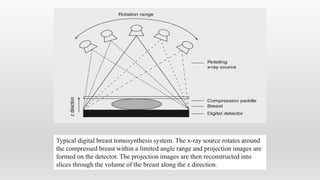
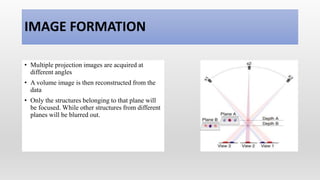
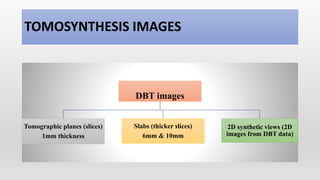
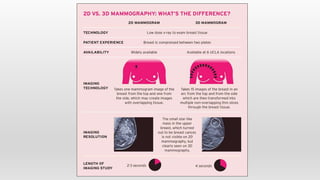
Digital breast tomosynthesis (DBT) is an emerging 3D breast imaging technique that involves acquiring low-dose X-ray images of the stationary breast from multiple angles to create tomographic slices. The first DBT system was introduced in 2011. DBT provides improved visualization of lesions and reduced call back rates compared to 2D digital mammography. While DBT exposes patients to a higher radiation dose than 2D mammography alone, combining DBT with a synthesized 2D mammogram can achieve a radiation dose similar to standard mammography alone. DBT is being widely adopted for breast cancer screening due to its superior performance over conventional digital mammography.


![ADVANTAGES
• Overlapping tissue structures are
resolved
• Improved visualization of lesion
margins
• Detecting subtle lesions
• Patient call back is reduced
Example of tomosynthesis. Improved visualization of architectural
distortion (circle in [b]) in the center of the right breast in tomosynthesis, as
compared to reconstructed 2D digital images. (a) Reconstructed 2D image.
(b) Tomosynthesis: single slice image.](https://image.slidesharecdn.com/digitalbreasttomosynthesis-211213051215/85/Digital-breast-tomosynthesis-11-320.jpg)