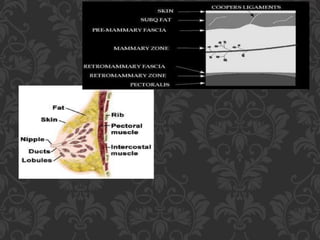
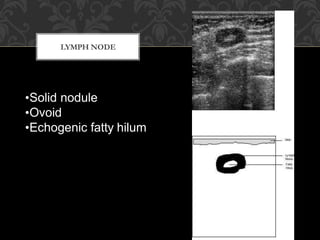
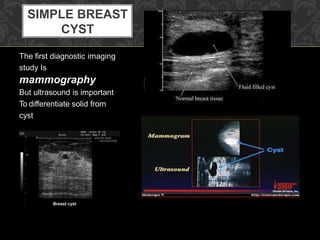
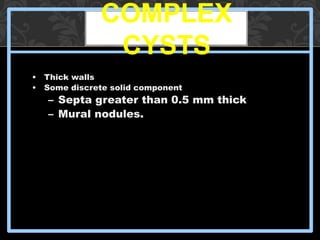
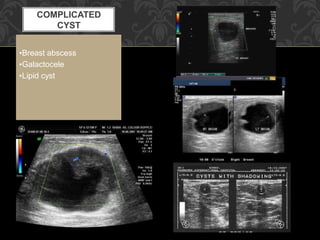
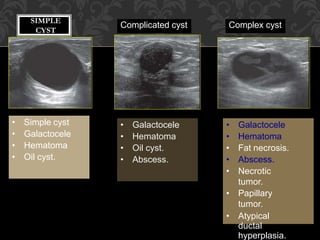
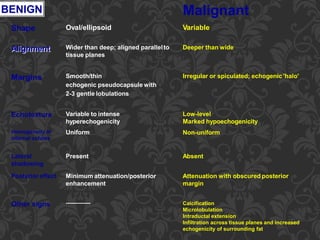
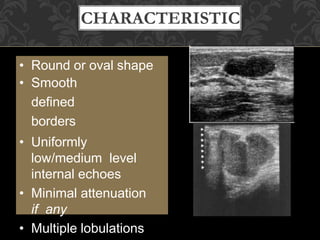
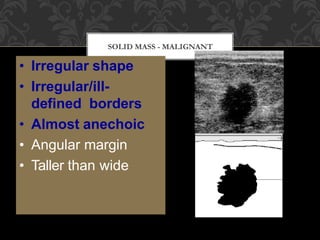
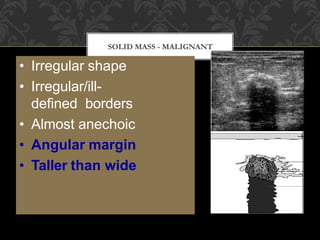
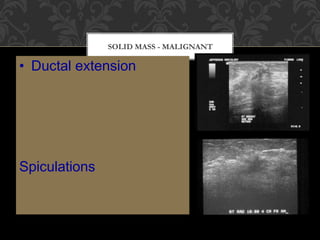
Breast ultrasound uses high-frequency sound waves to detect breast abnormalities. It has high sensitivity in detecting breast lesions. Modern ultrasound equipment with high-frequency transducers can detect malignancy associated with microcalcifications. Breast ultrasound is useful for differentiating between cystic and solid breast lesions. Simple cysts appear anechoic with thin walls and increased sound transmission, while complex cysts have thick walls, septations, or solid components. Malignant solid masses tend to have an irregular shape, angular margins, heterogeneity, and ductal extension, compared to benign masses which are often oval with smooth margins and uniform internal echoes.