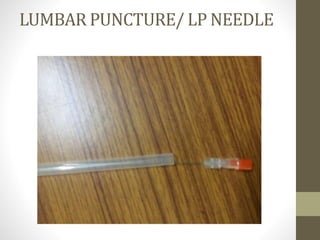
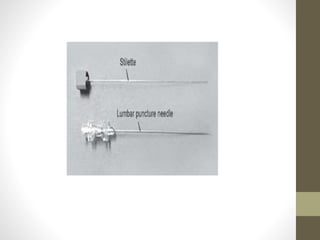
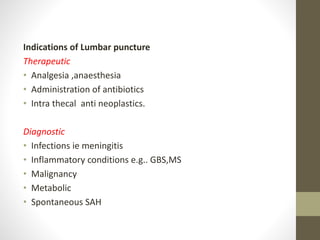
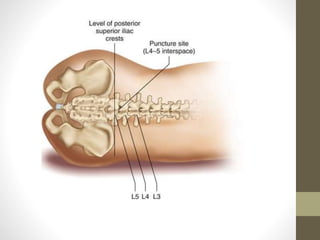
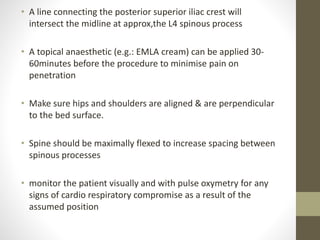
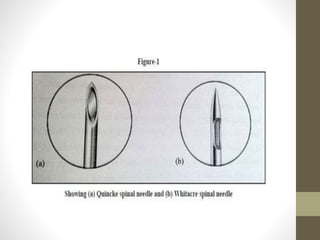
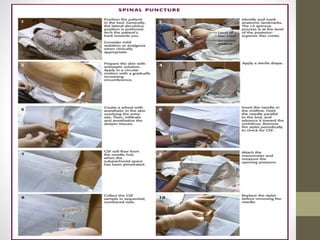
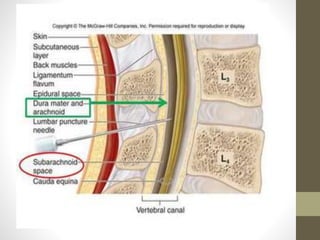
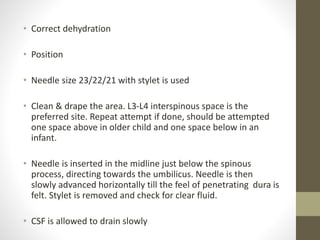
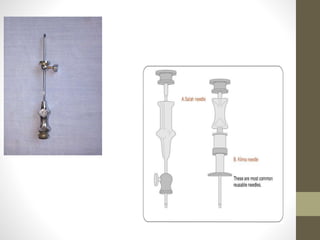
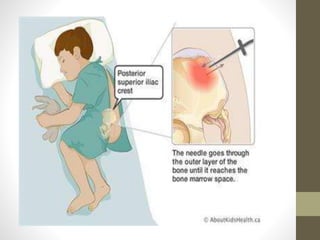
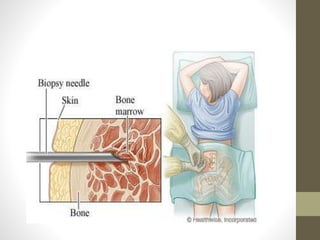
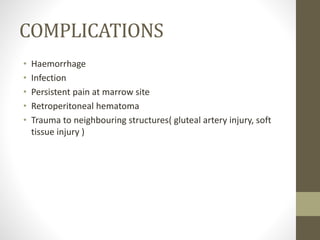
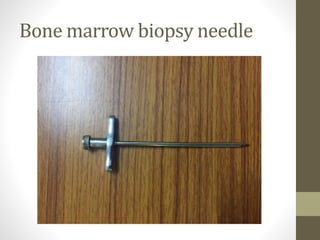
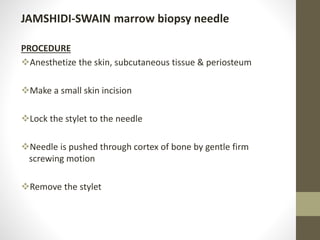
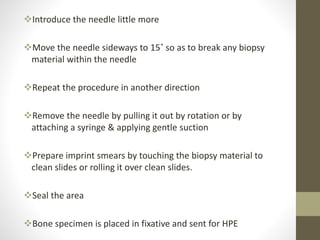
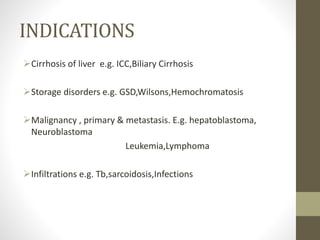
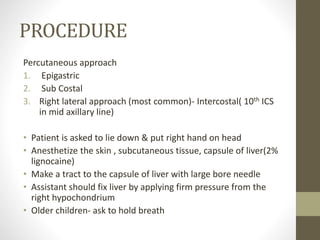
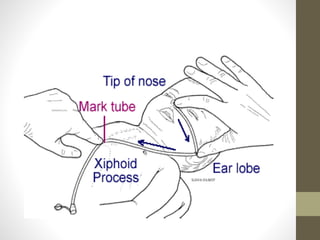
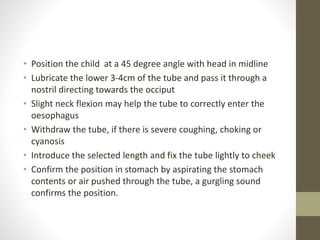
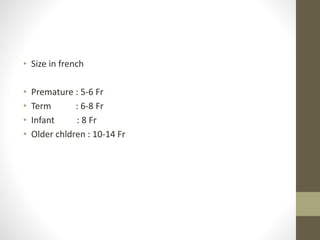
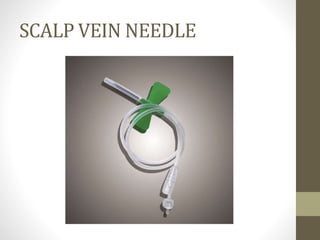
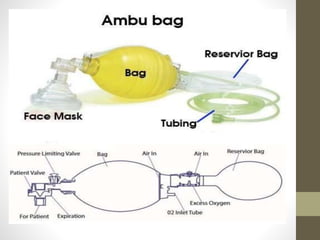
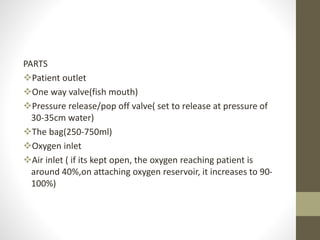
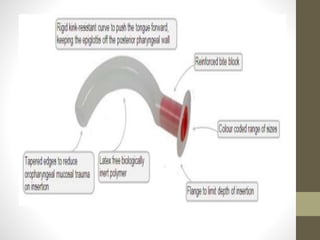
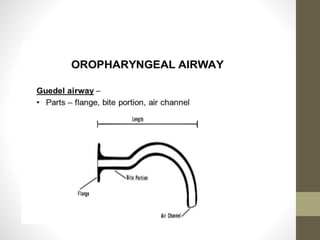
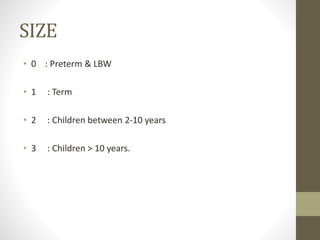
This document provides information on various pediatric medical instruments and procedures. It describes the indications, contraindications, complications and steps for performing lumbar punctures, bone marrow aspirations, liver biopsies, nasogastric/feeding tubes, suction tubes, scalp vein needles, Ambu bags, bag valve masks, Guedel airways, and laryngoscopes. Key details are provided for each instrument/procedure including appropriate sizes, positioning, sterile technique, and monitoring for complications.