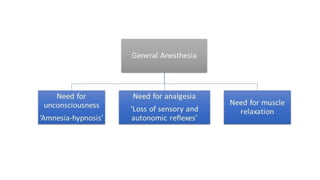
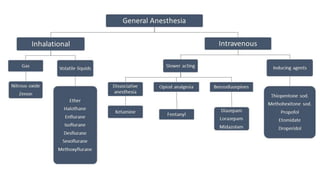
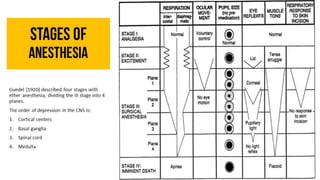
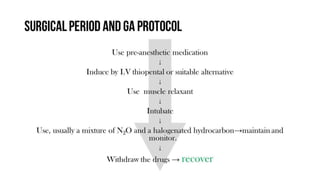
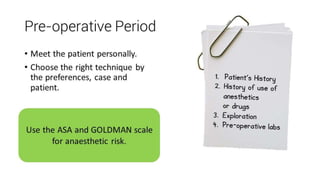
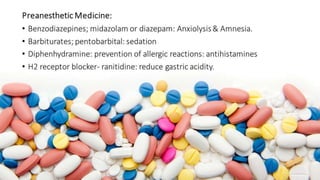
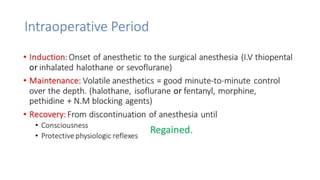
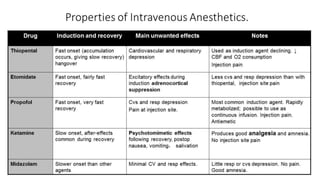
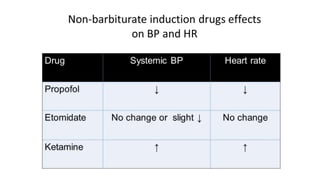
General anesthetics are drugs that induce reversible loss of consciousness and sensations during surgery. They work by depressing the central nervous system in stages, starting with cortical centers and ending with the medulla. There are two main types - inhalational gases administered through masks or intravenous drugs given through injections. A balanced anesthesia approach uses multiple drugs to induce unconsciousness, amnesia, analgesia, and muscle relaxation. Precise drug combinations and dosages are tailored for each patient and procedure type. The goal is to smoothly induce and rapidly recover from anesthesia with minimized risks and side effects.