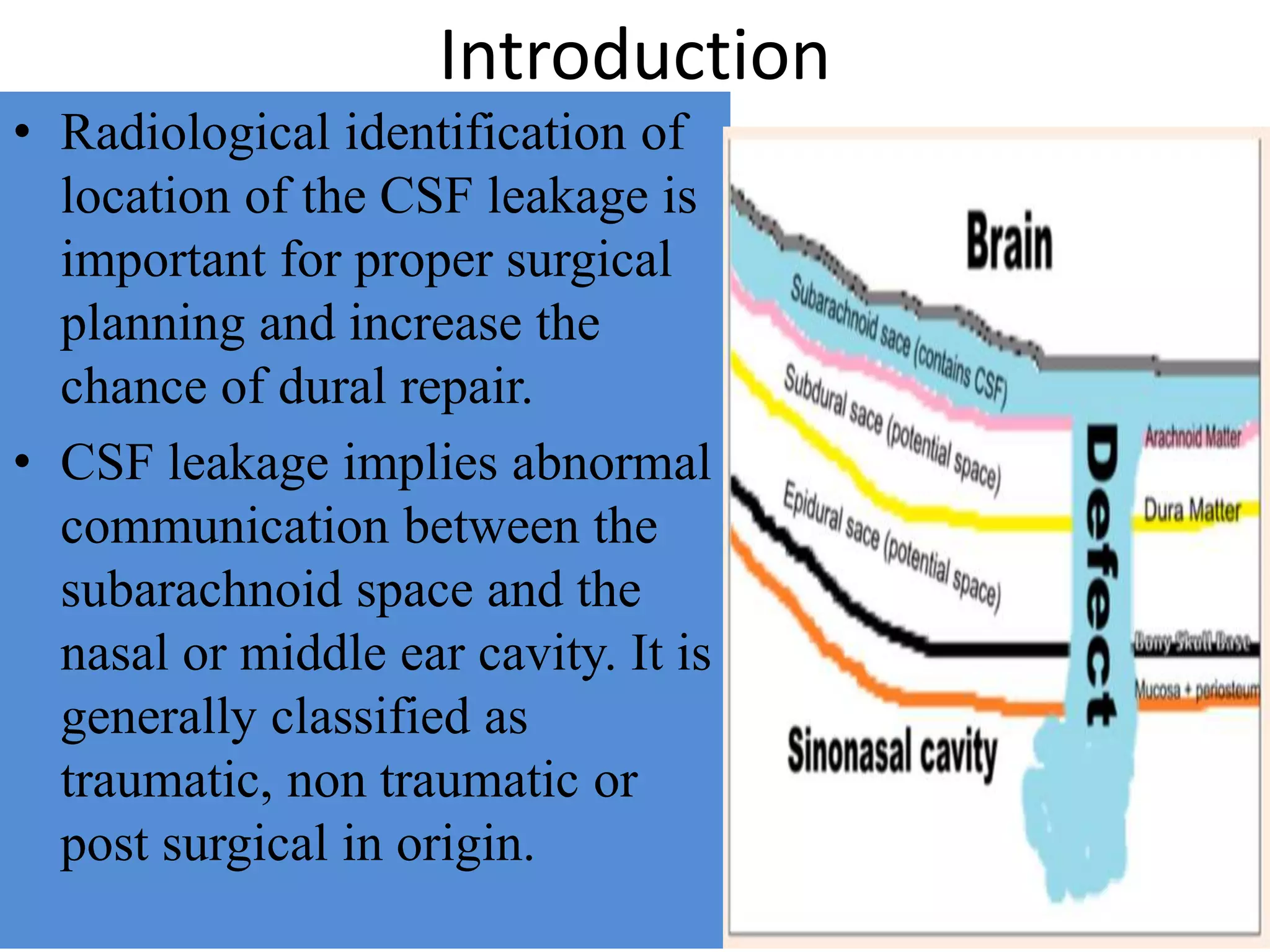
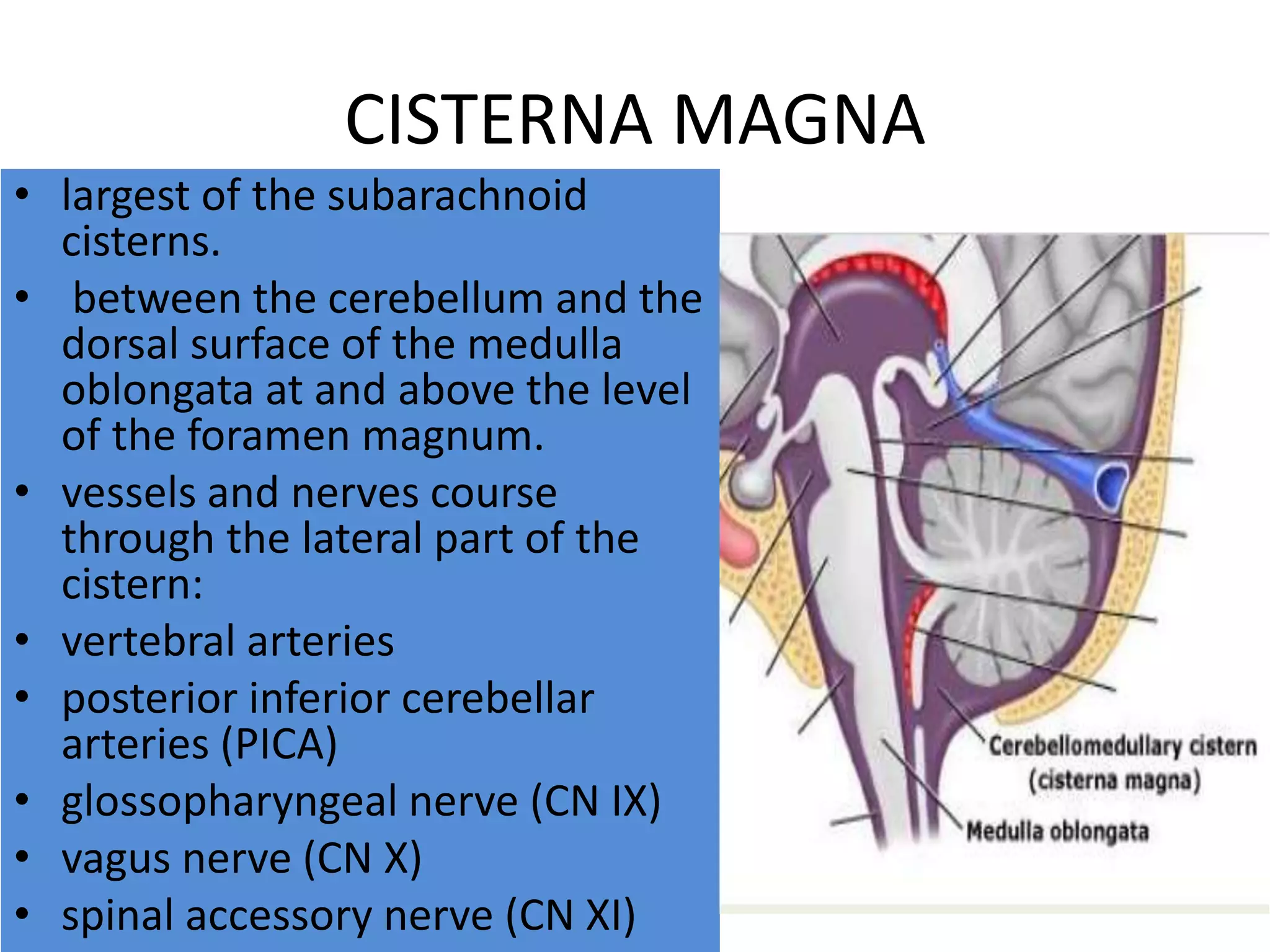
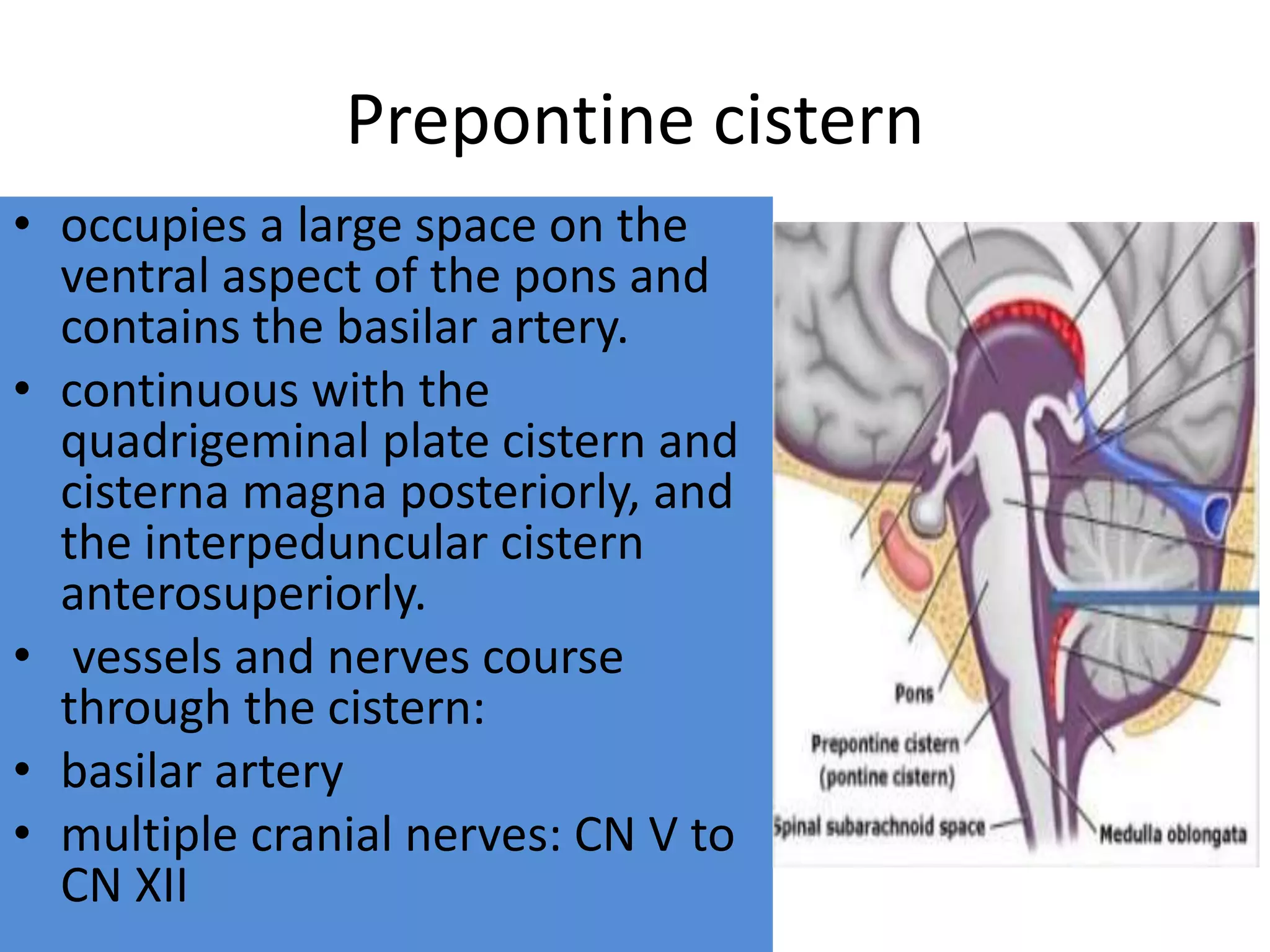
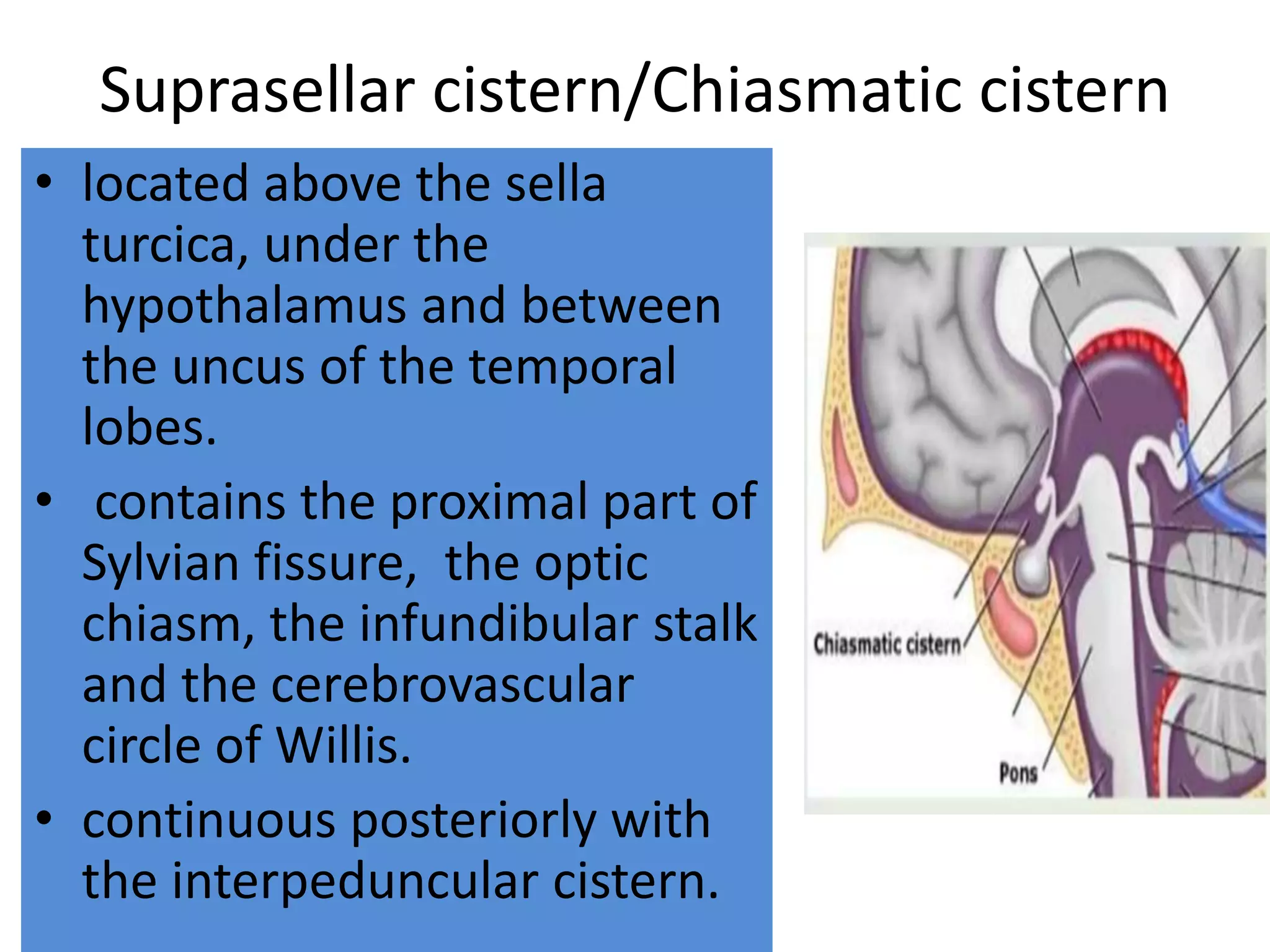
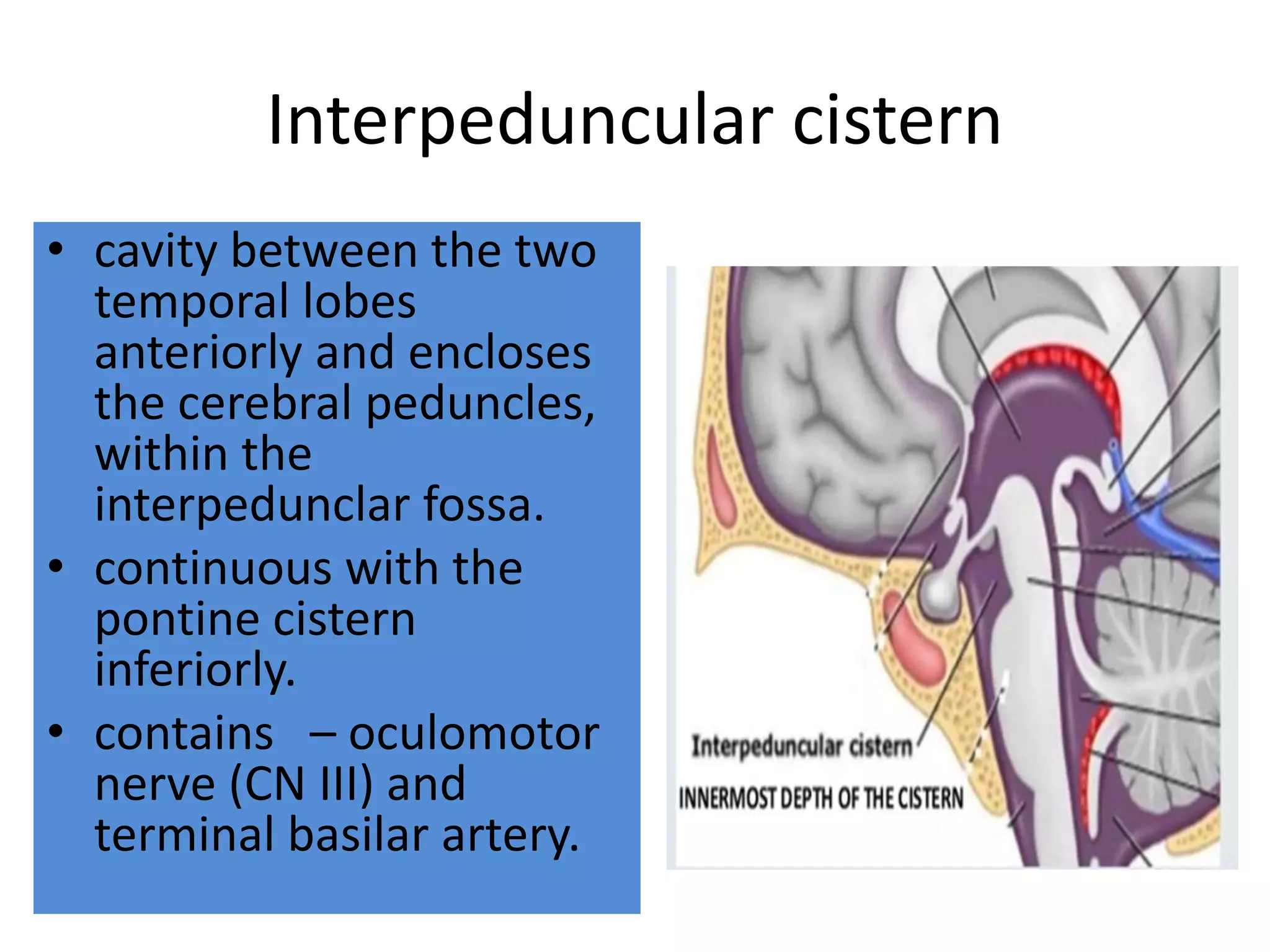
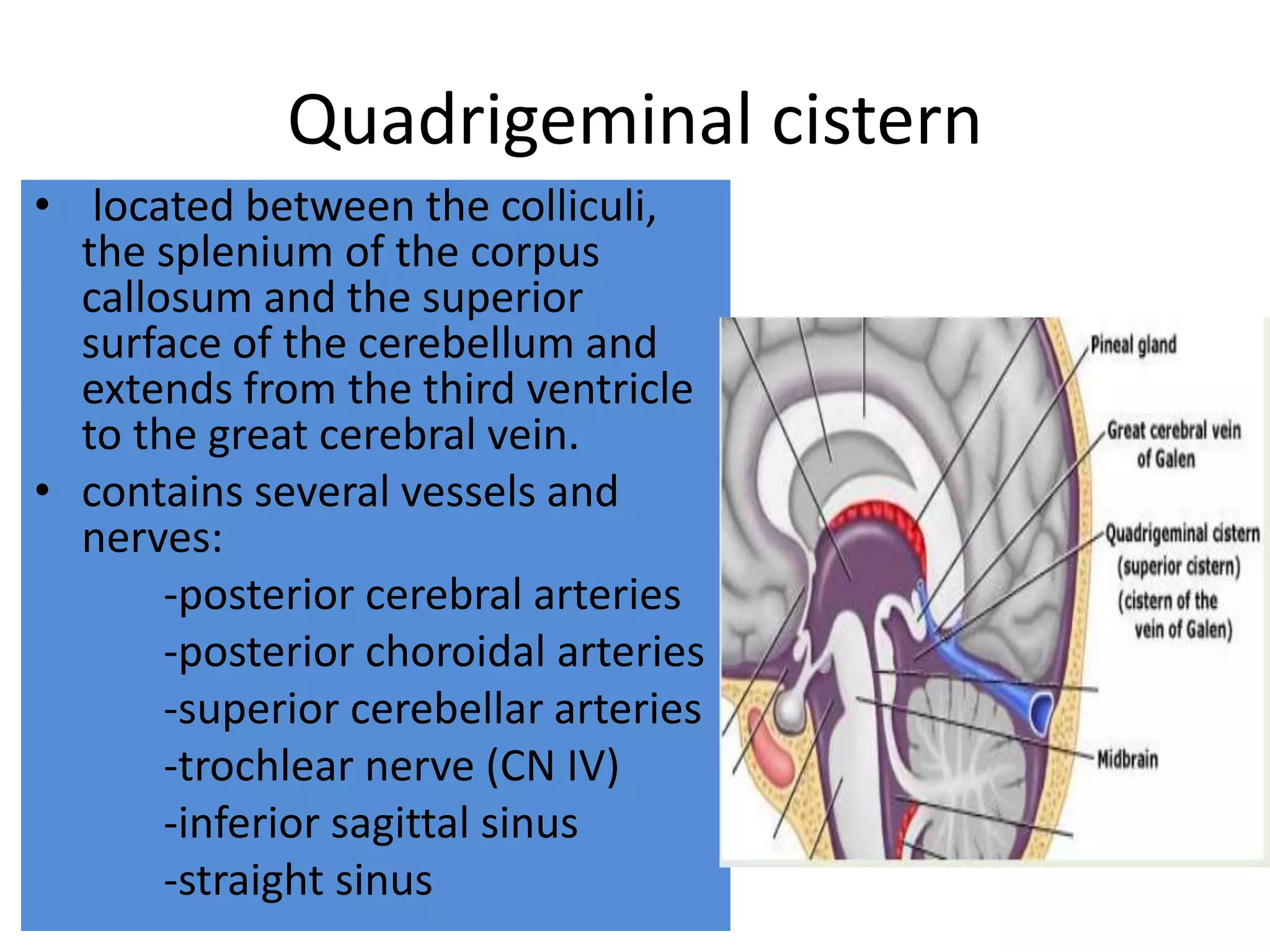
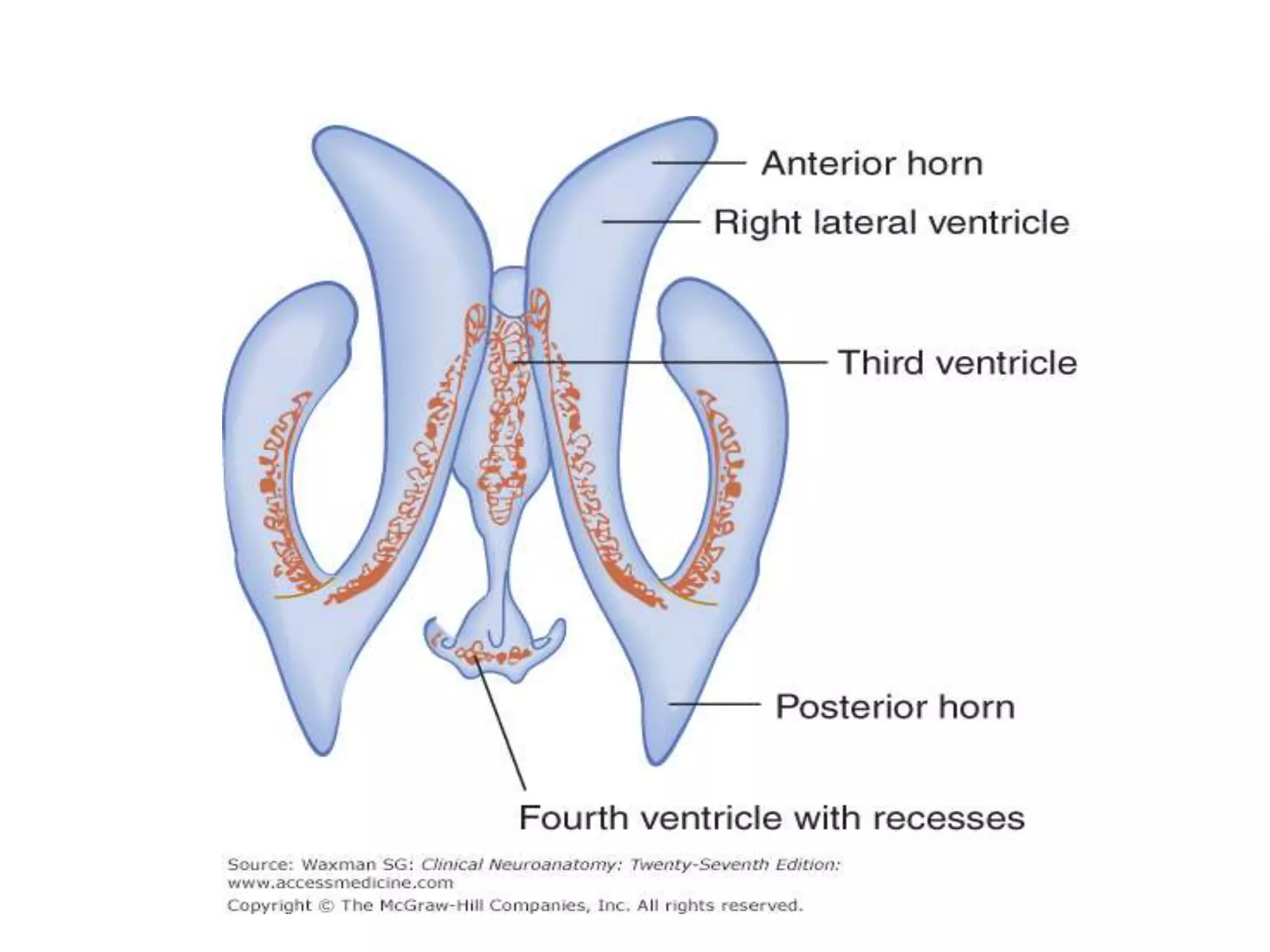
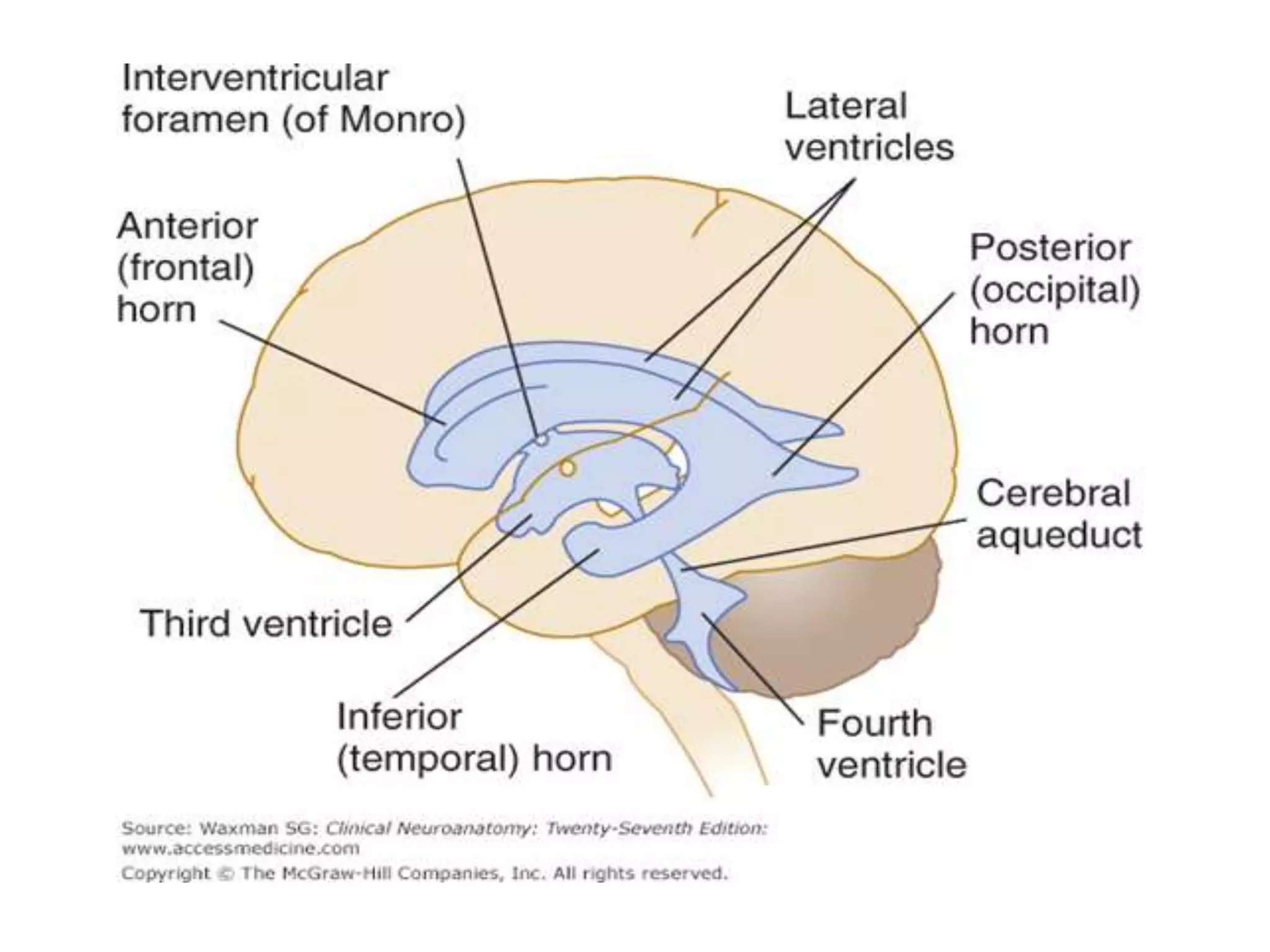
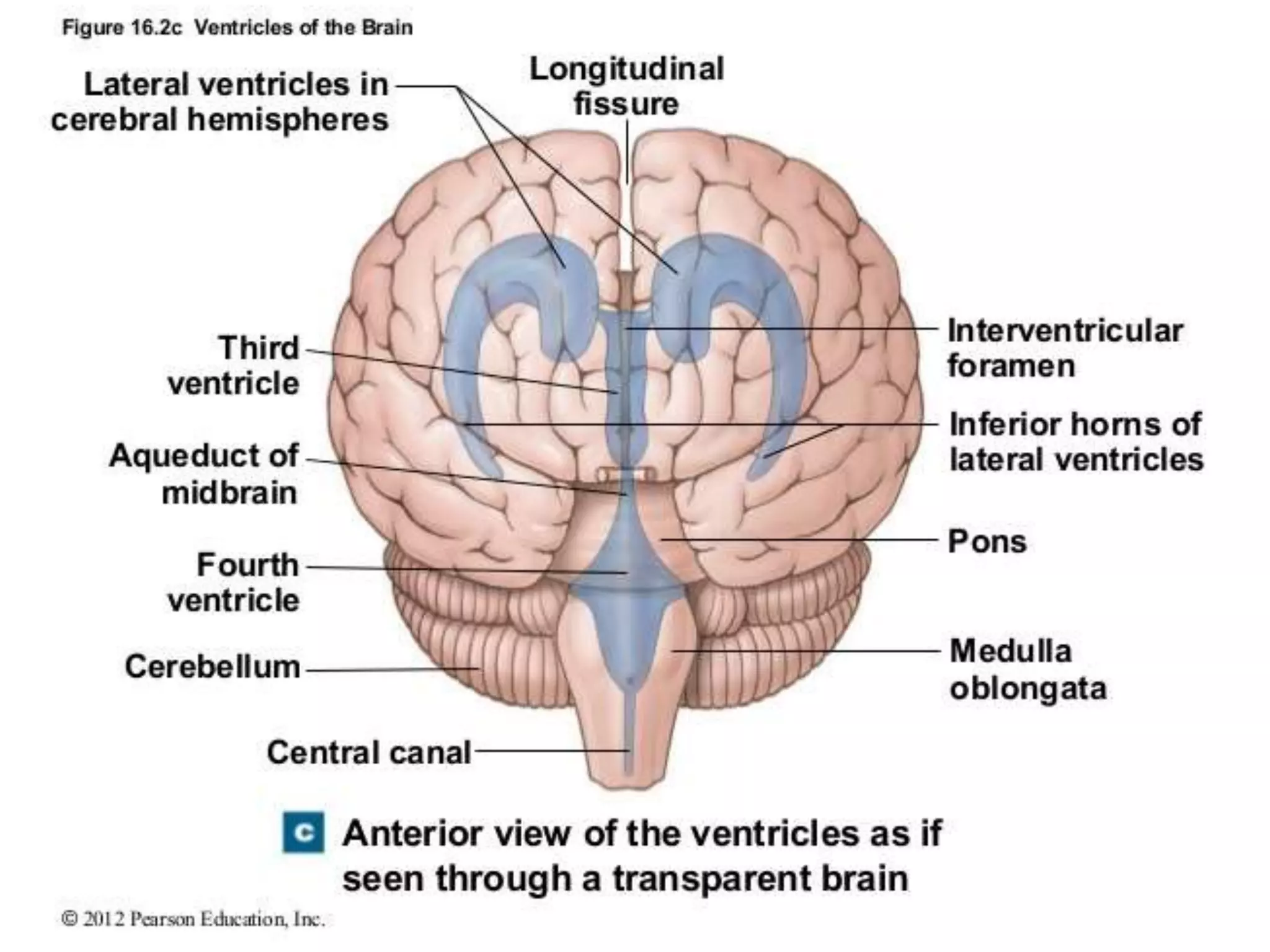
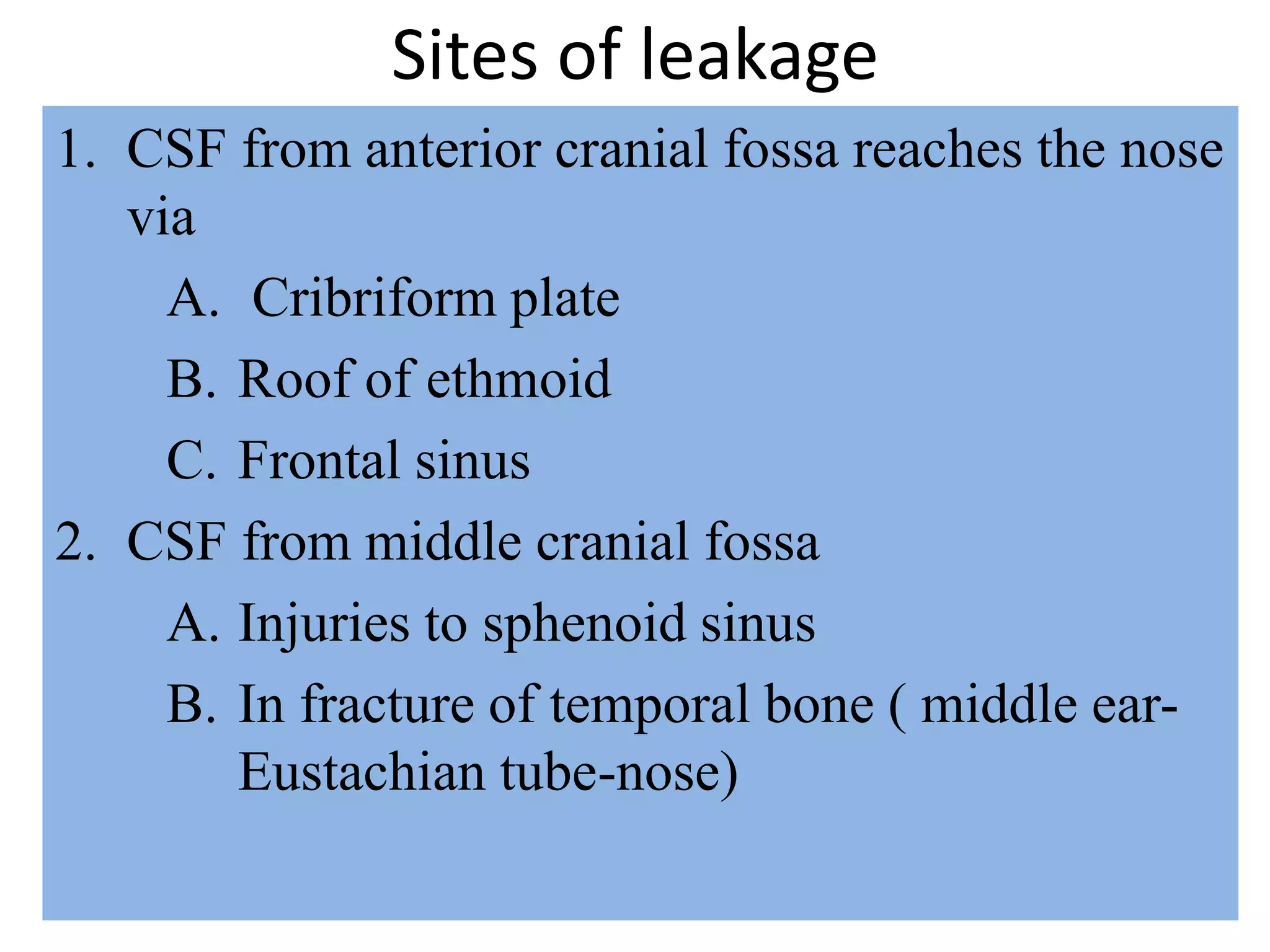
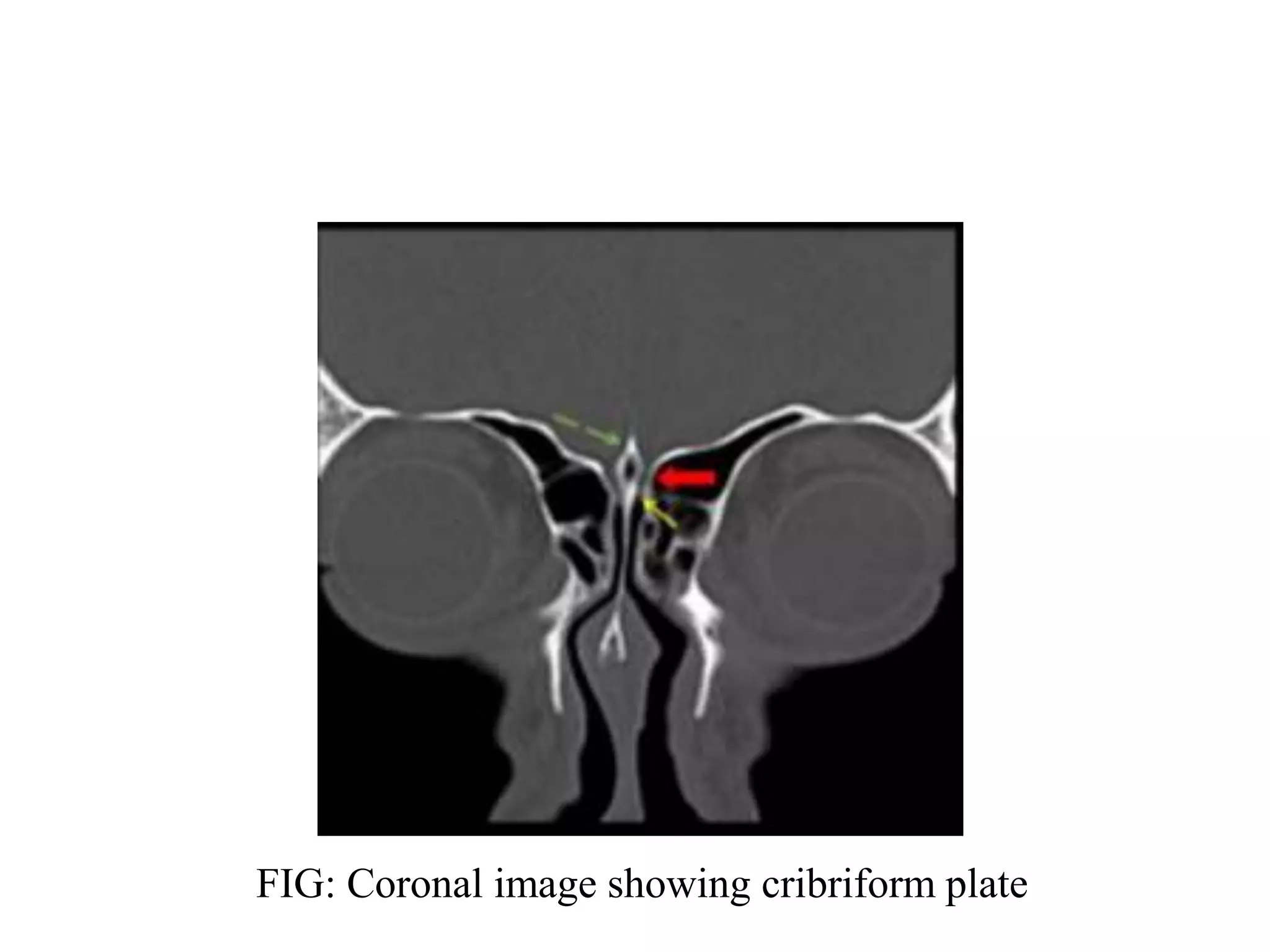
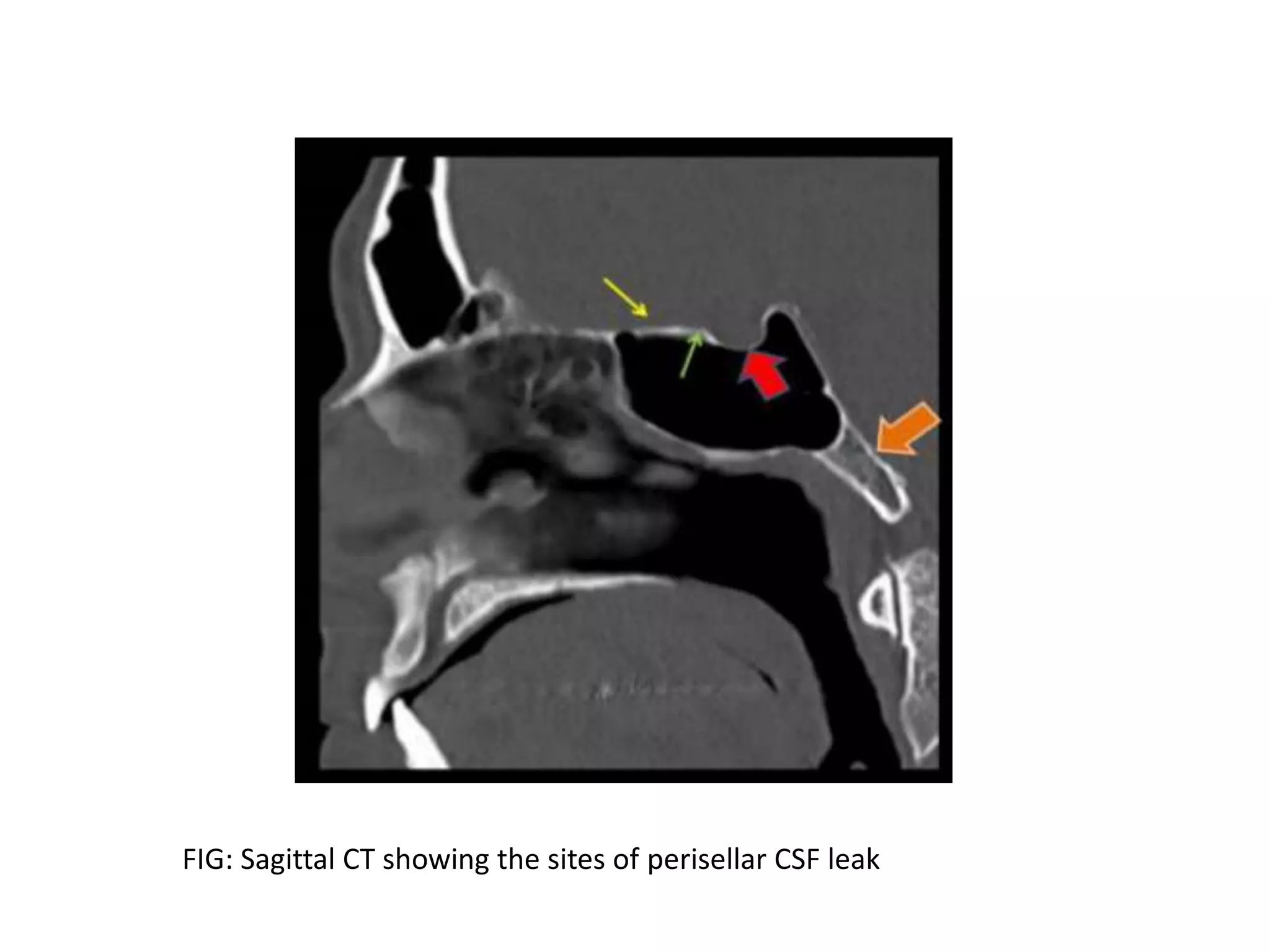
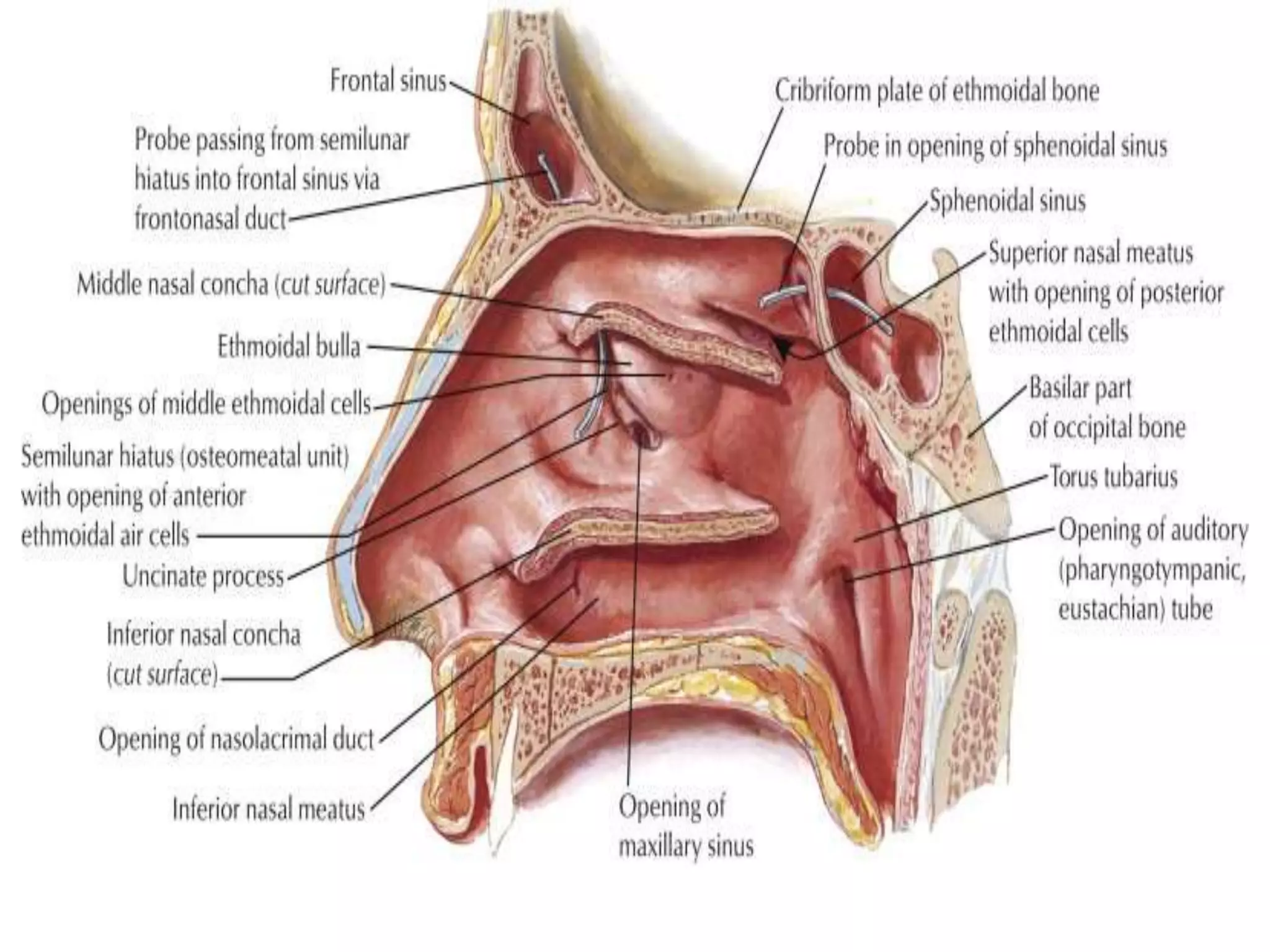
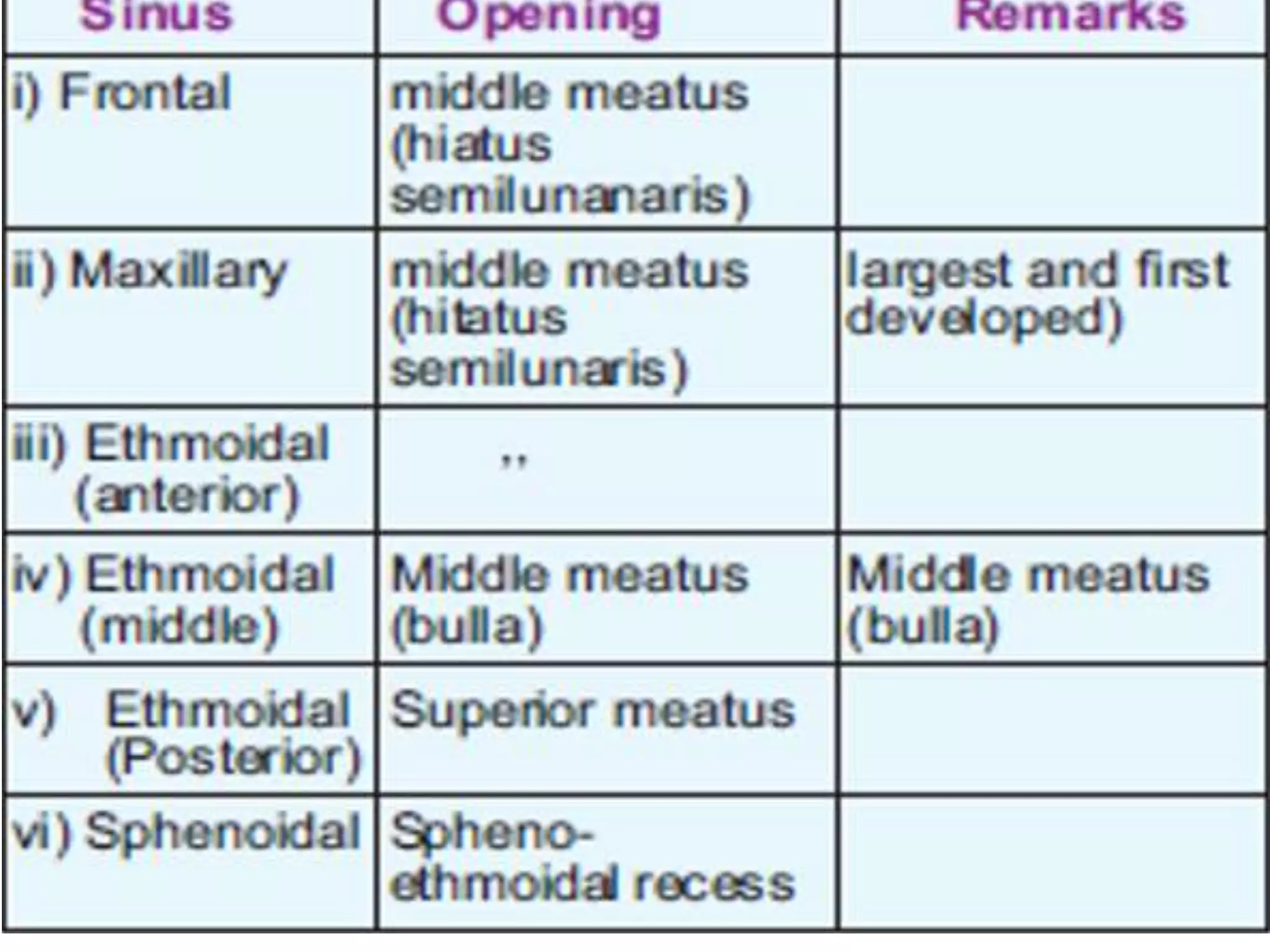
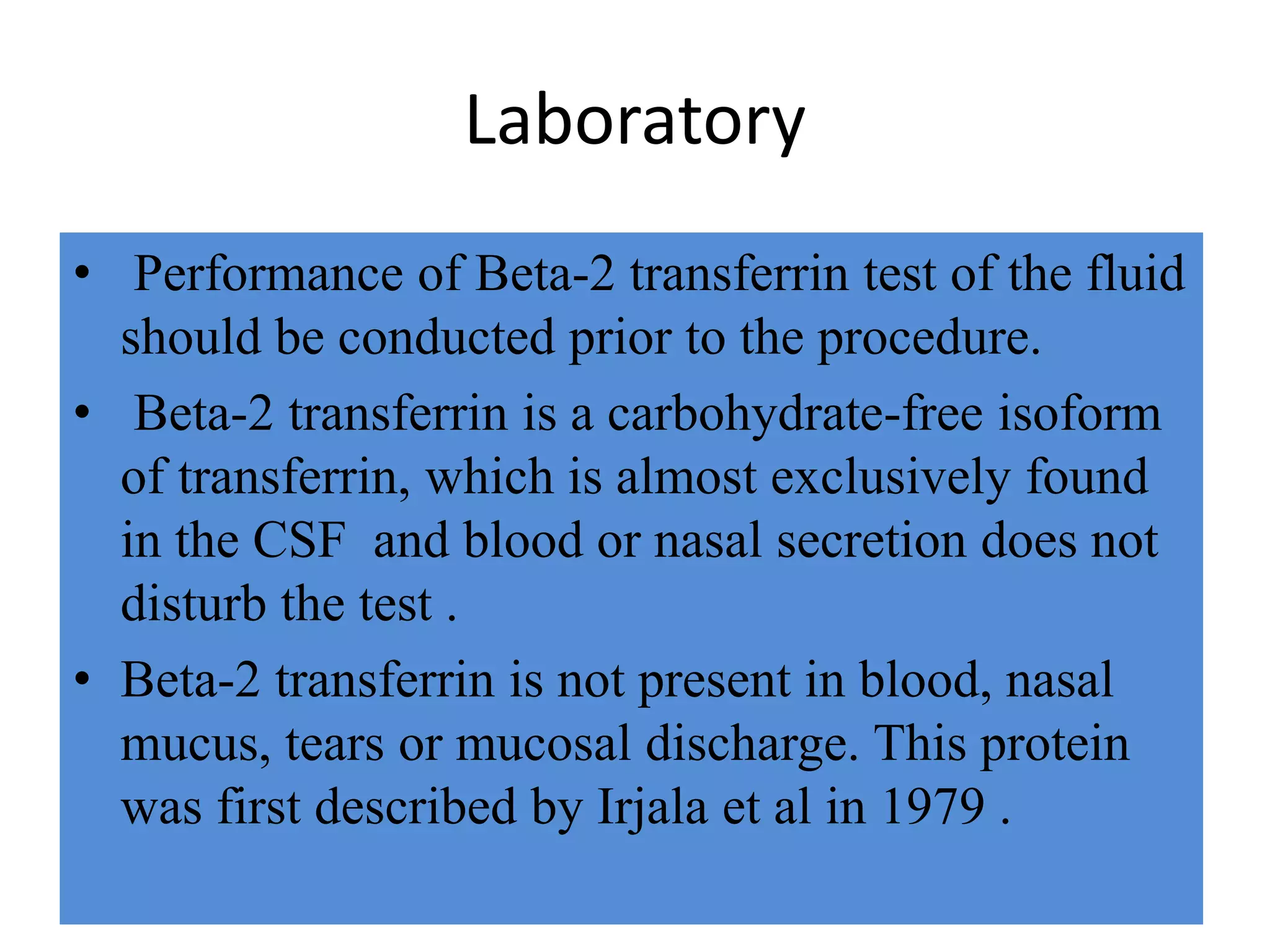
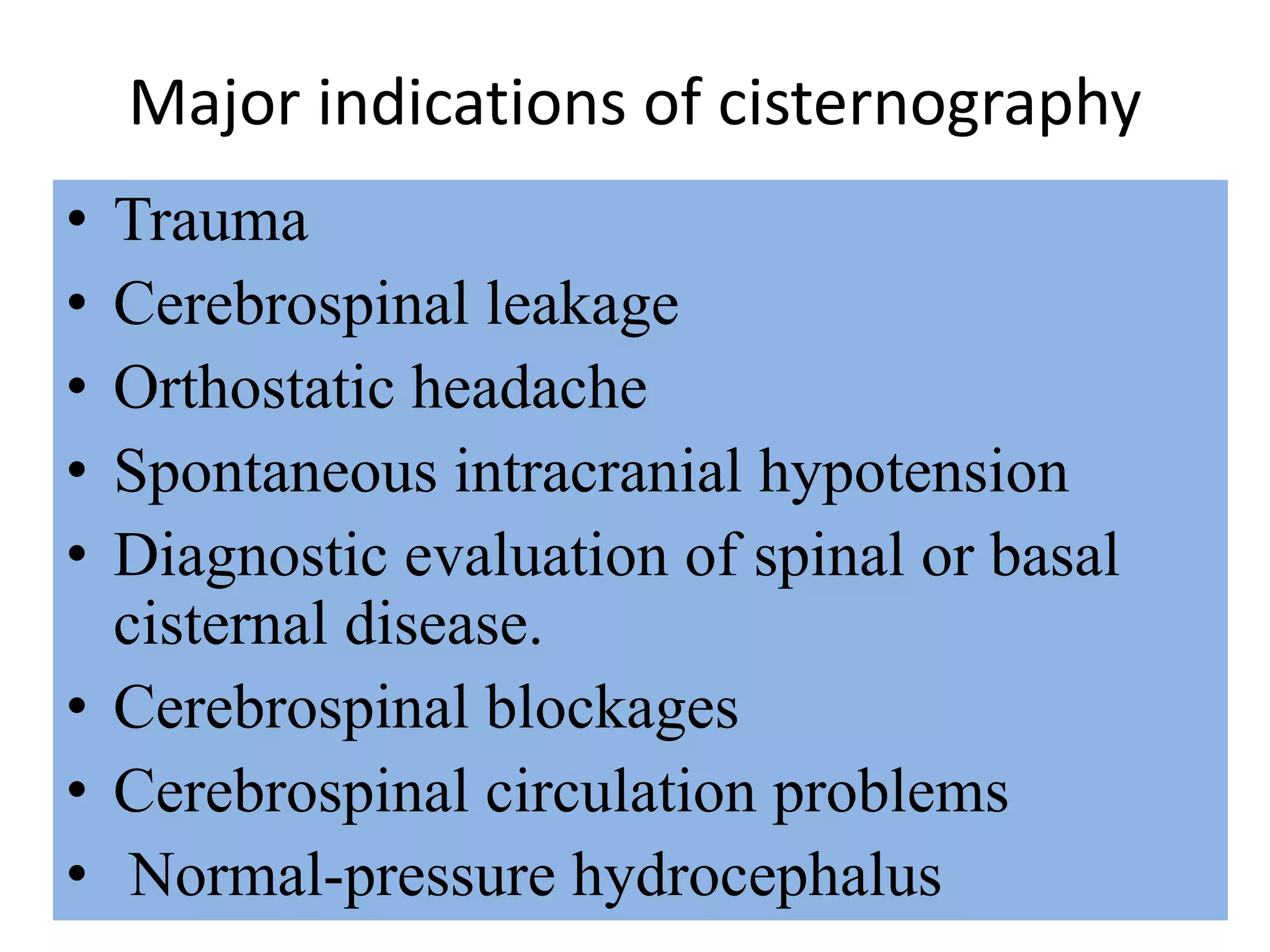
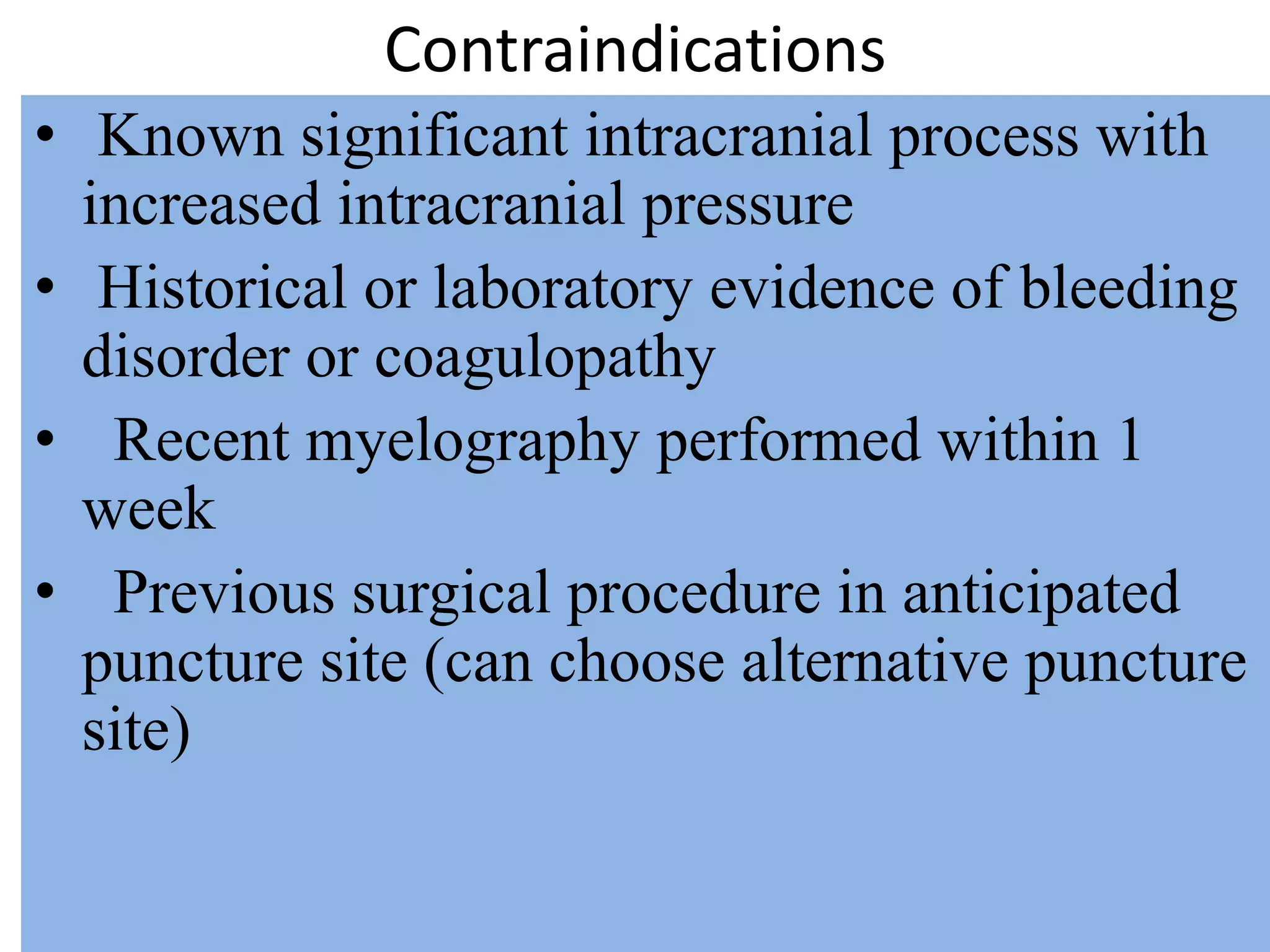
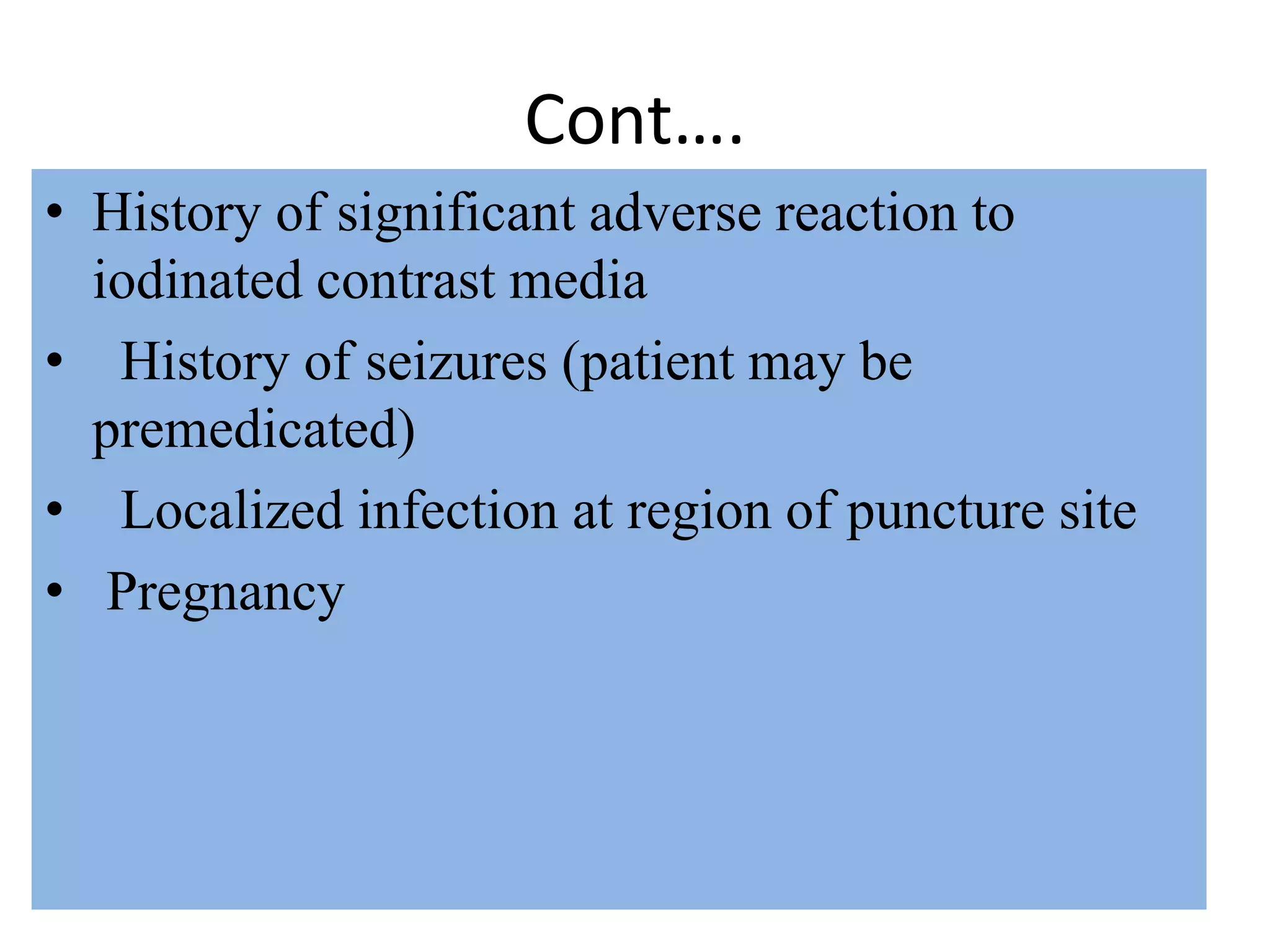
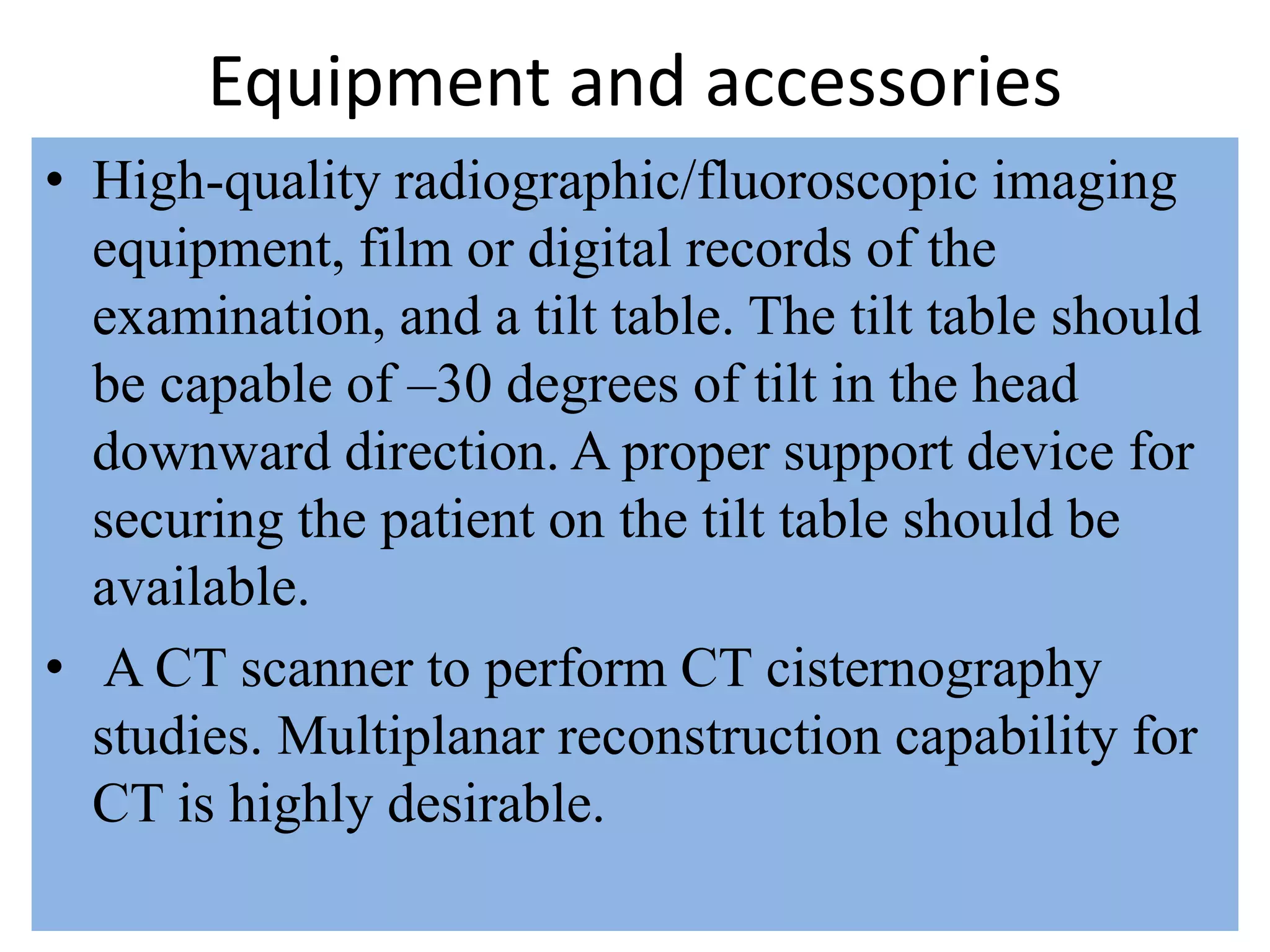
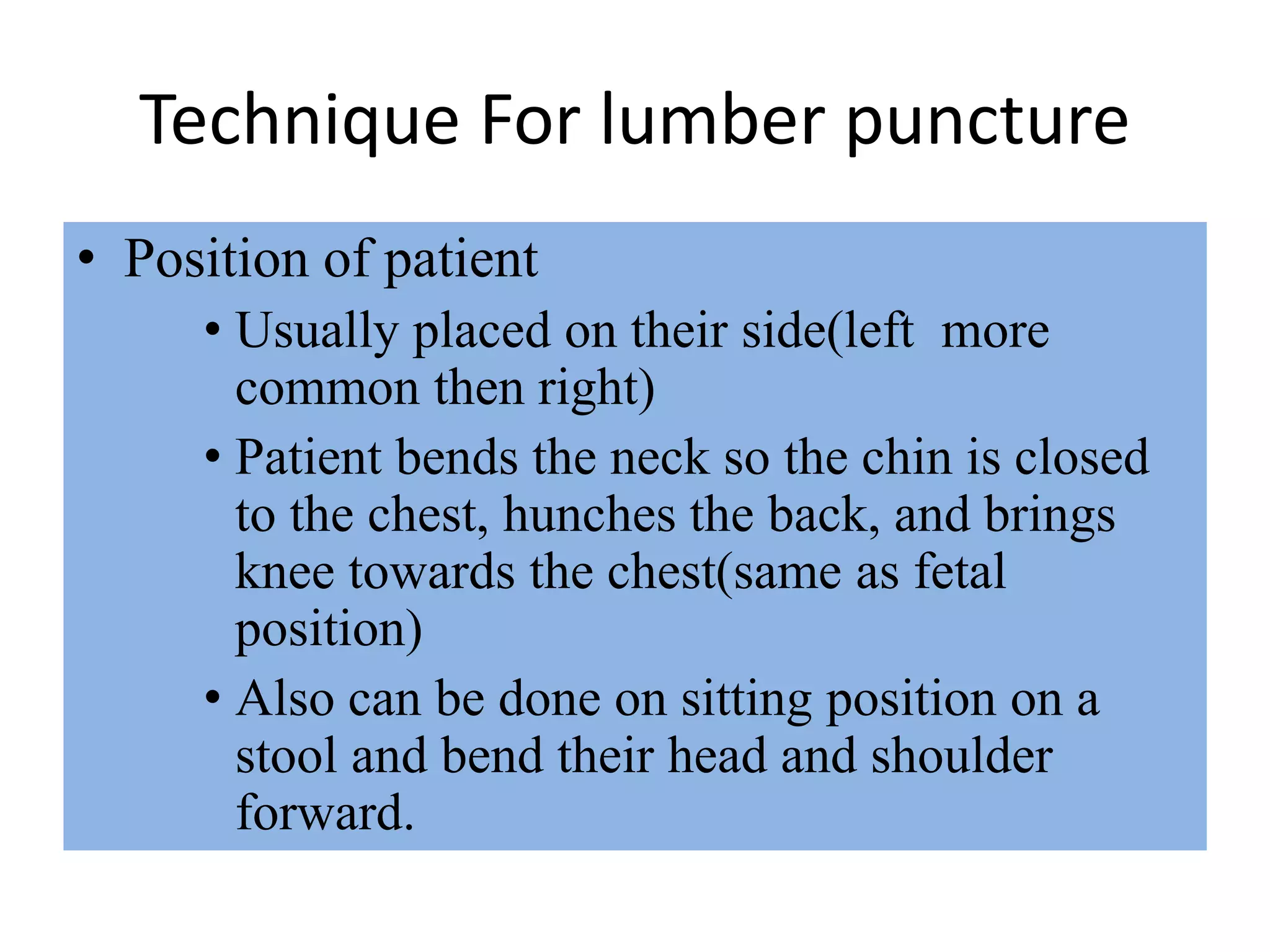
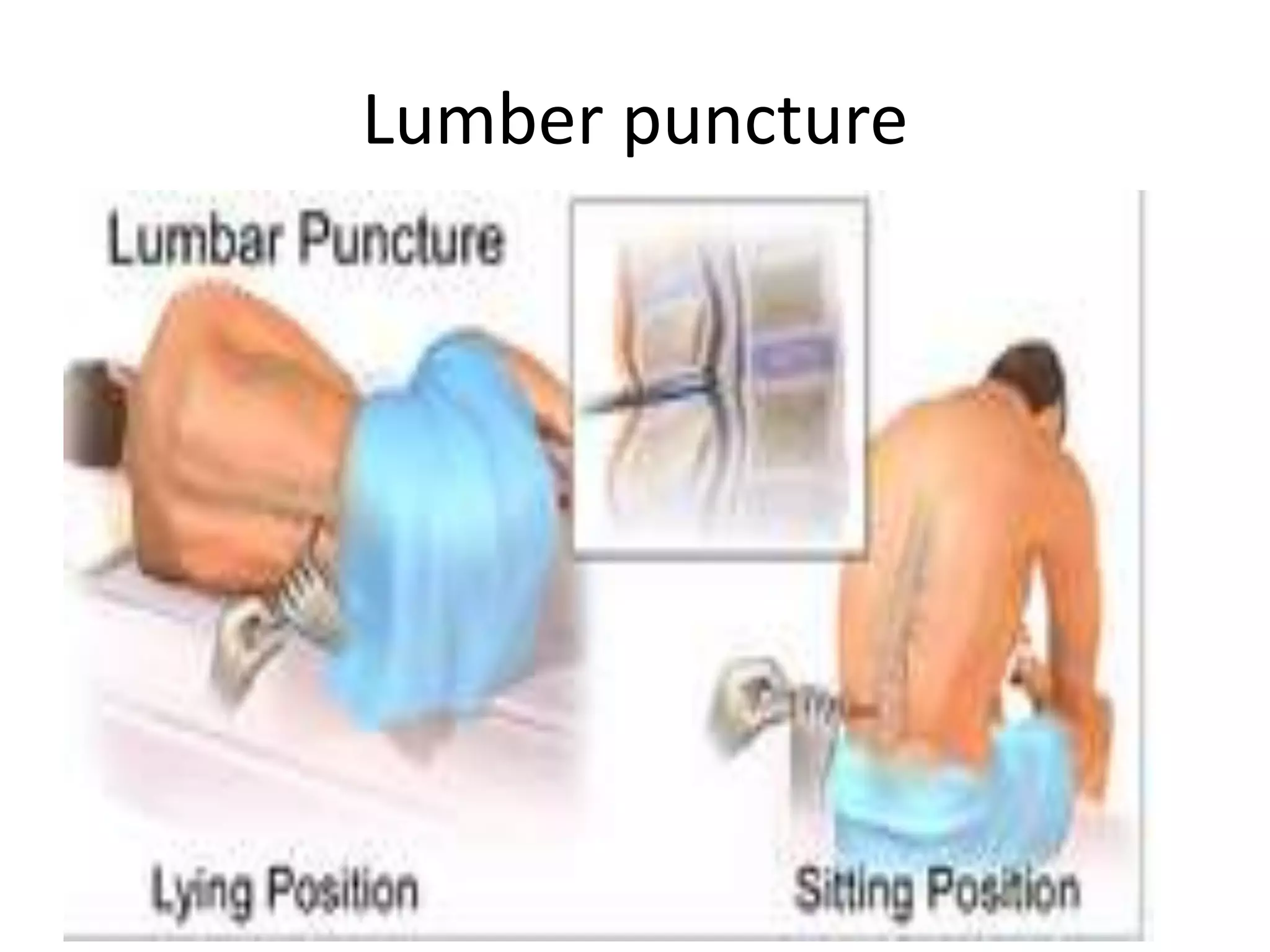
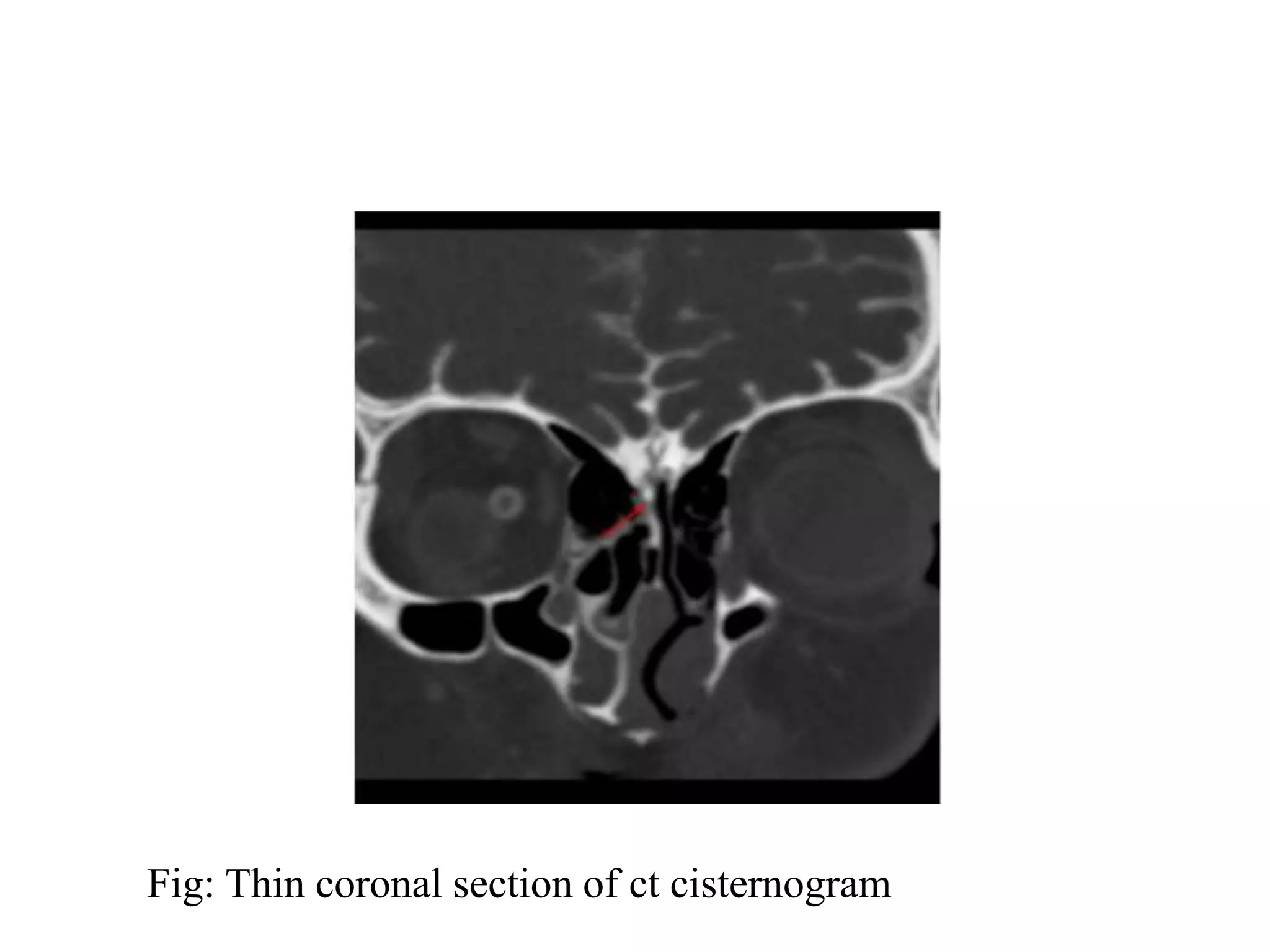
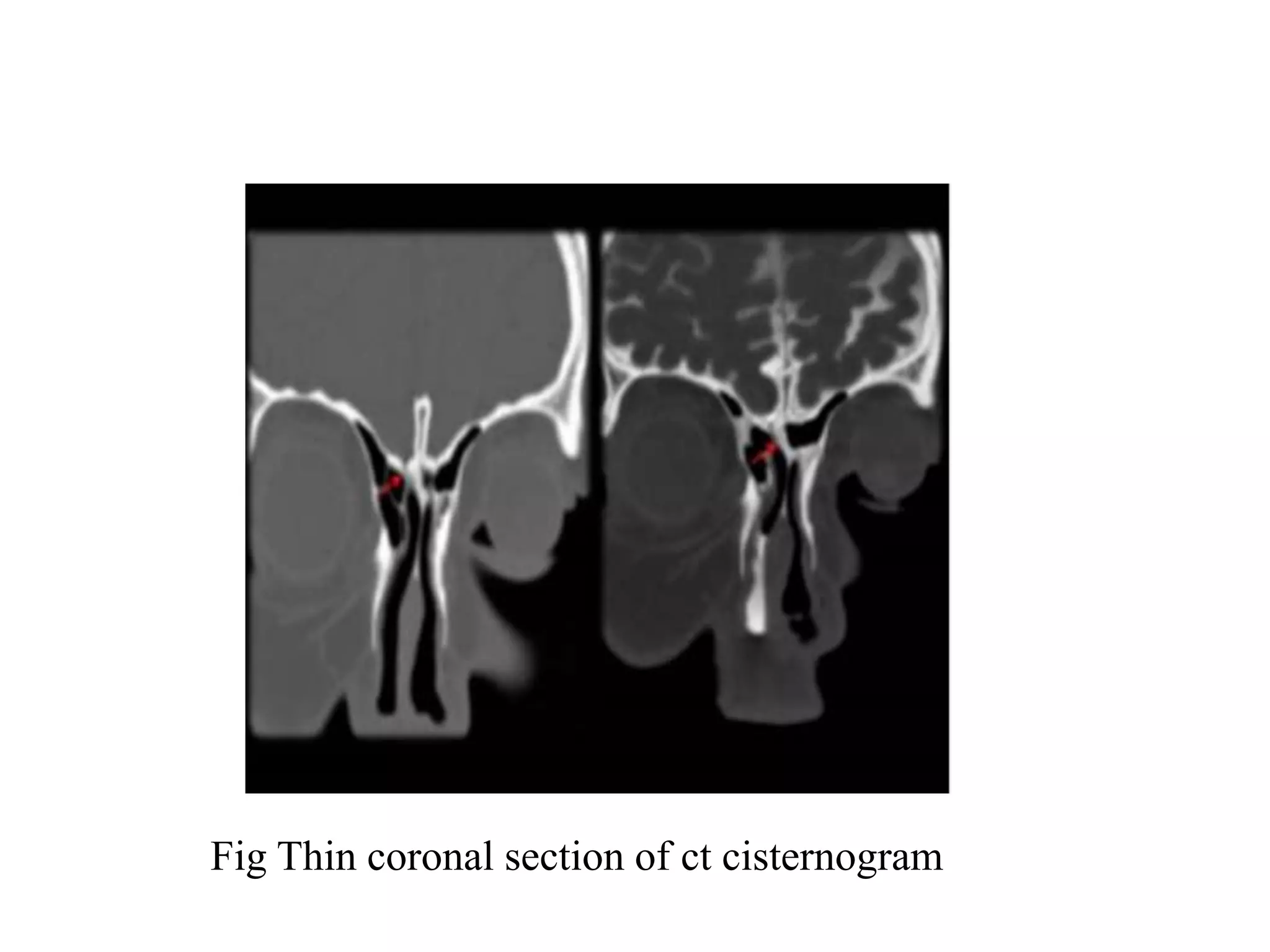
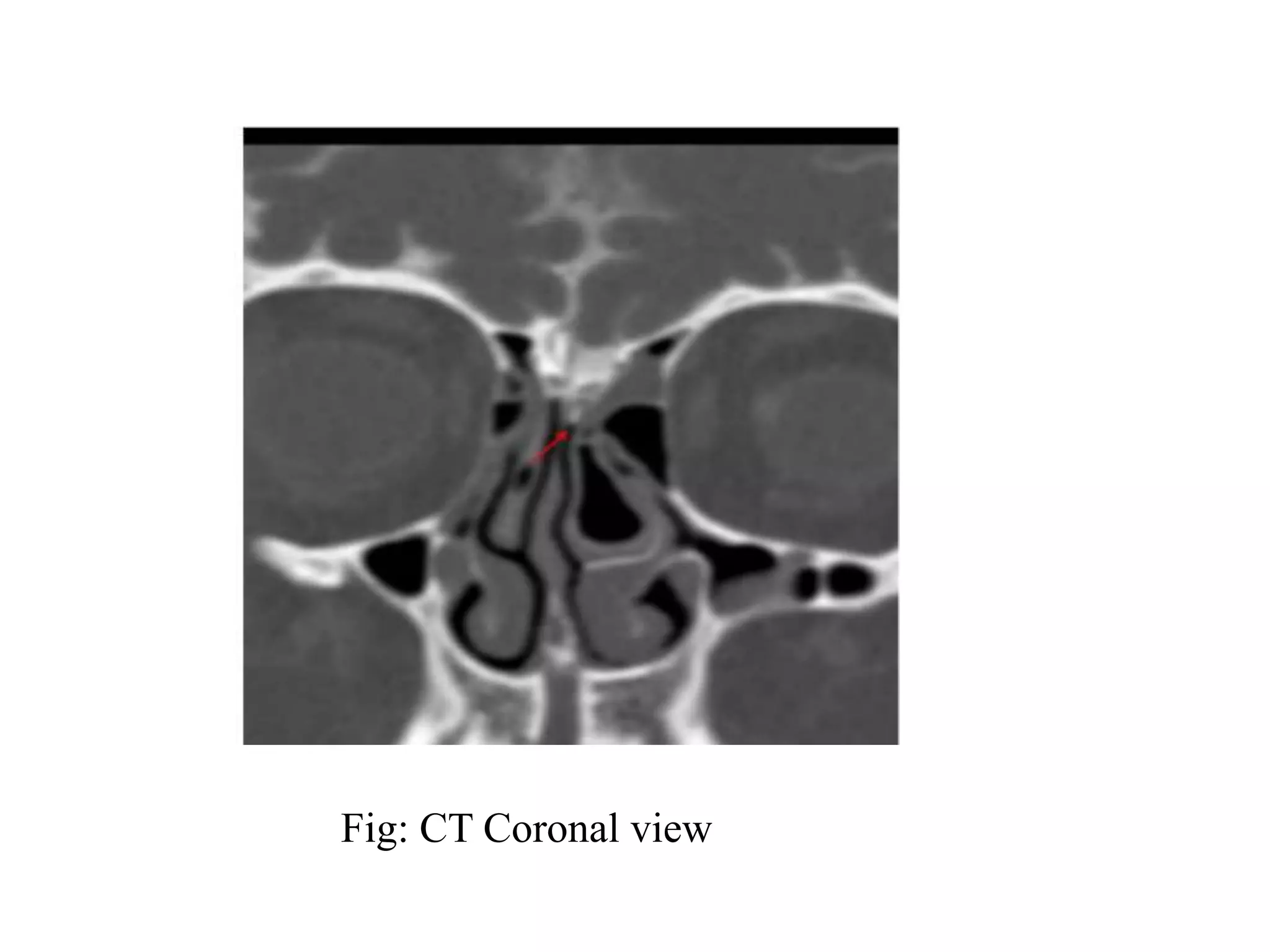
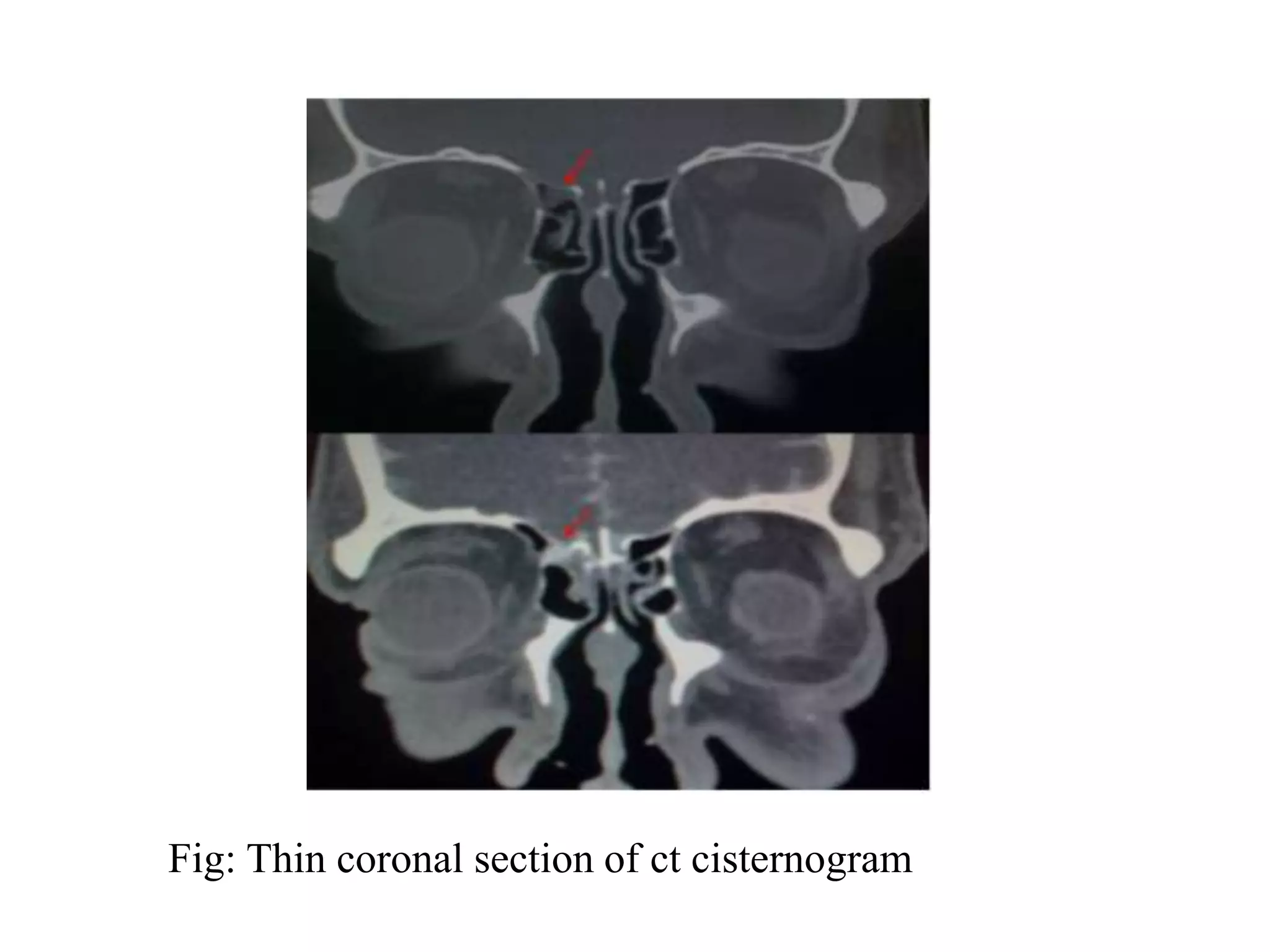
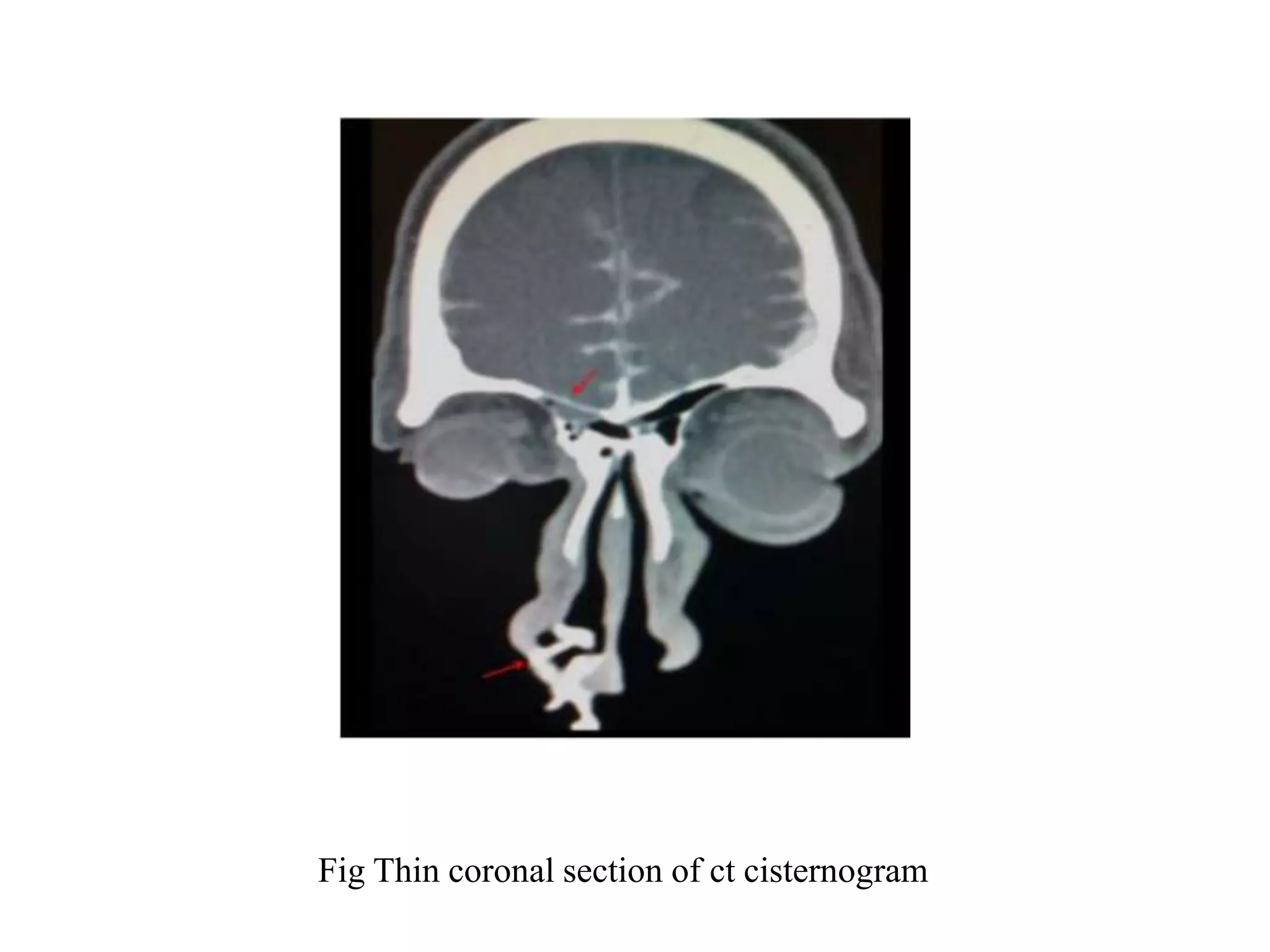
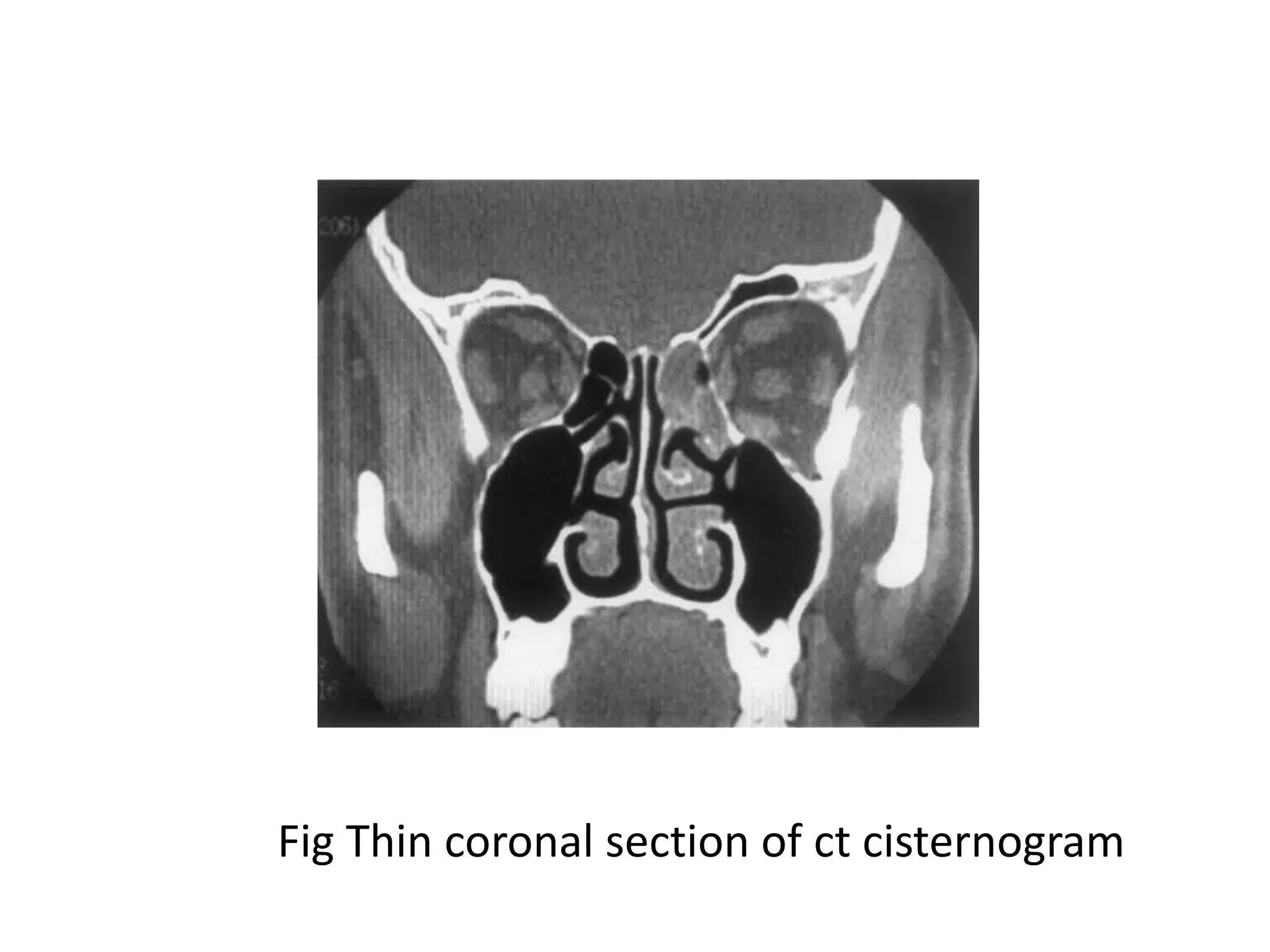
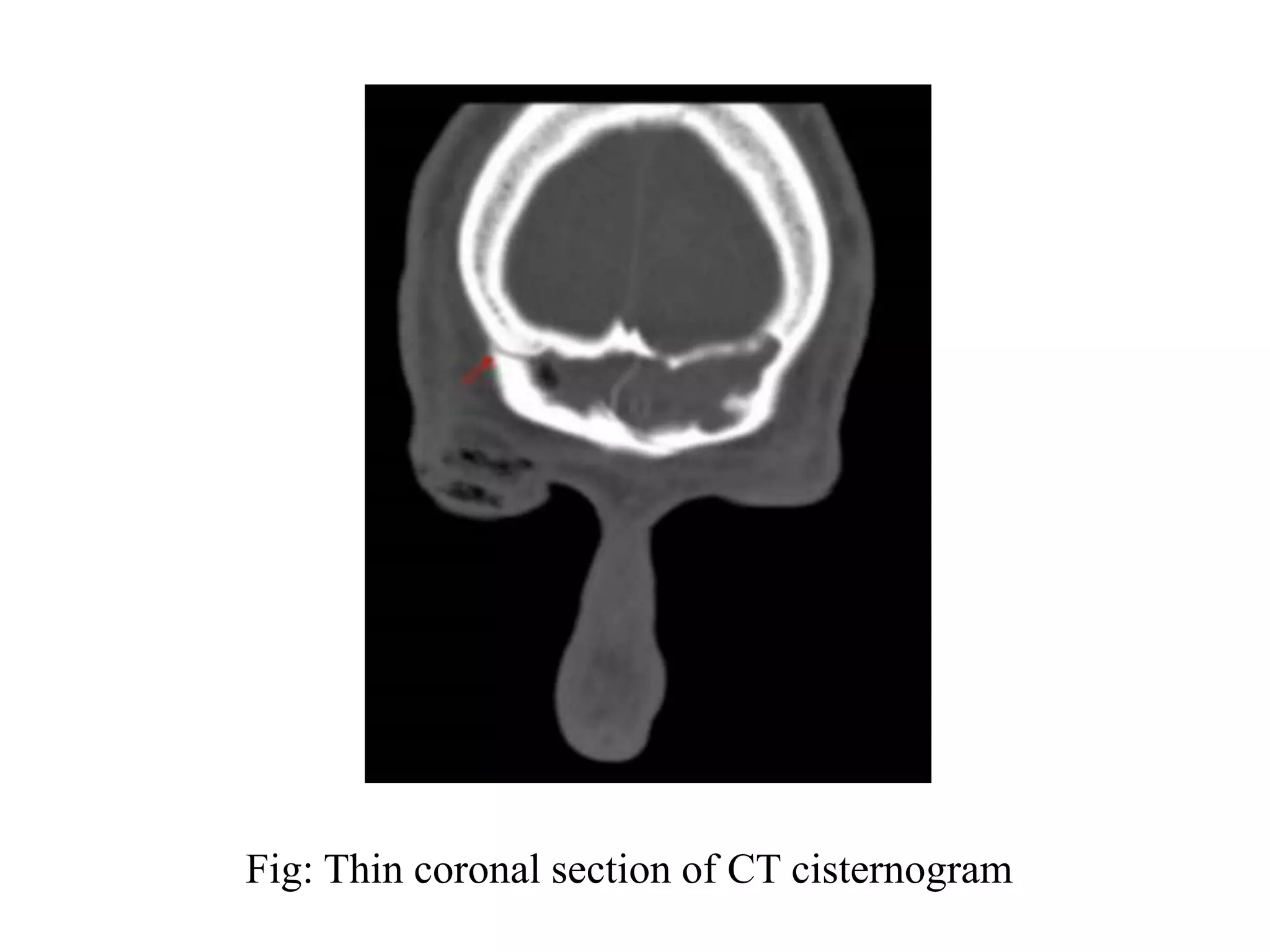
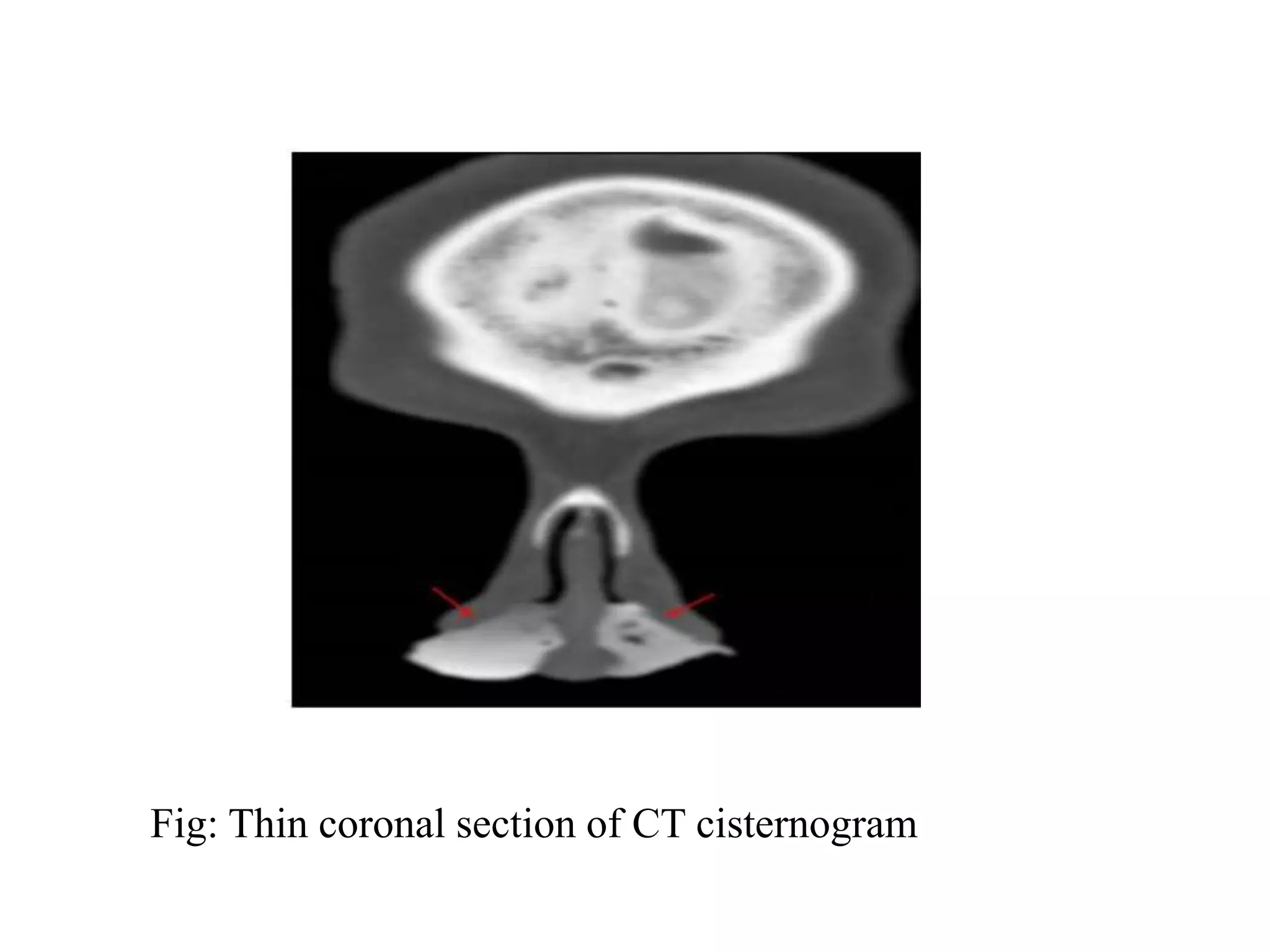
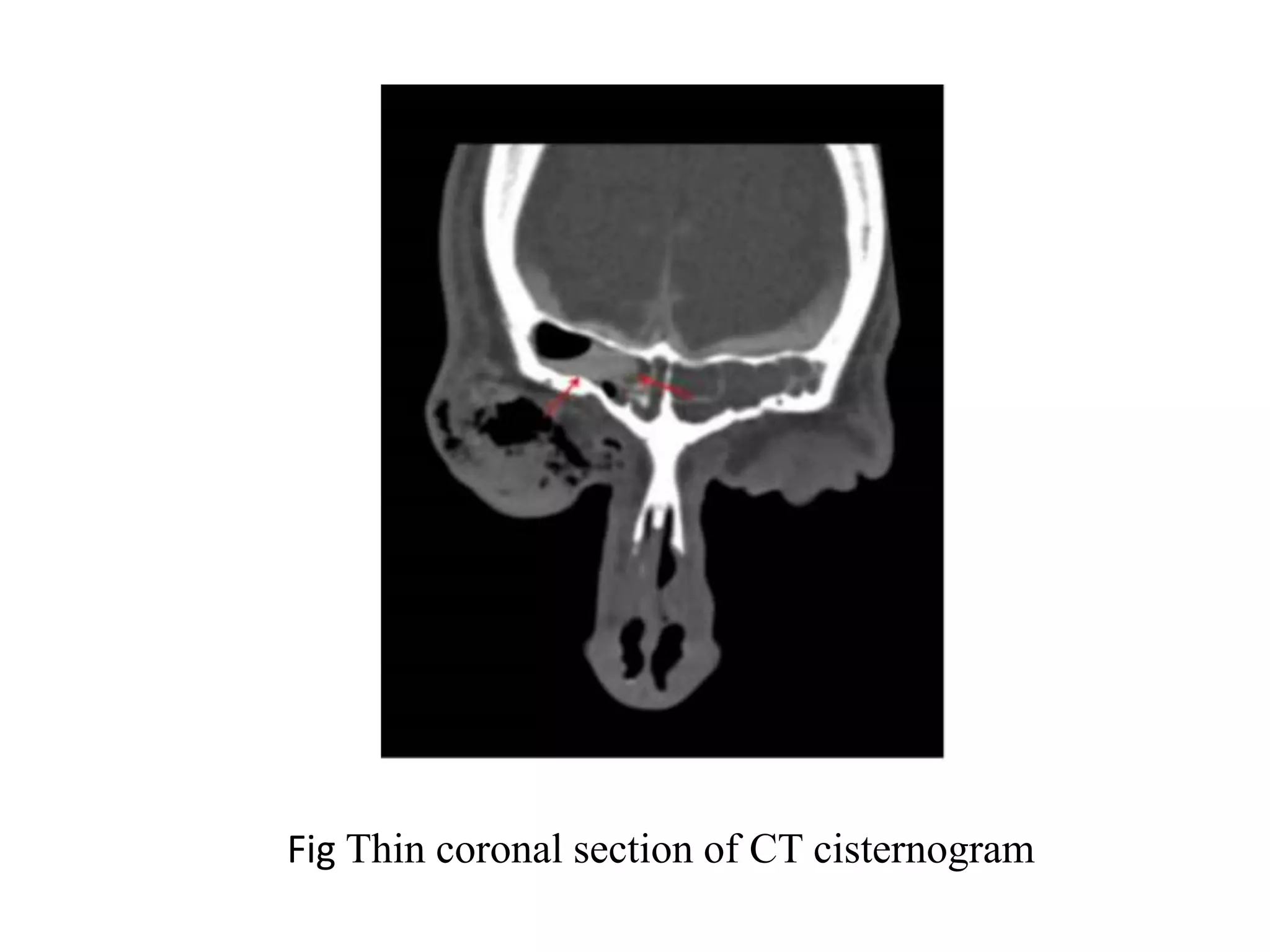
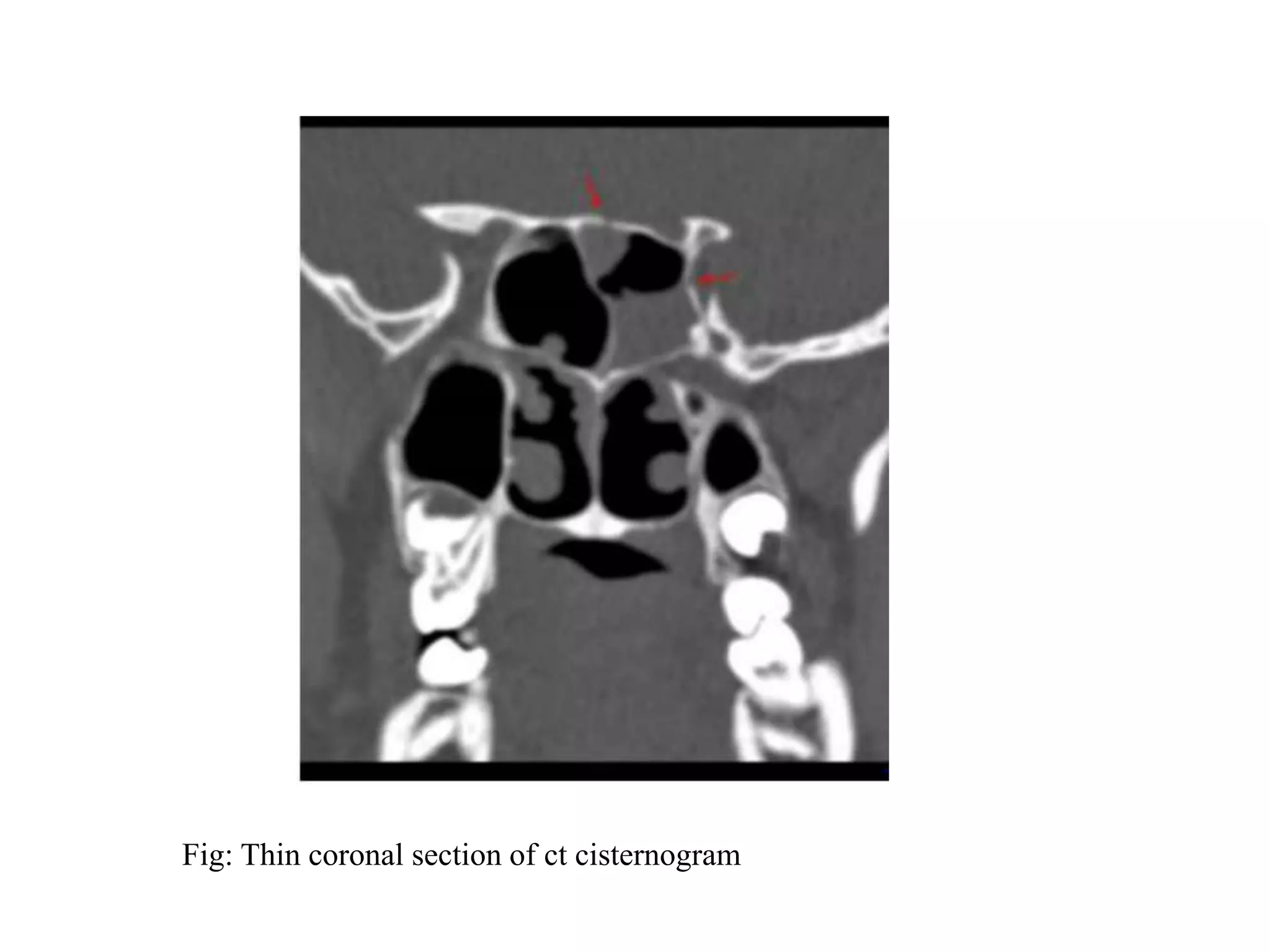
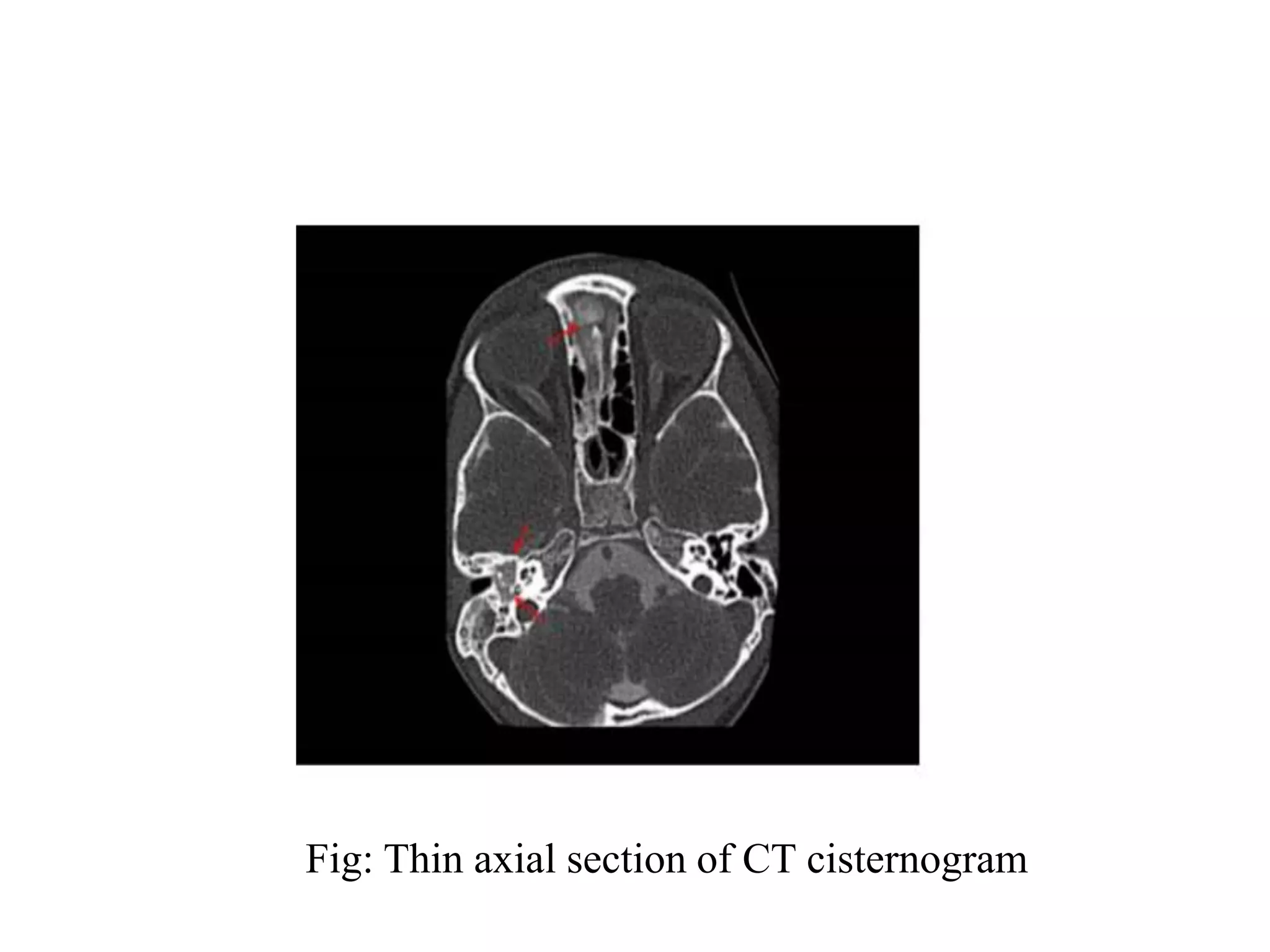
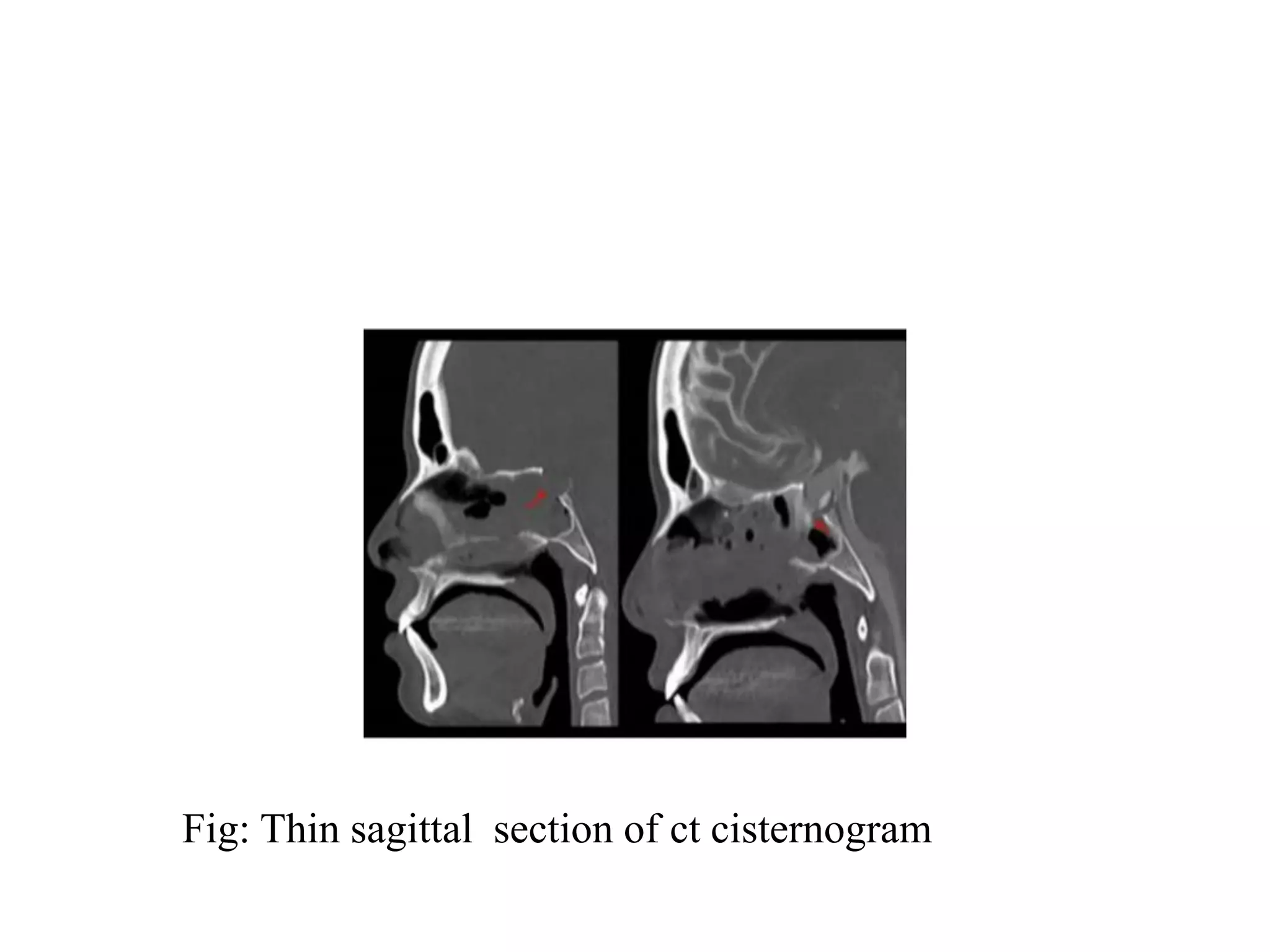
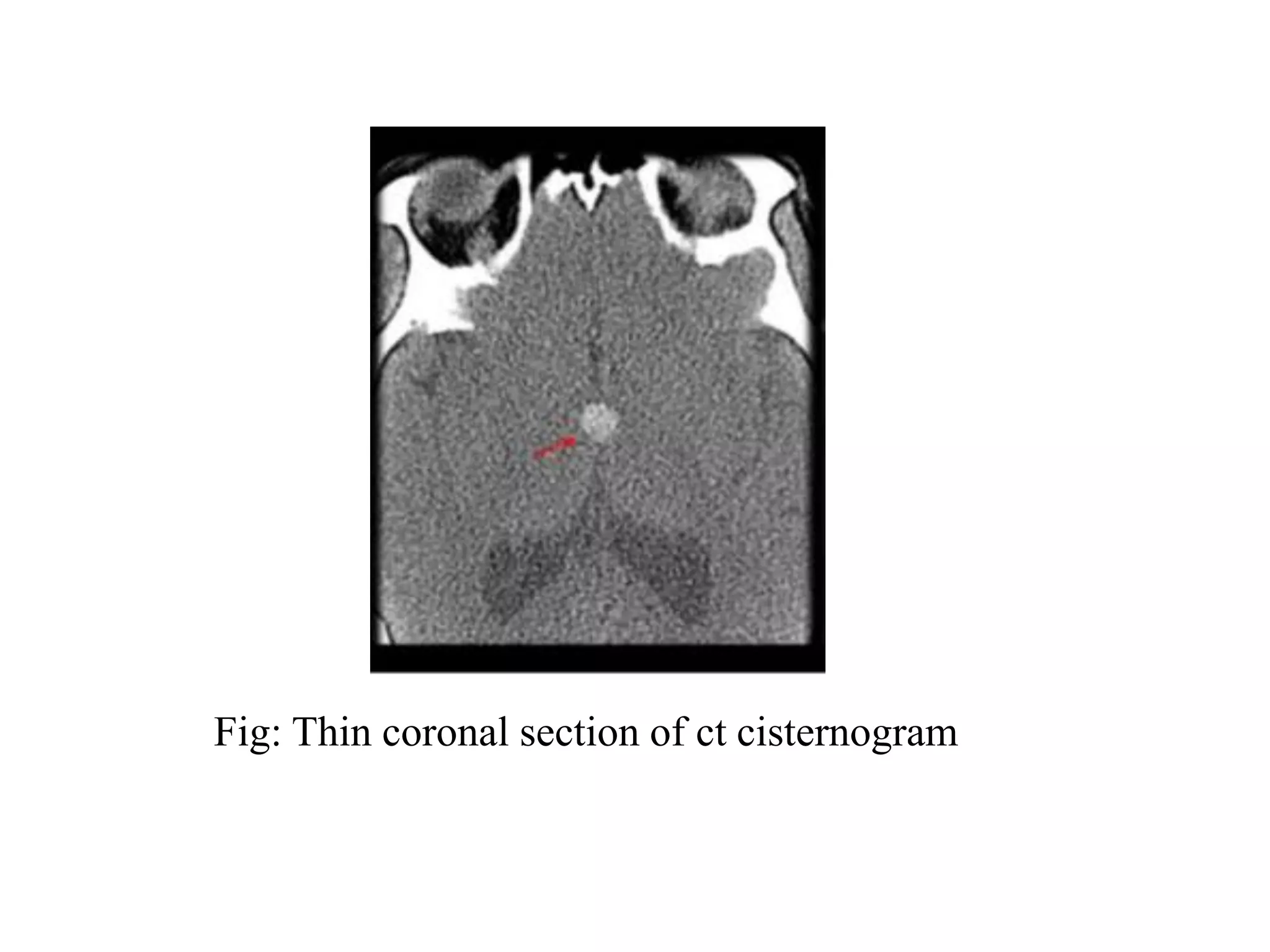
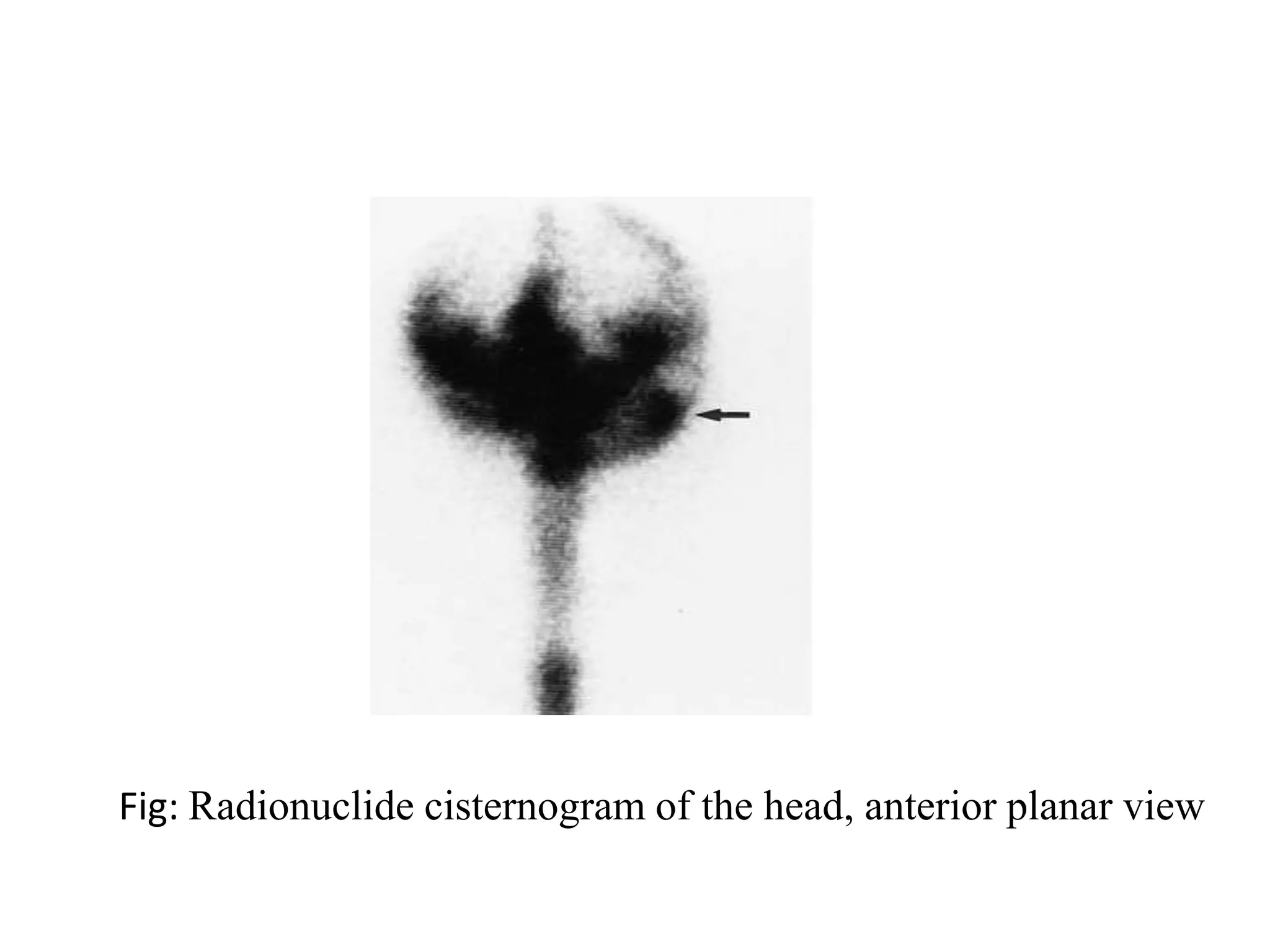
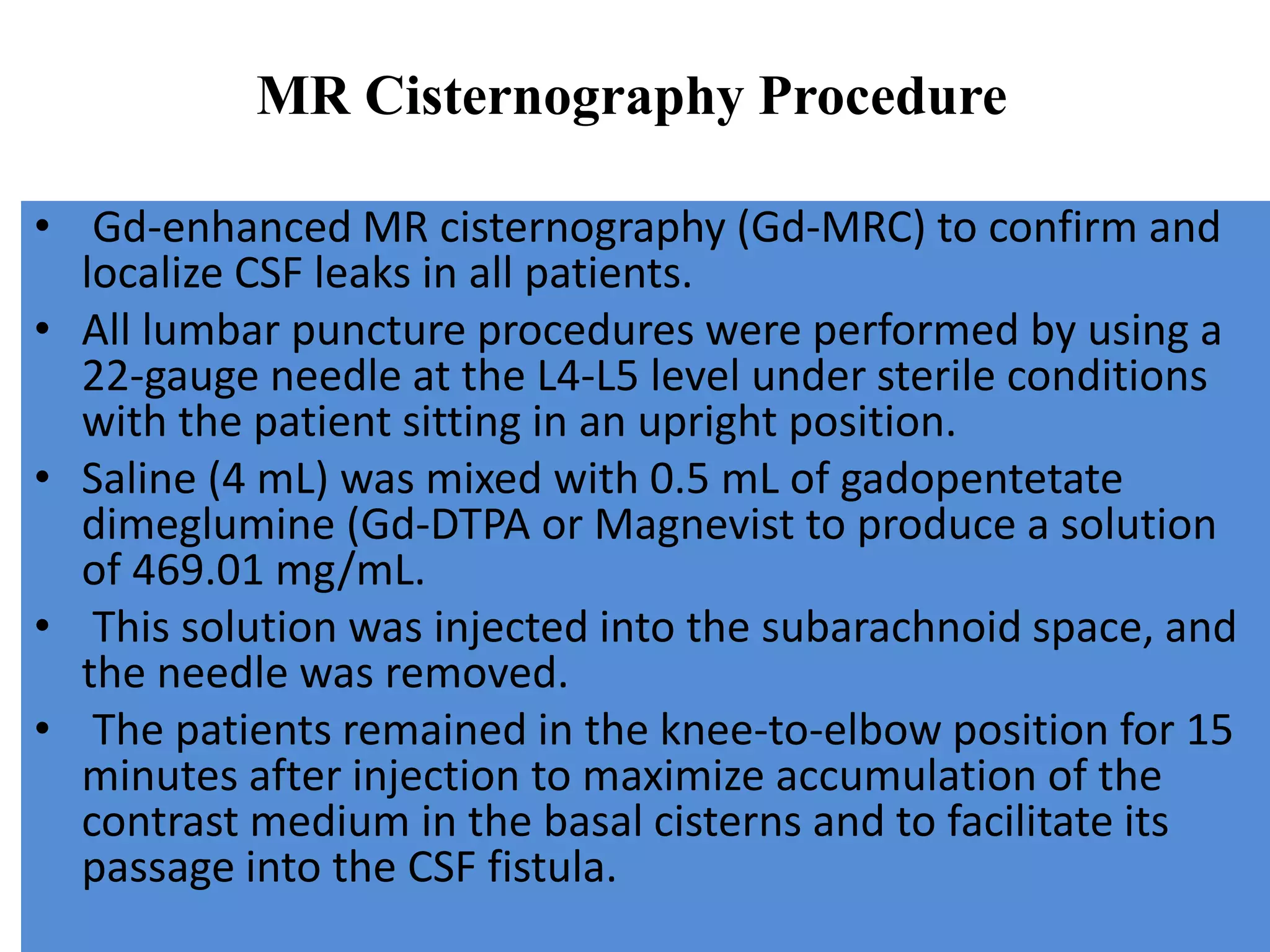
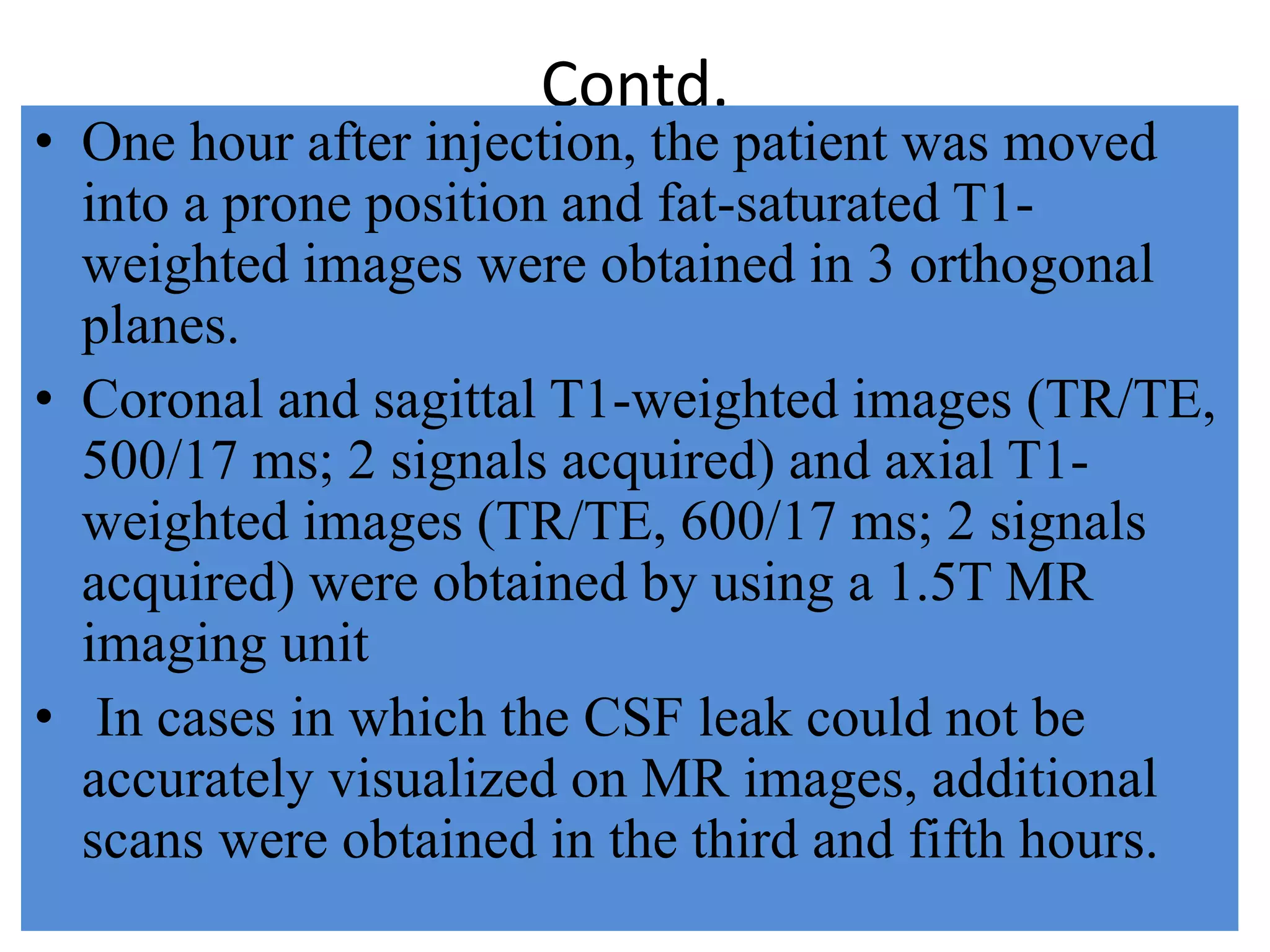
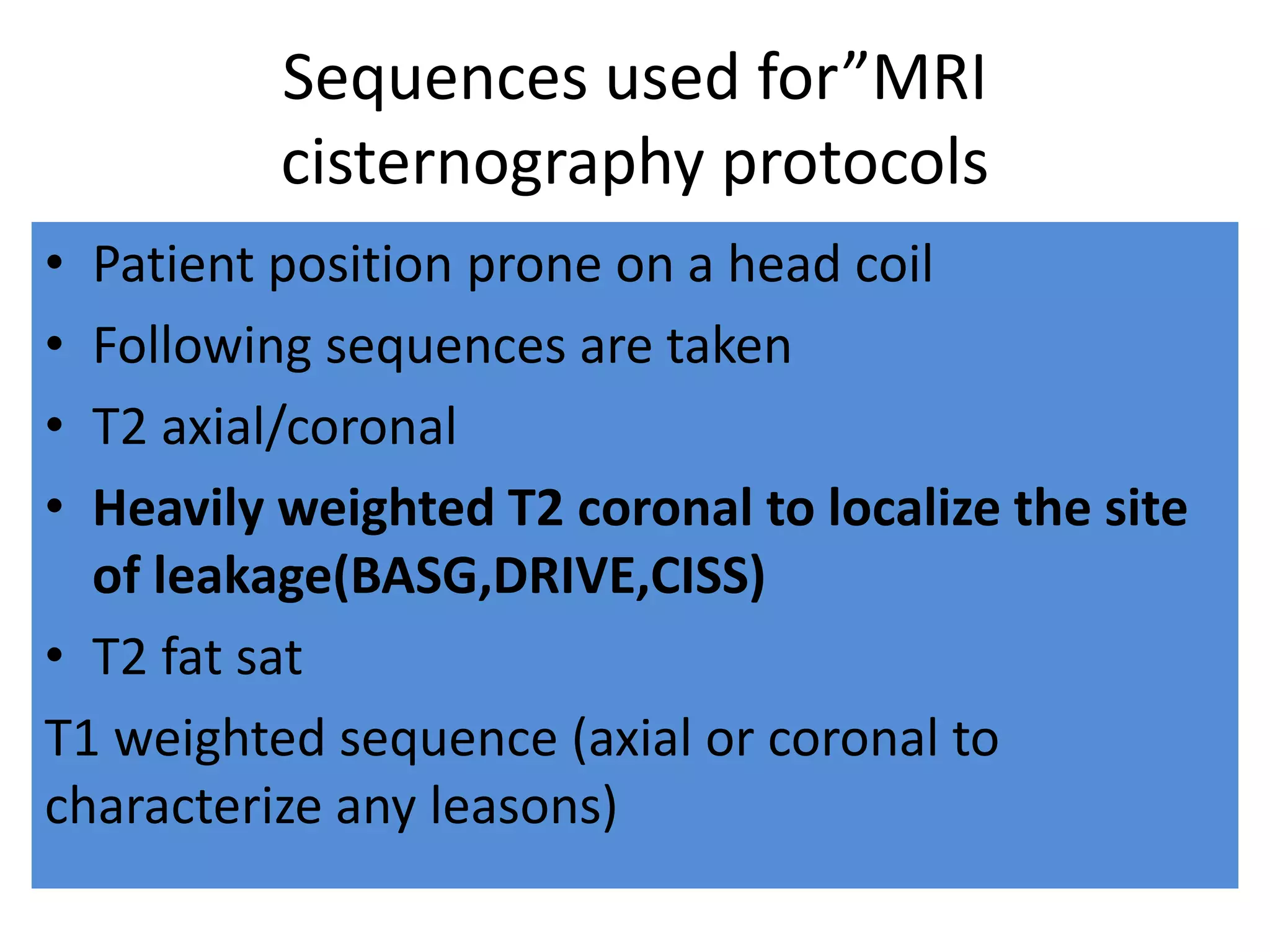
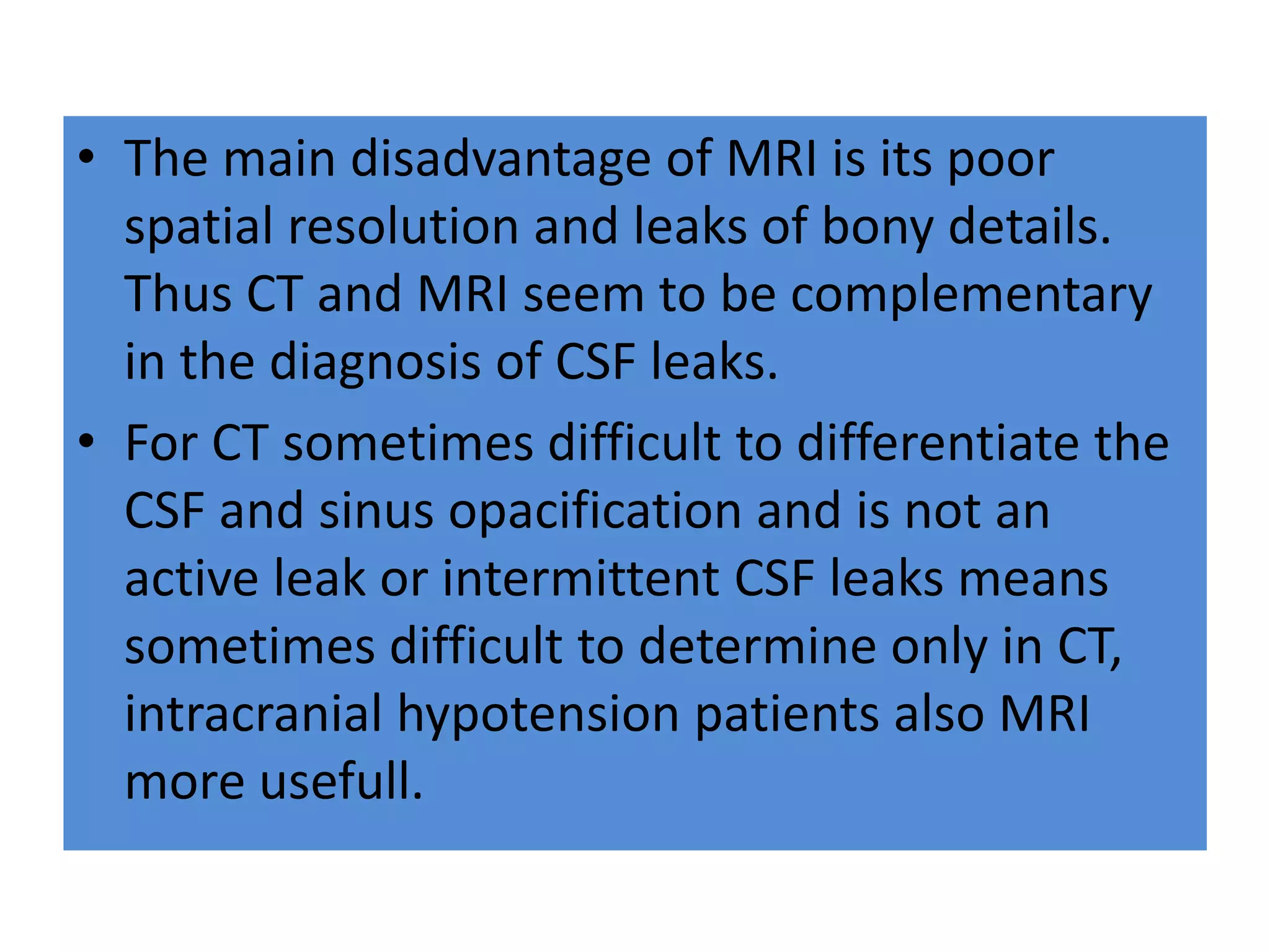
The document provides an overview of cisternography, a radiological procedure to identify the location of cerebrospinal fluid (CSF) leakage. It discusses the anatomy of CSF cisterns in the brain, indications for cisternography including traumatic and non-traumatic CSF leaks, contraindications, and the procedure which involves a lumbar puncture to inject contrast followed by imaging. Patient preparation, consent, and post-procedure care are also outlined.