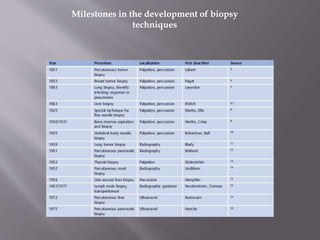
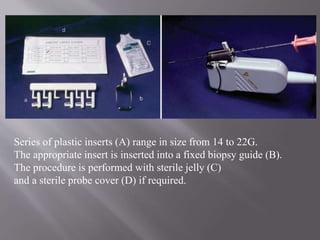
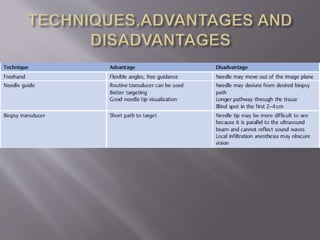
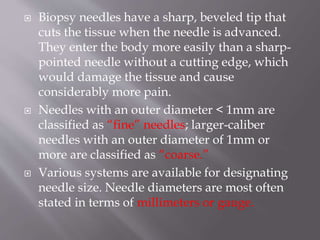
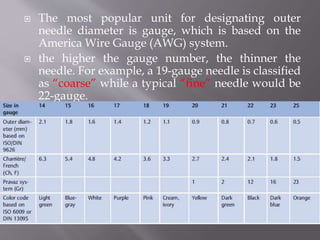
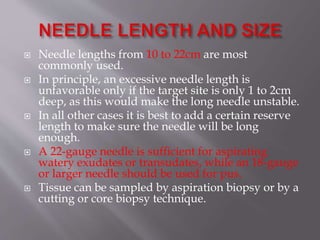
This document discusses the history and development of ultrasound-guided needle procedures from the 1960s onwards. It notes that while early studies showed minor risks, later reviews found complication rates up to 0.9% with some mortality. The document outlines key aspects of performing biopsies safely and effectively using ultrasound guidance, including appropriate patient preparation, informed consent, needle choice, and specimen handling. It emphasizes the importance of real-time visualization to target lesions precisely while avoiding vital structures.