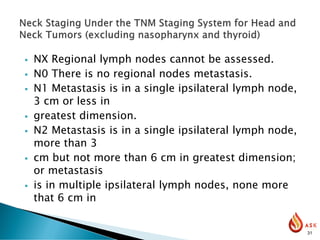
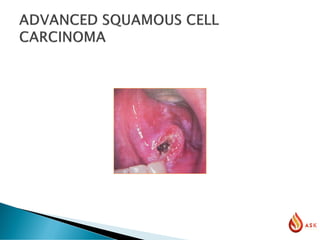
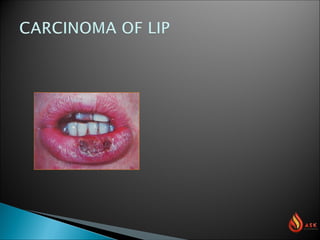
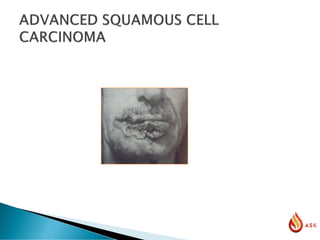
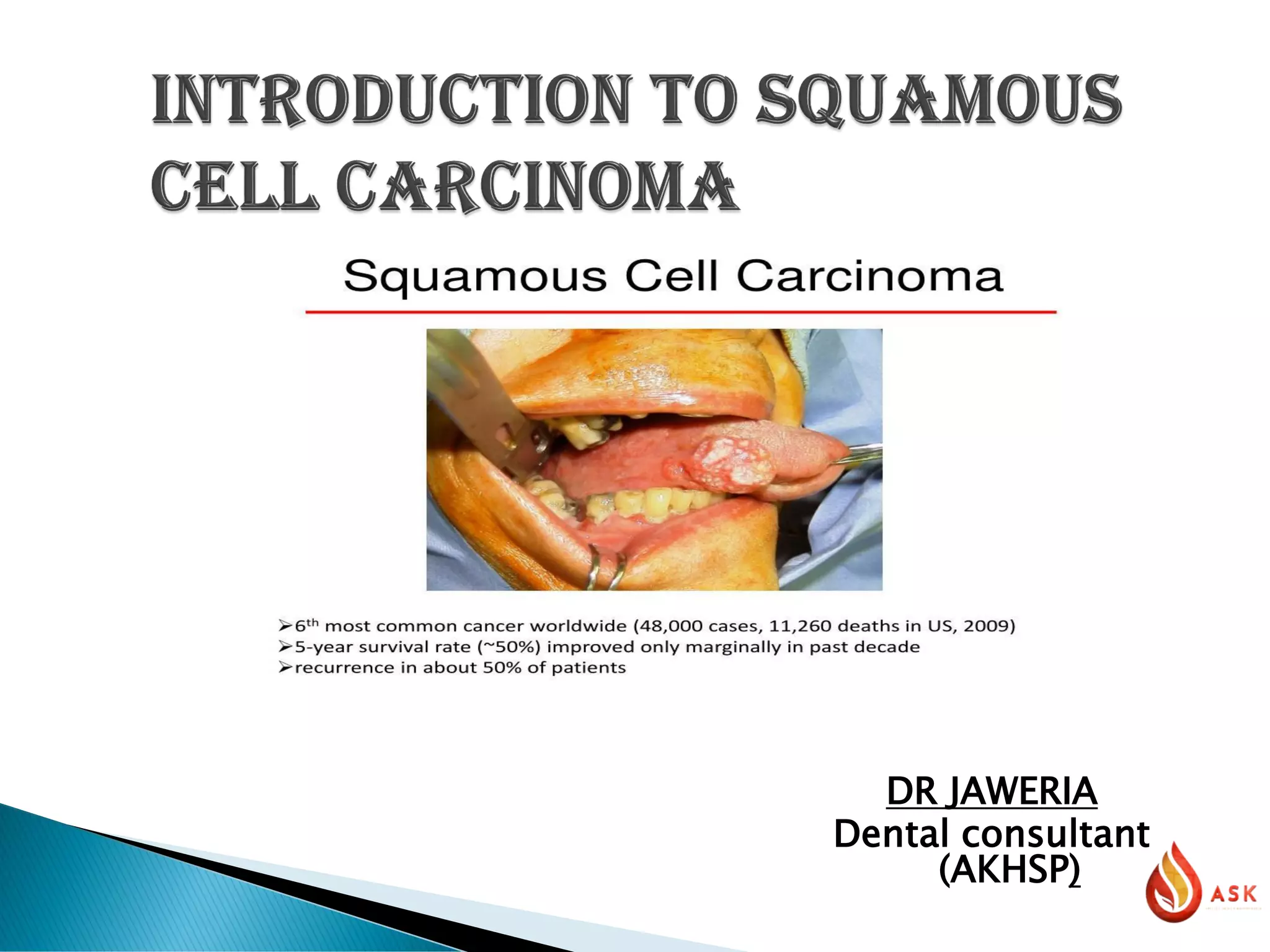
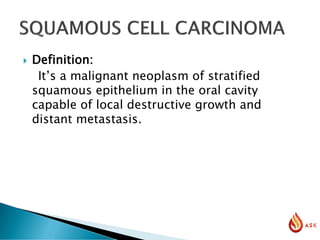
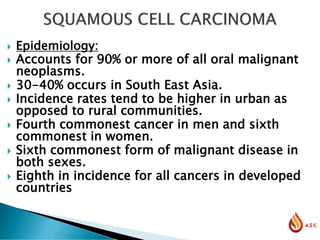
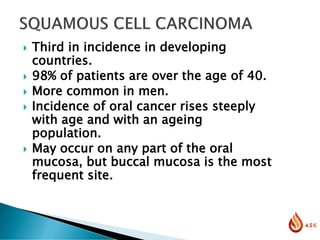
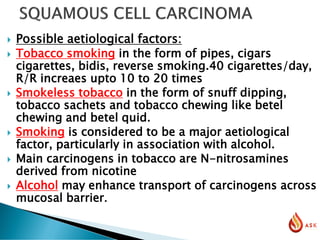
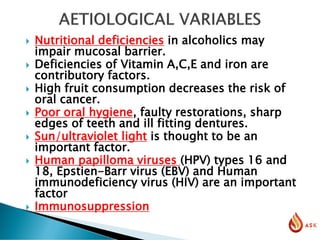
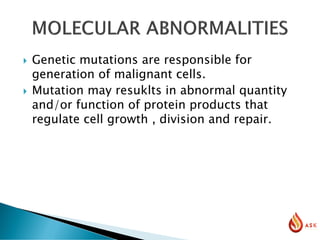
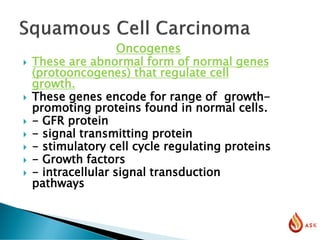
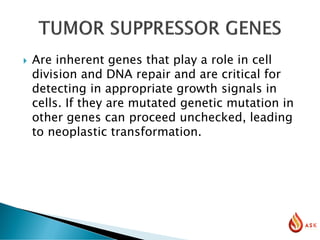
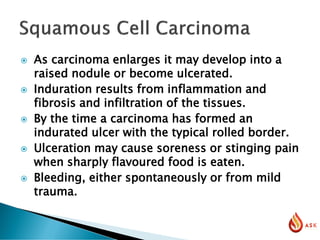
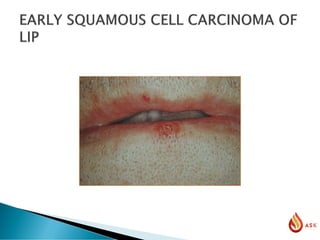
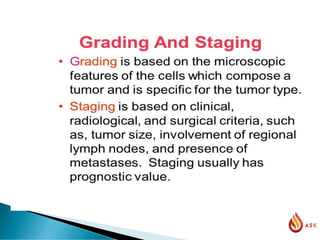
The document provides a comprehensive overview of squamous cell carcinoma (SCC) of the oral cavity, detailing its epidemiology, clinical features, diagnosis, and treatment options. SCC is the most prevalent oral malignant neoplasm, particularly affecting individuals over 40, with significant risk factors including tobacco and alcohol use, poor oral hygiene, and viral infections. The document also discusses staging, histopathological characteristics, and the importance of early diagnosis in influencing prognosis.




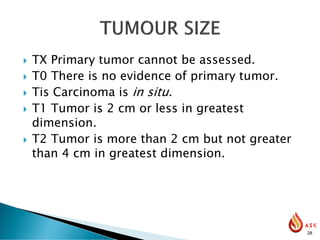
![ T3 Tumor is more than 4 cm in greatest
dimension.
T4 (lip) Tumor invades through cortical bone,
inferior alveolar nerve, floor of mouth, or skin
of face—i.e., chin or nose.
T4a (oral Tumor invades adjacent structures
(e.g., through cavity) cortical bone, into deep
[extrinsic] muscle of tongue](https://image.slidesharecdn.com/sccweb-230313143010-b17c1bde/85/Oral-Squamous-Cell-Carcinoma-29-320.jpg)
![ [genioglossus, hypoglossus, palataglossus,
and styloglossus], maxillary sinus, skin of
face).
T4b Tumor invades masticator space,
pterygoid plates, or skull base and/or
encases the internal carotid artery.
Note: Superficial erosion alone of bone/tooth
socket by gingival primary
is not sufficient to classify as T4.](https://image.slidesharecdn.com/sccweb-230313143010-b17c1bde/85/Oral-Squamous-Cell-Carcinoma-30-320.jpg)