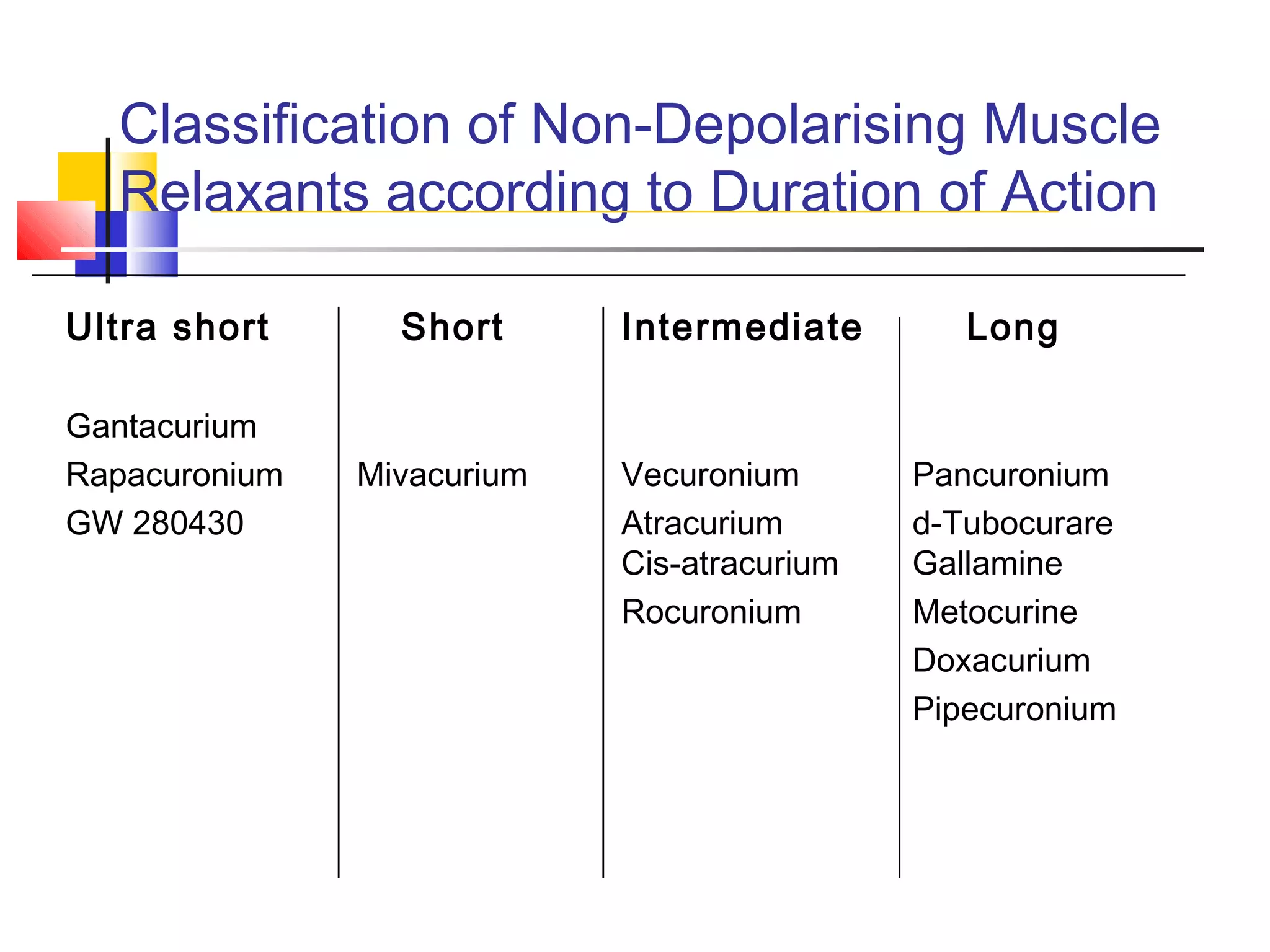
This document discusses skeletal muscle relaxants and their reversal. It begins by defining neuromuscular blocking drugs as those that act at the neuromuscular junction to block neuromuscular transmission, in order to facilitate muscle relaxation for surgery. It then covers the history, classification, and mechanisms of action of both depolarizing drugs like succinylcholine and non-depolarizing drugs. It discusses the pharmacology, clinical uses, and side effects of various muscle relaxants. It concludes by addressing the reversal of neuromuscular blockade using anticholinesterase drugs like neostigmine and strategies to minimize their muscarinic side effects.