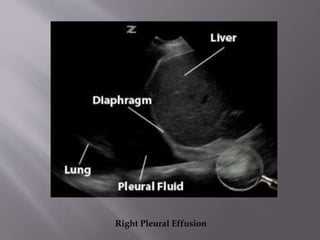
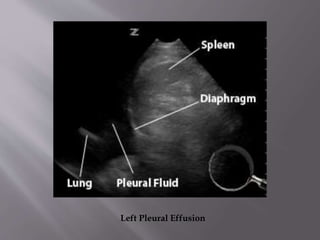
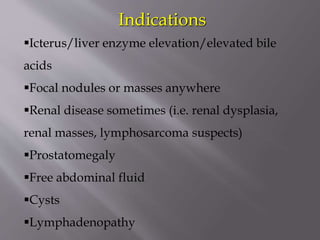
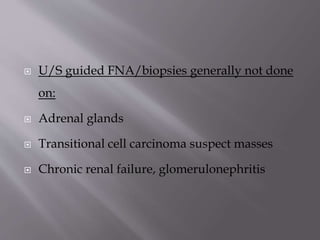
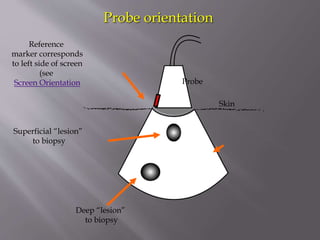
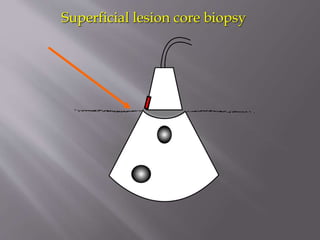
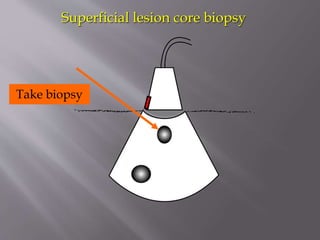
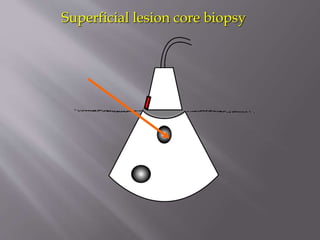
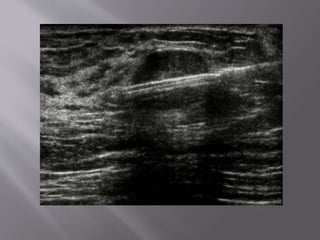
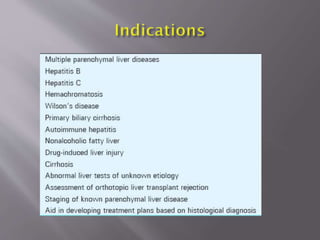
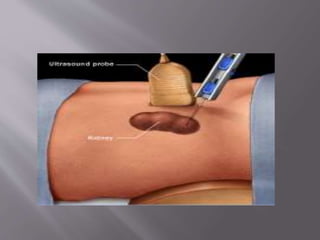
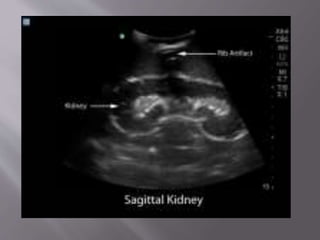
This document provides information on various radiology procedures including aspirations, drainages, and biopsies. It describes how cyst aspirations are performed using ultrasound guidance to insert a needle and drain fluid from cysts in the breast or elsewhere. It also discusses paracentesis for draining ascites and thoracocentesis for draining pleural effusions. The document outlines patient positioning and technical steps for each procedure. Biopsy procedures are also summarized, including how ultrasound is used to precisely guide needle placement and obtain tissue samples from organs like the liver and kidneys.