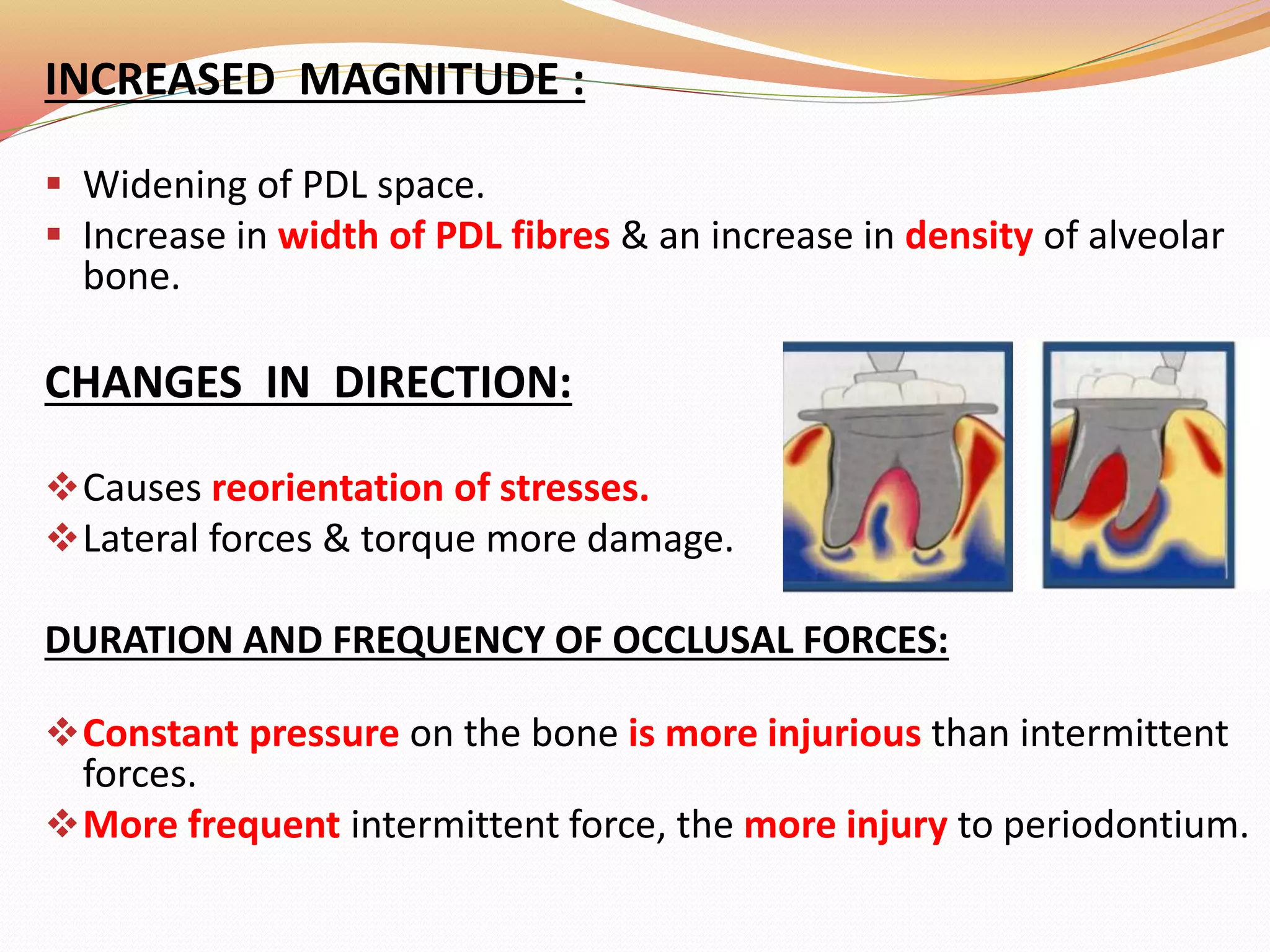
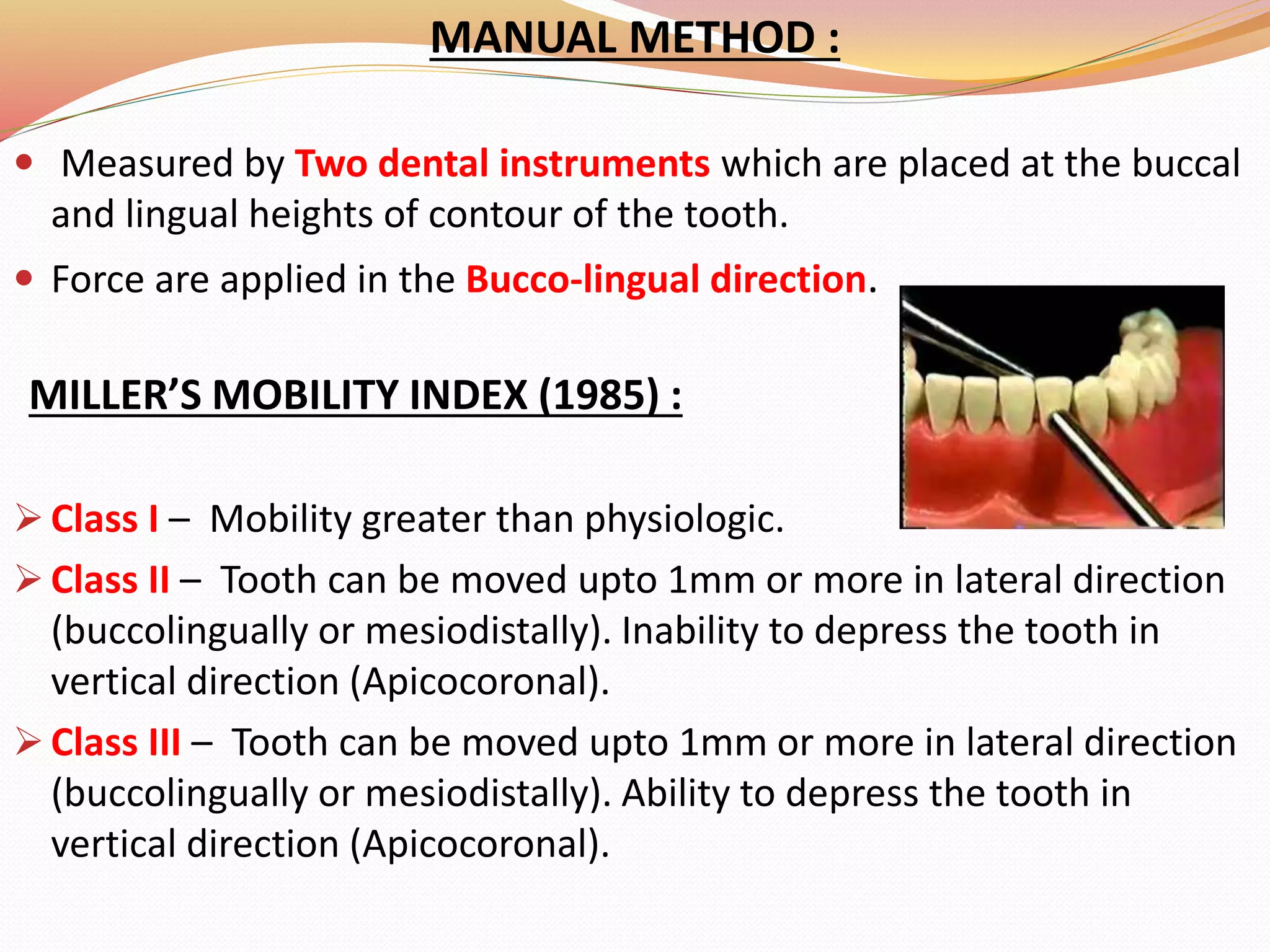
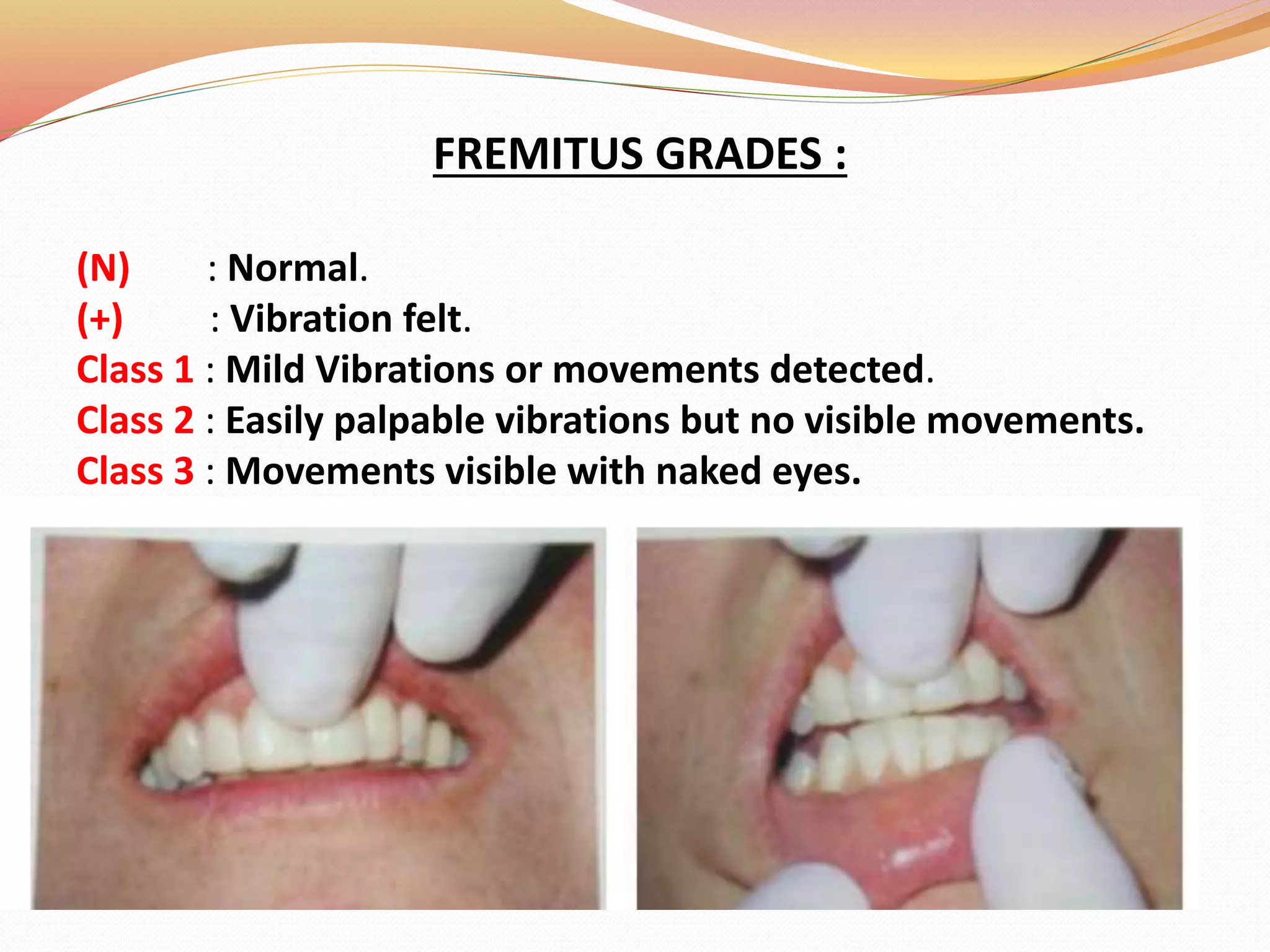
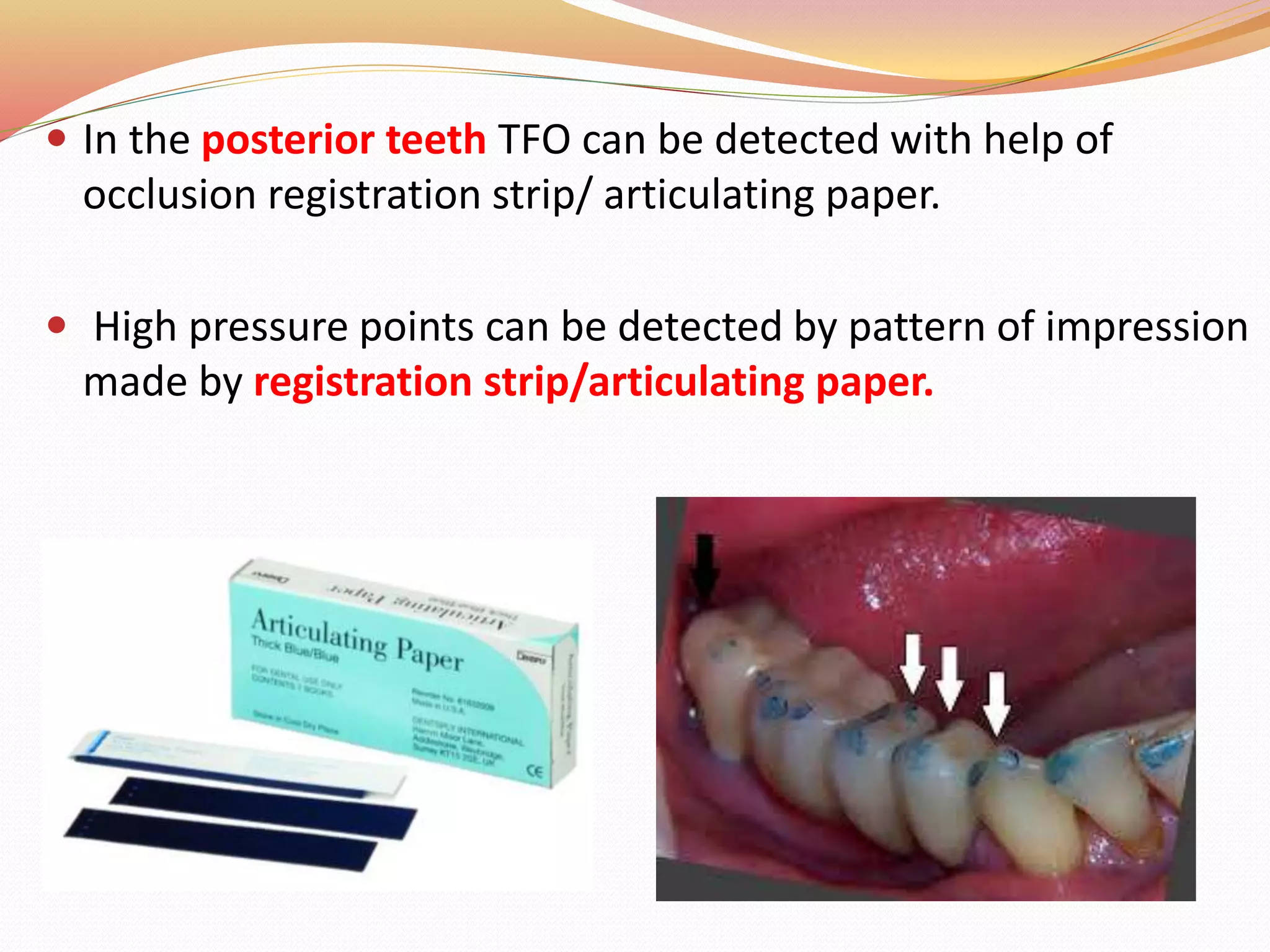
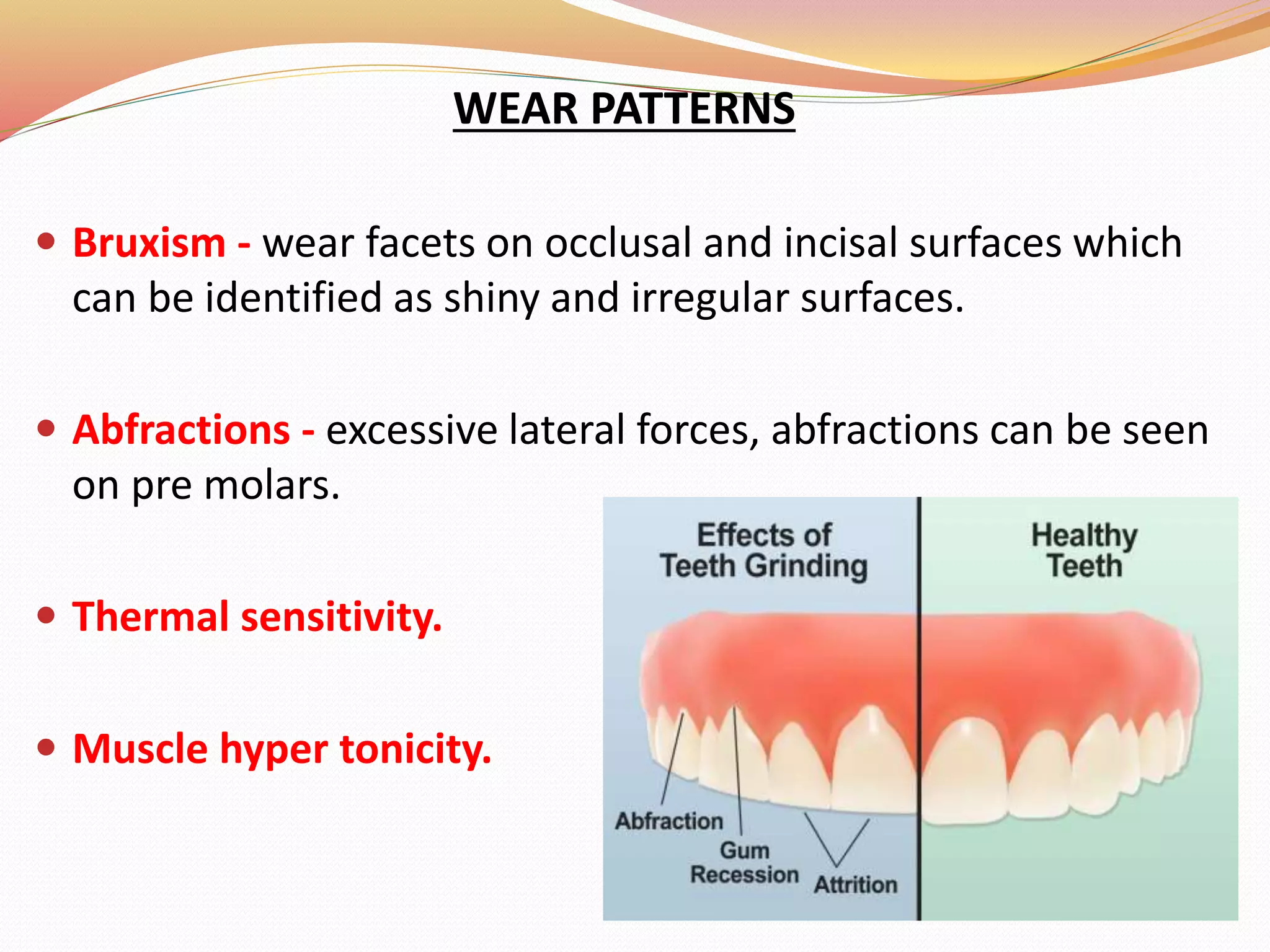
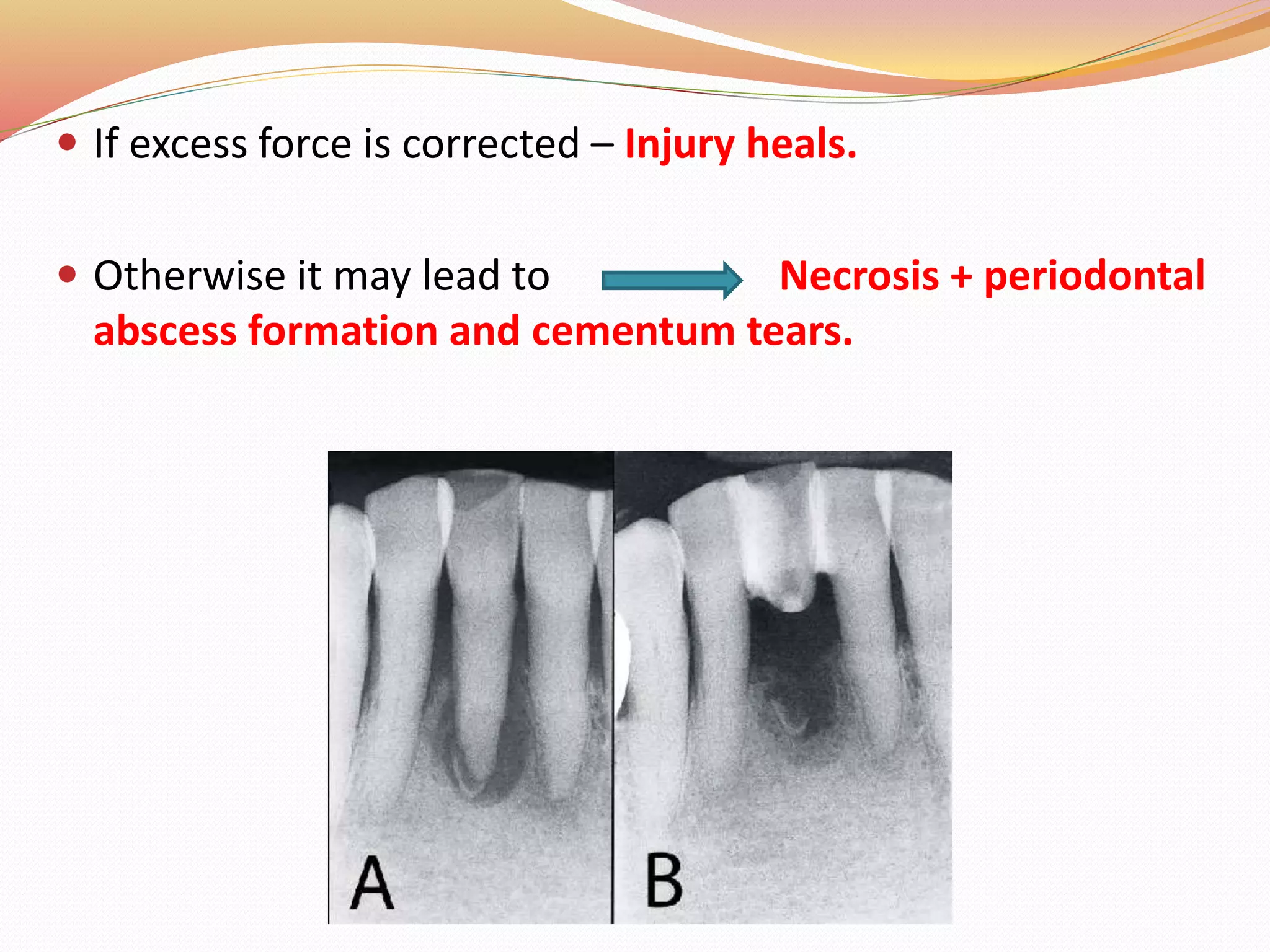
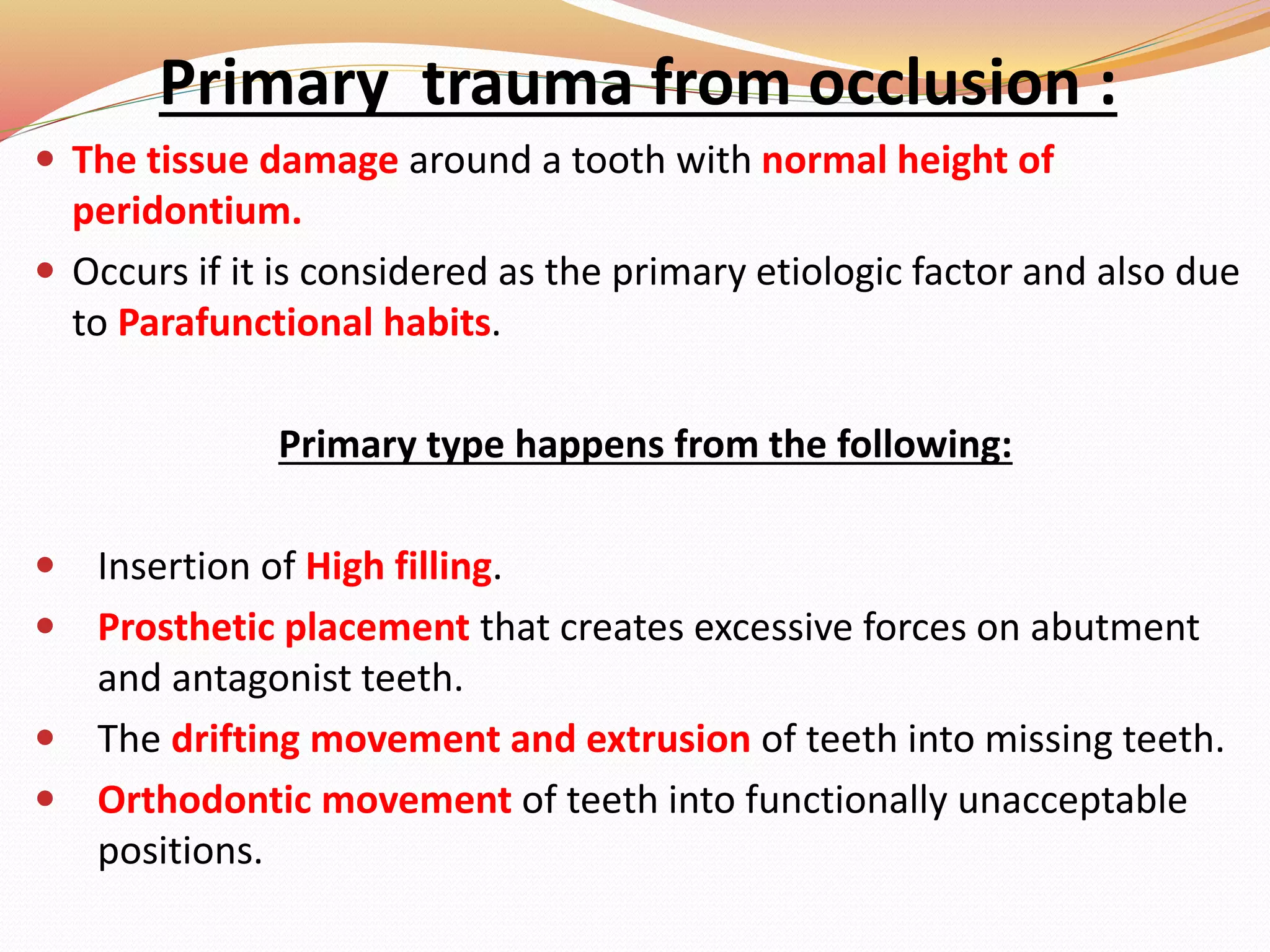
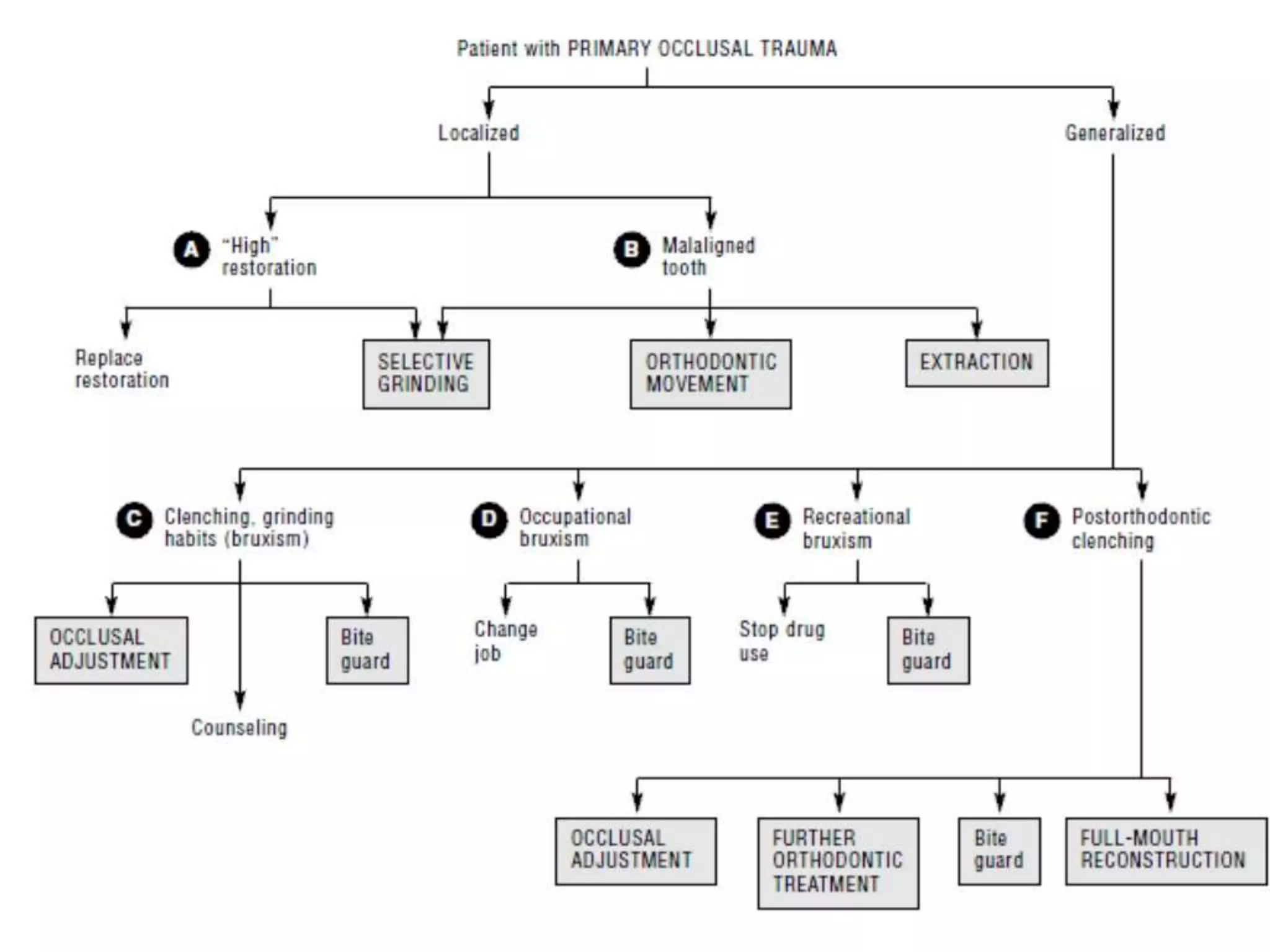
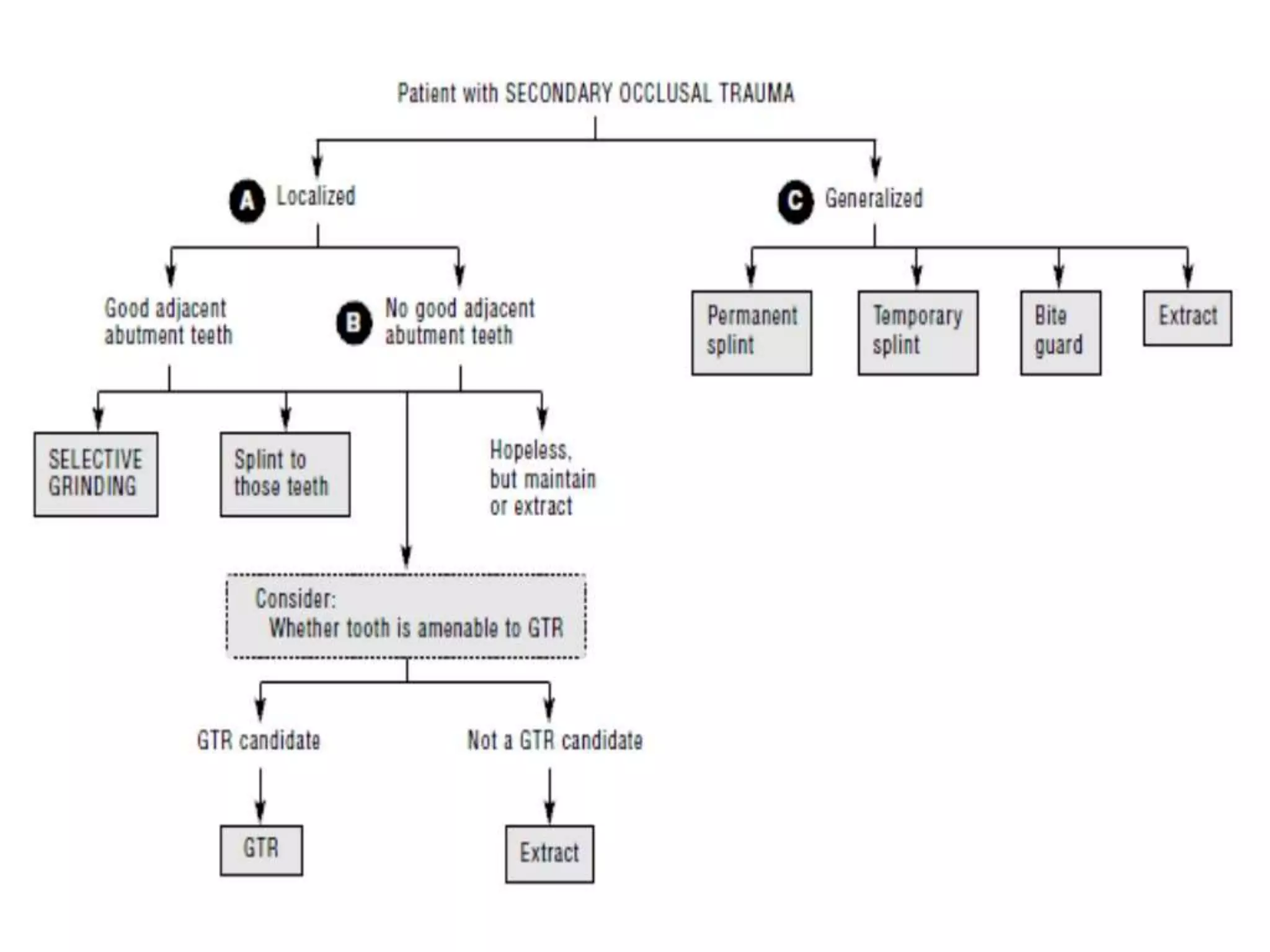
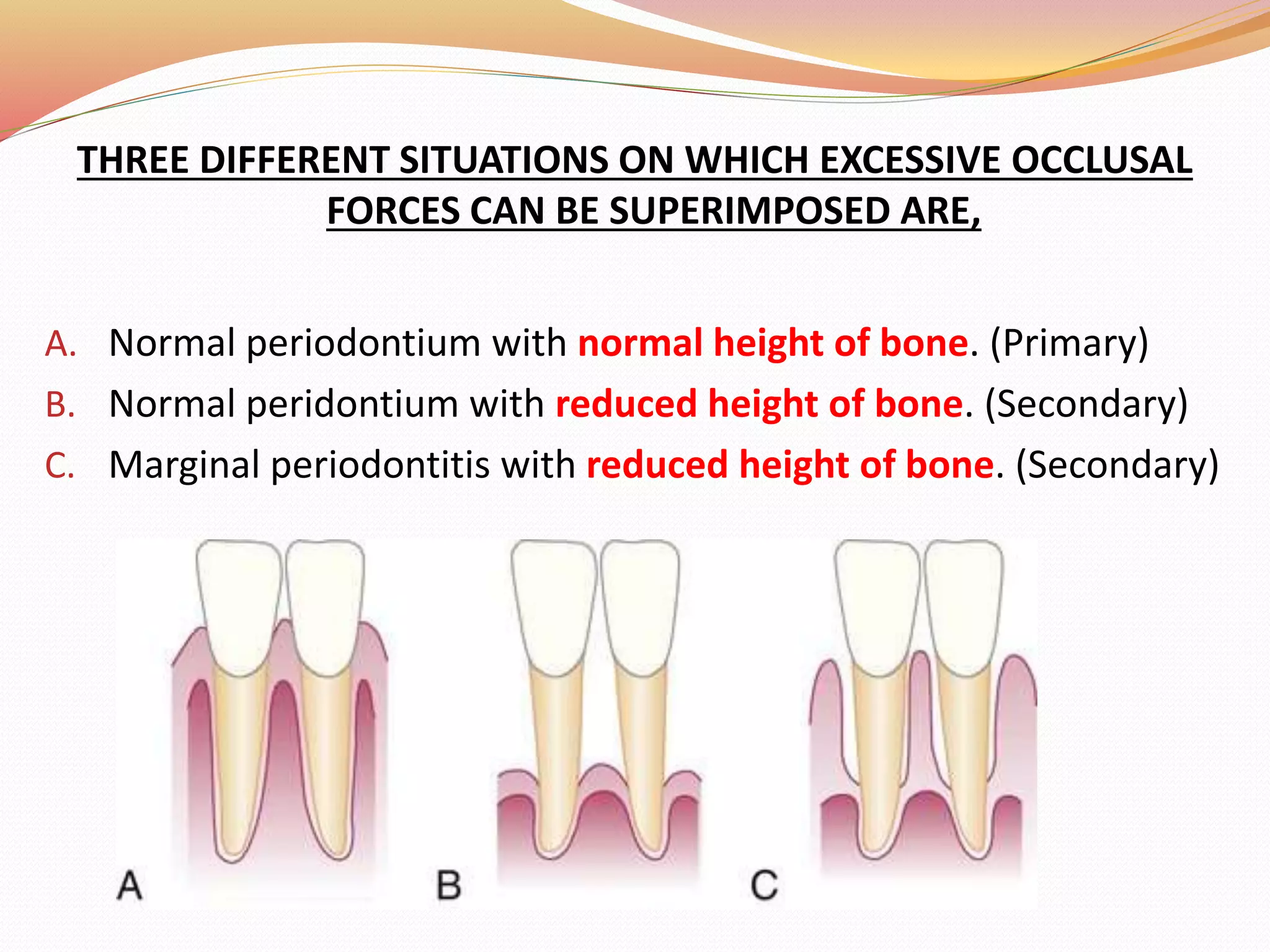
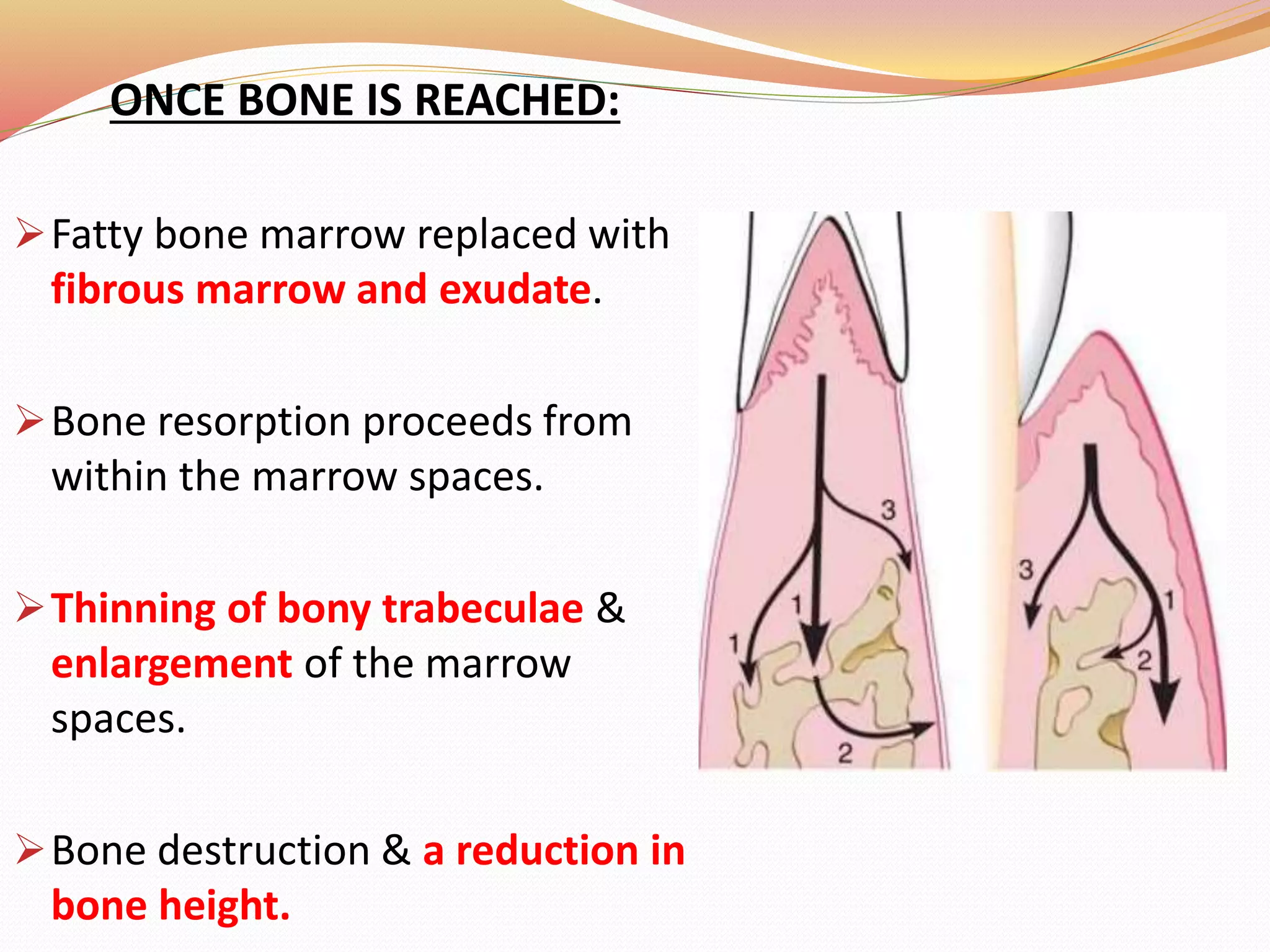
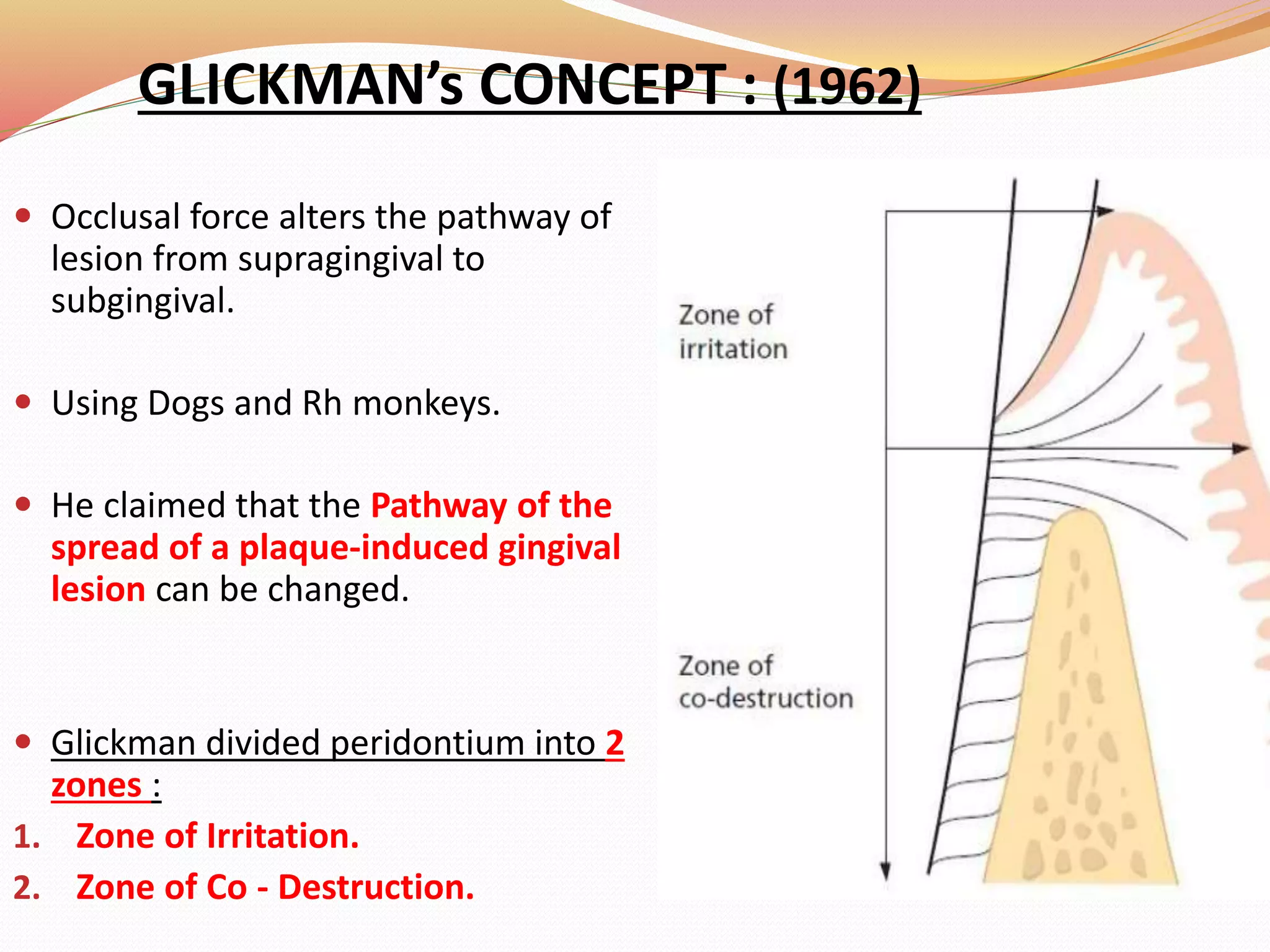
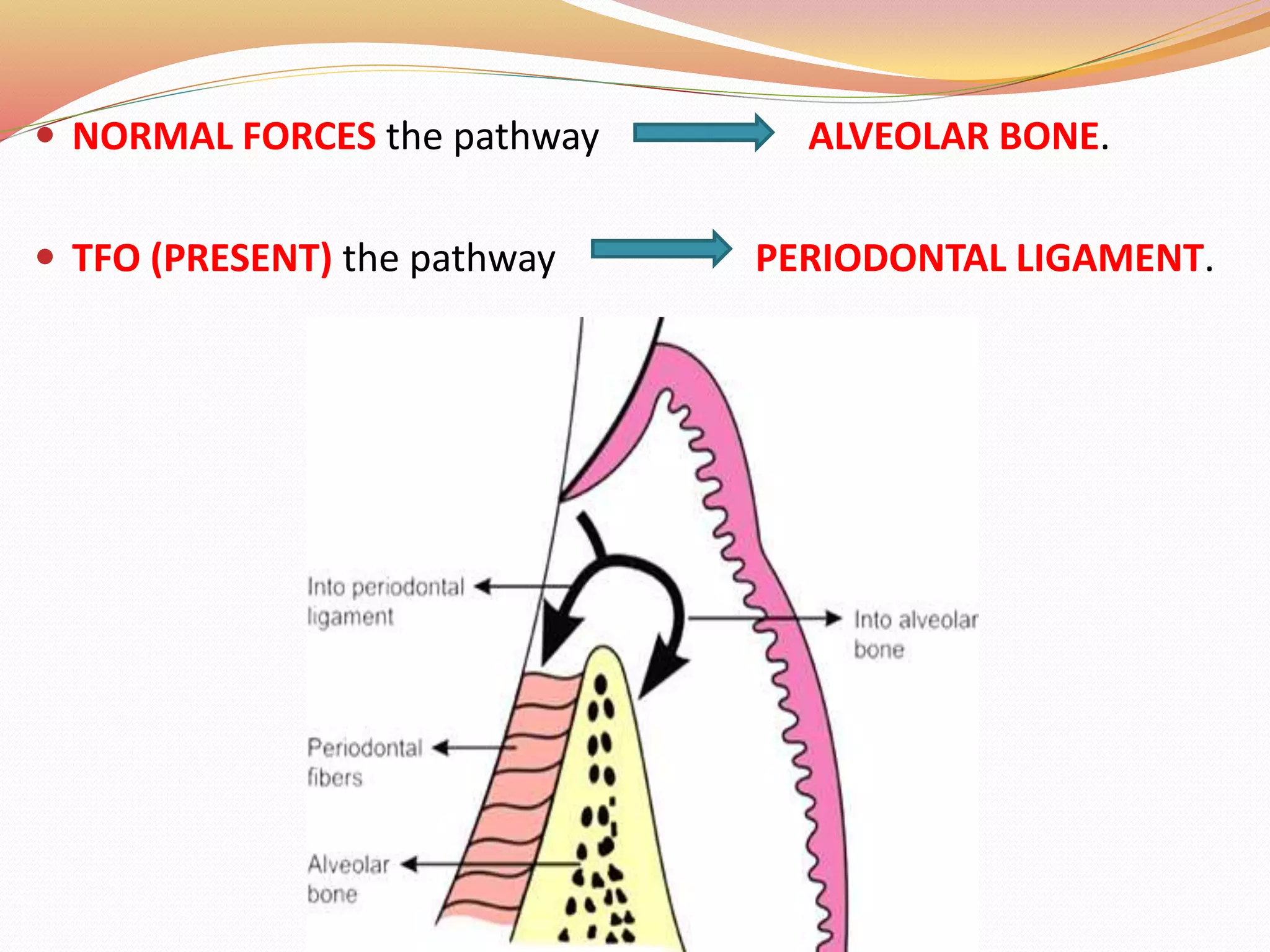
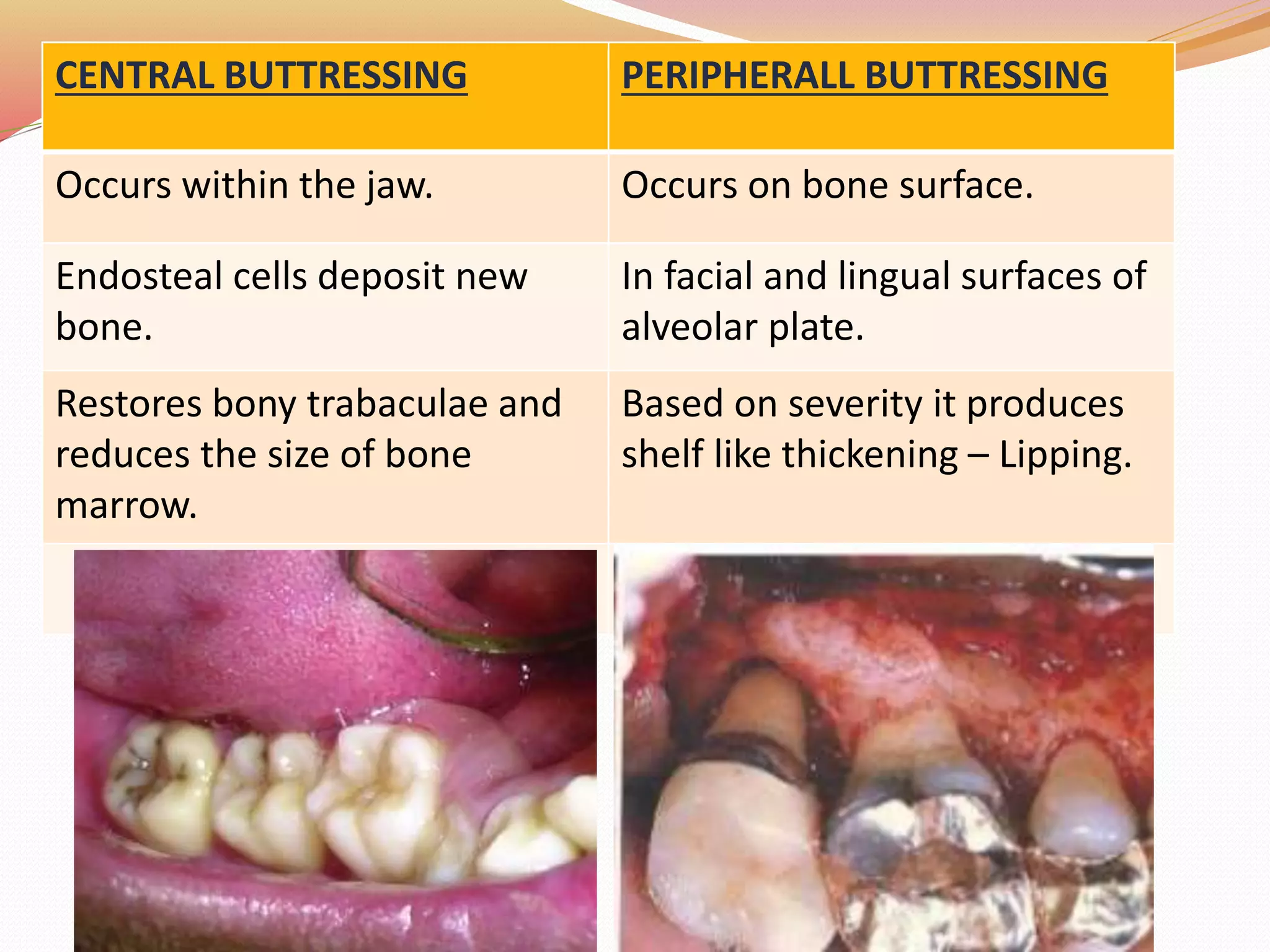
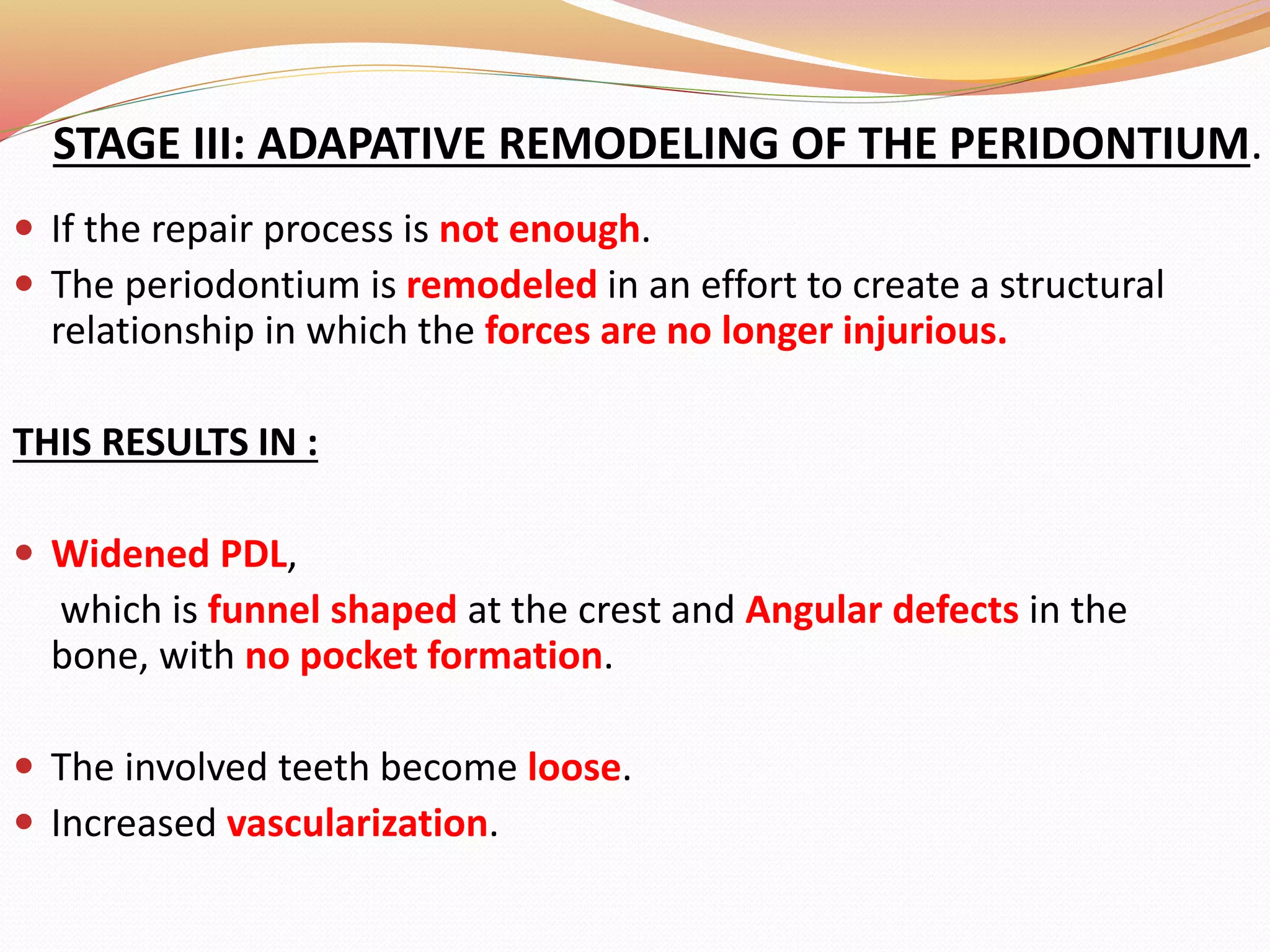
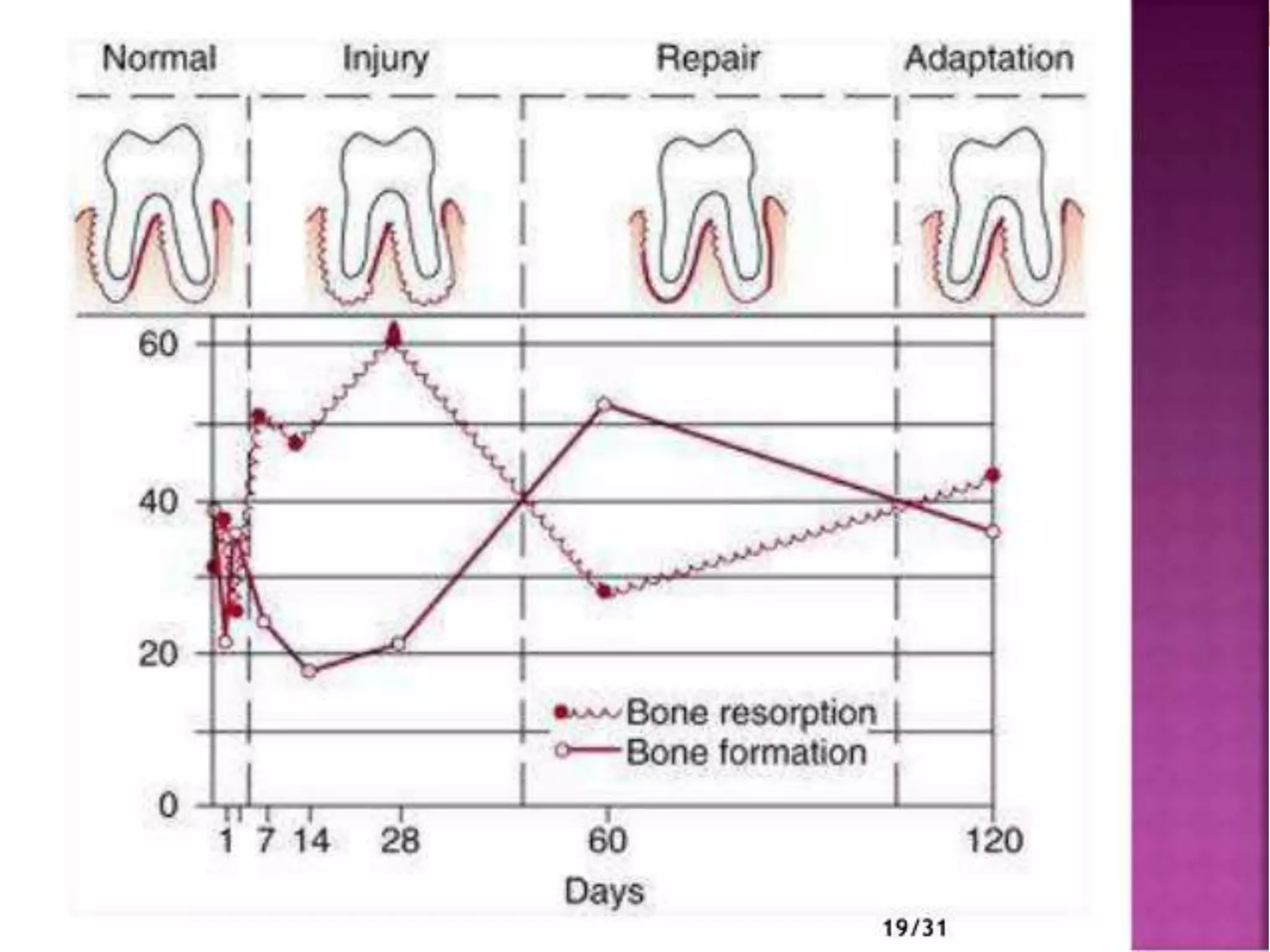
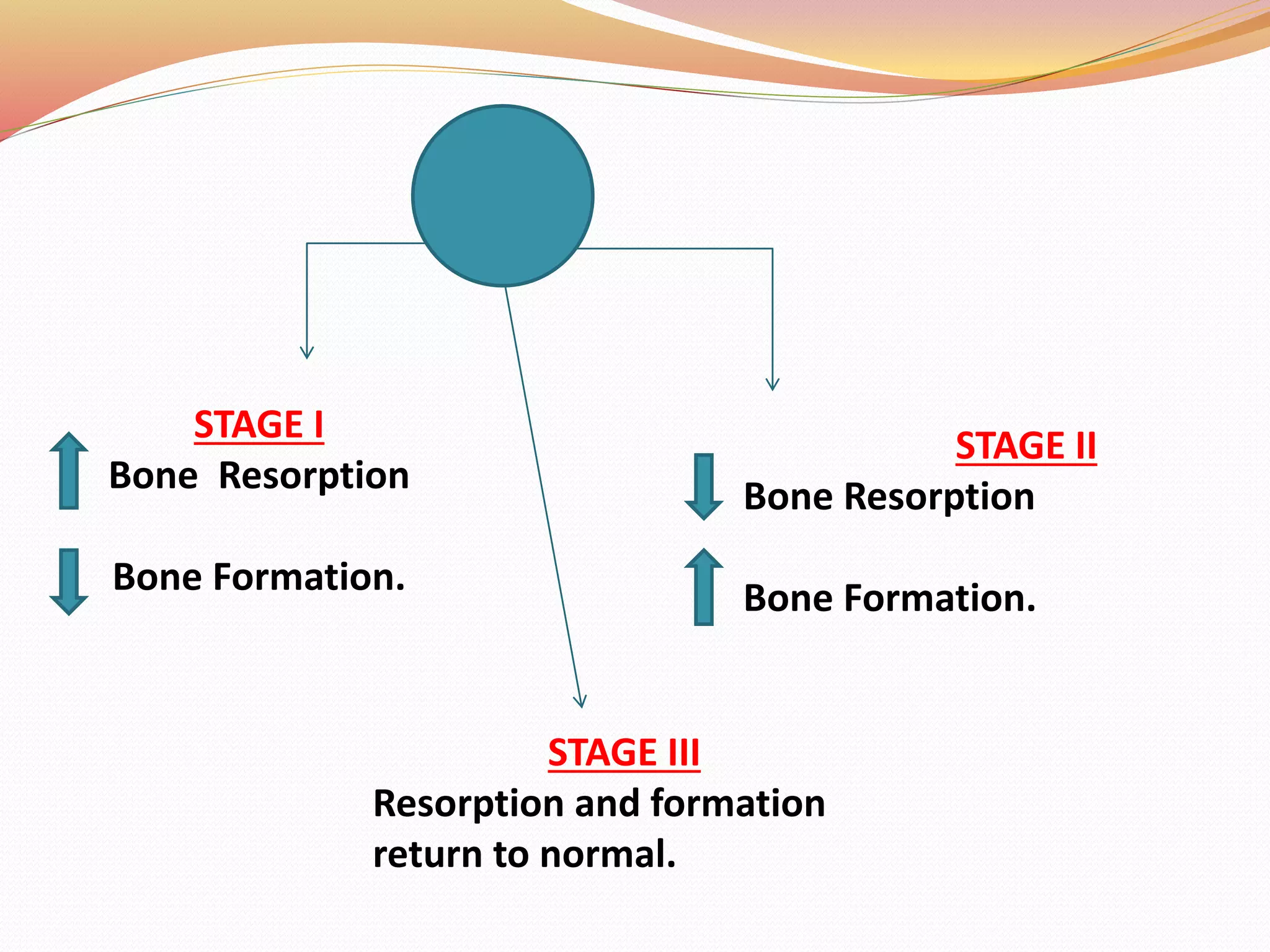
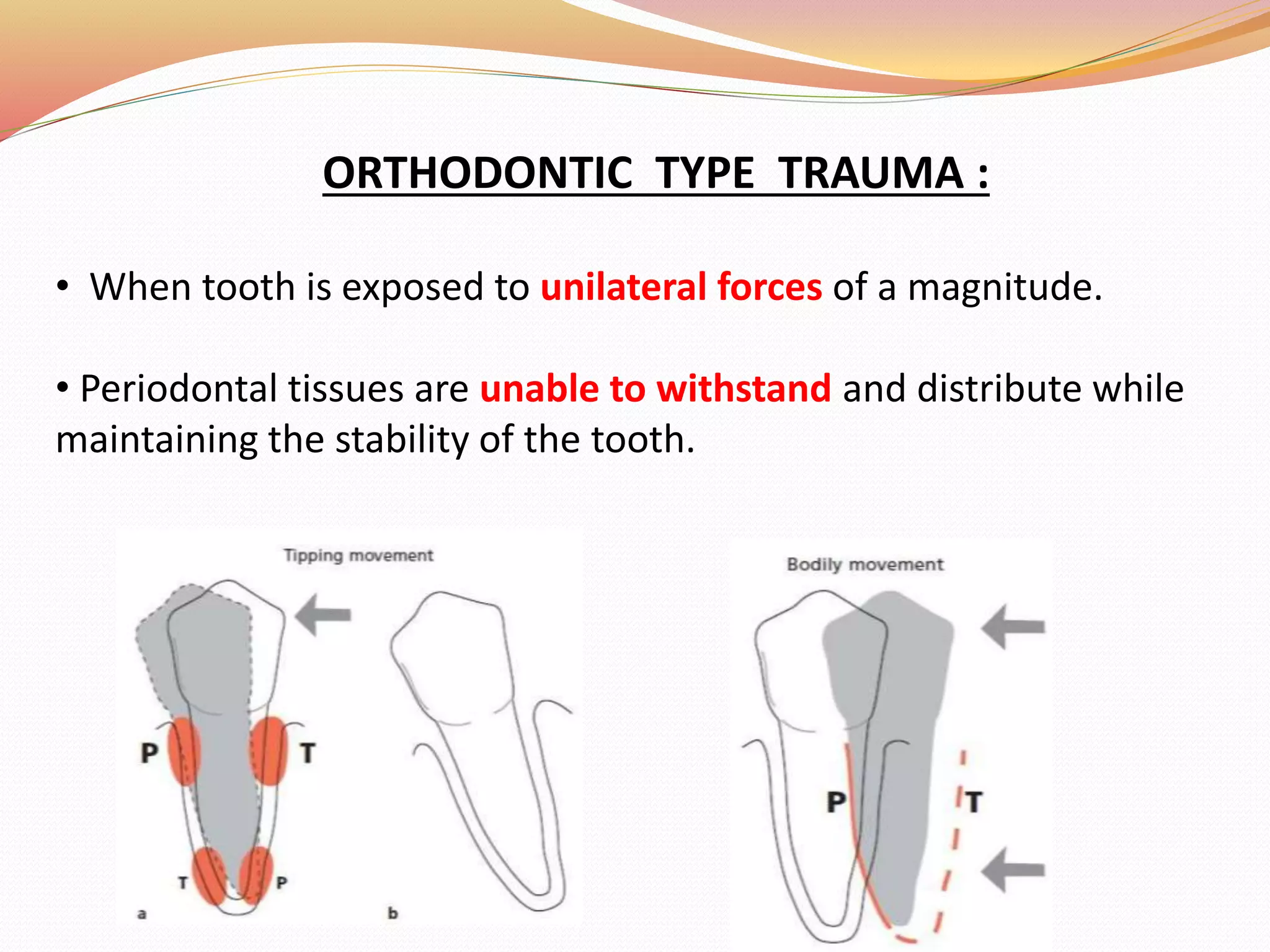
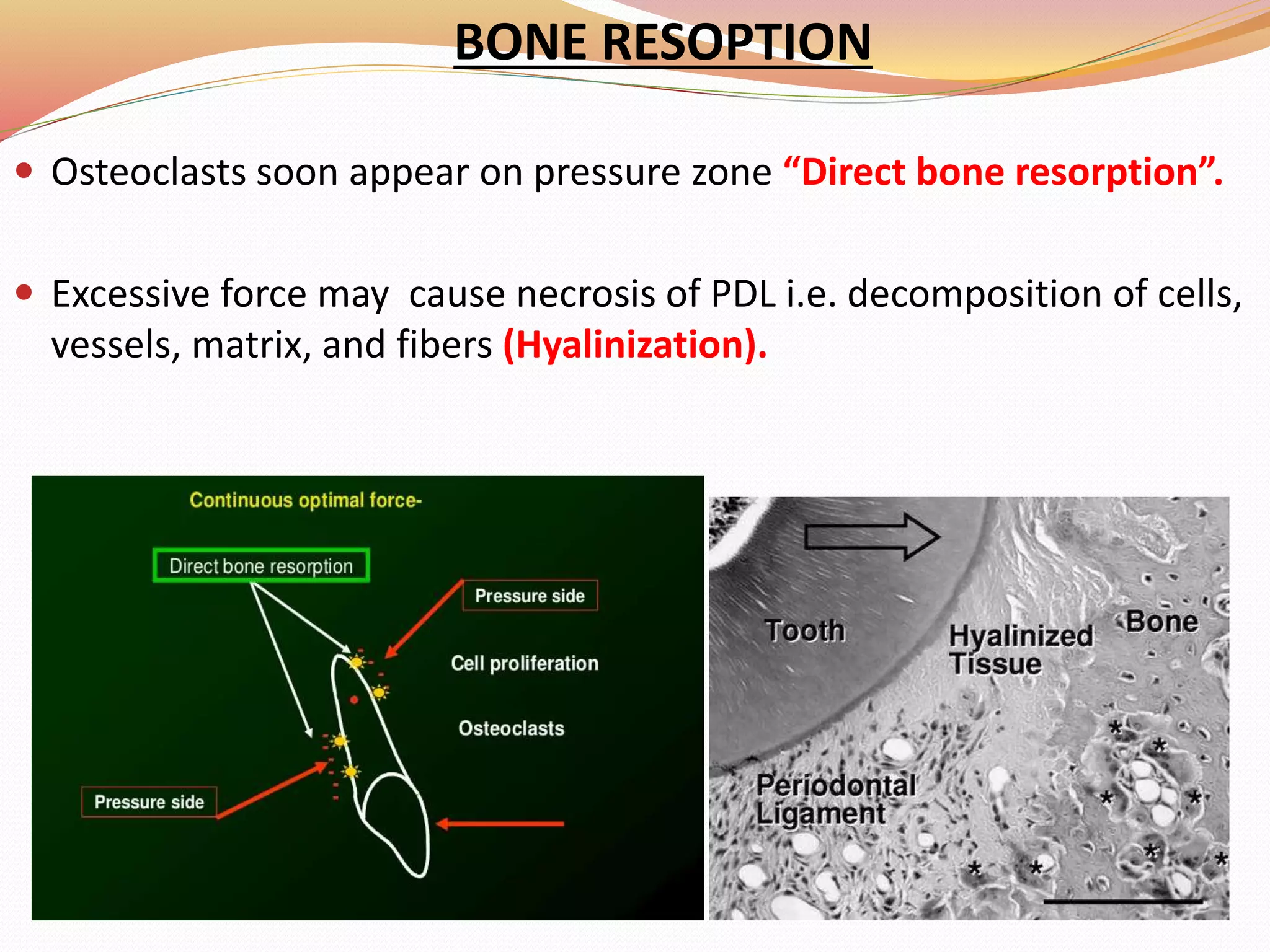
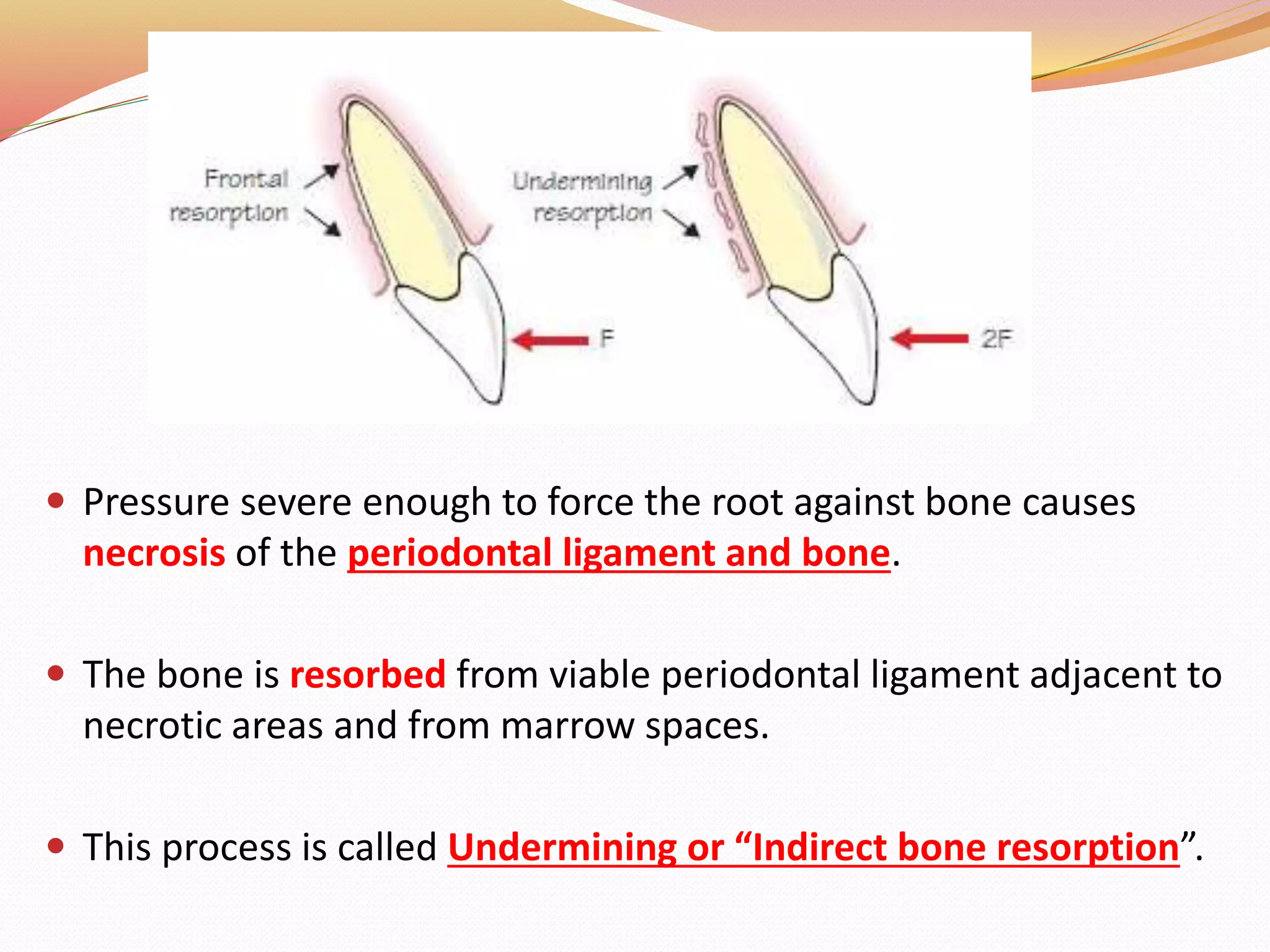
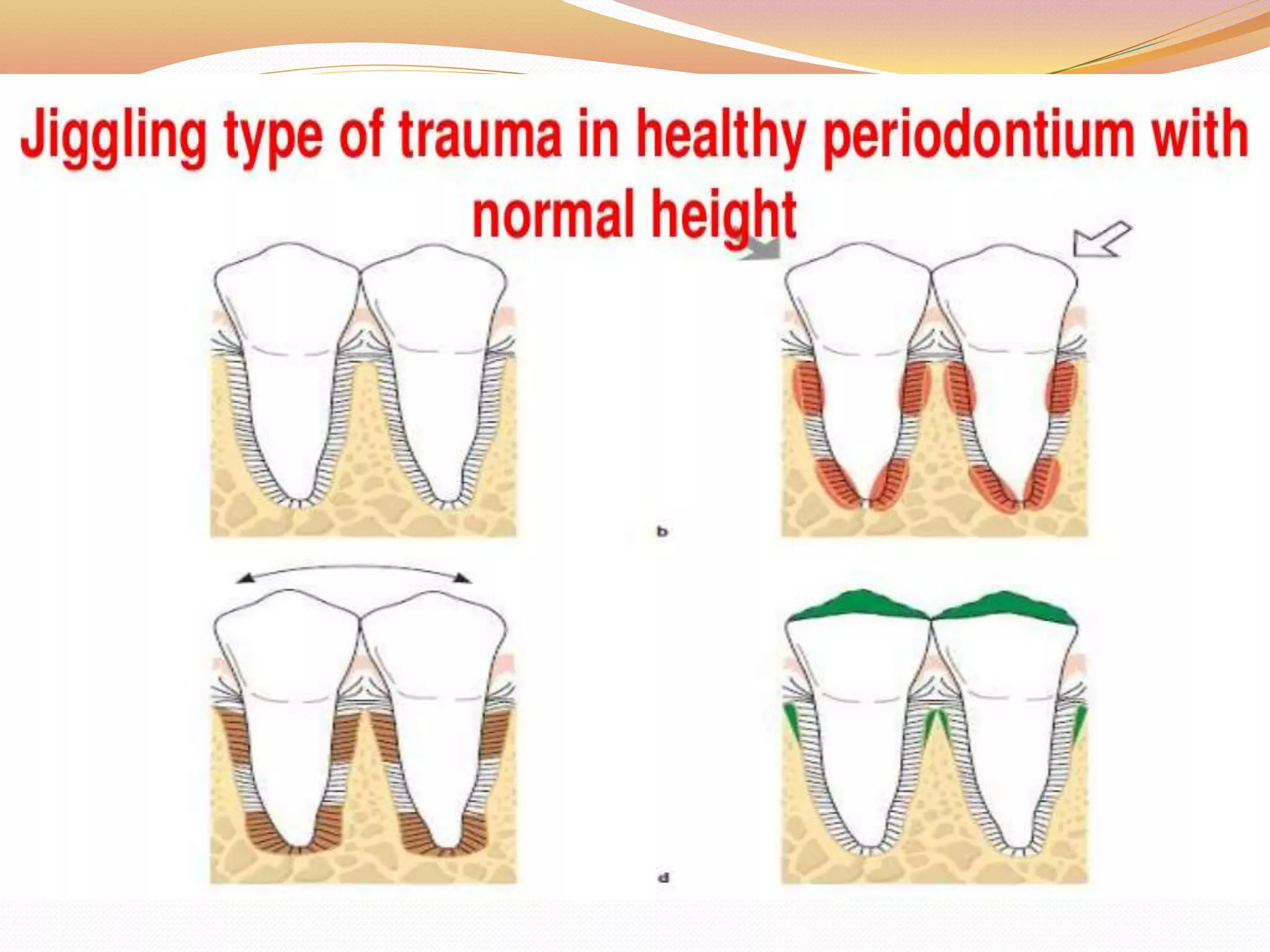
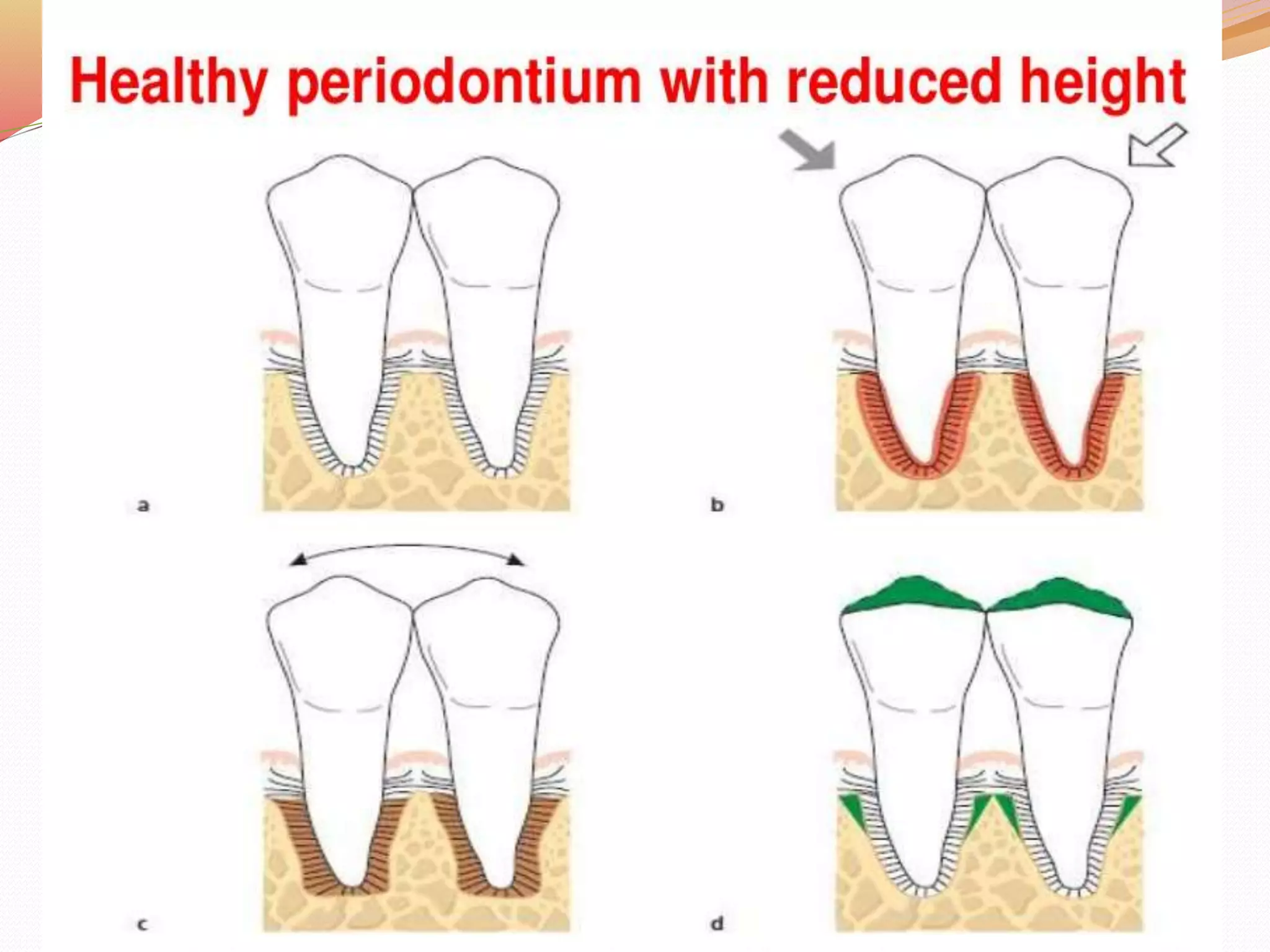
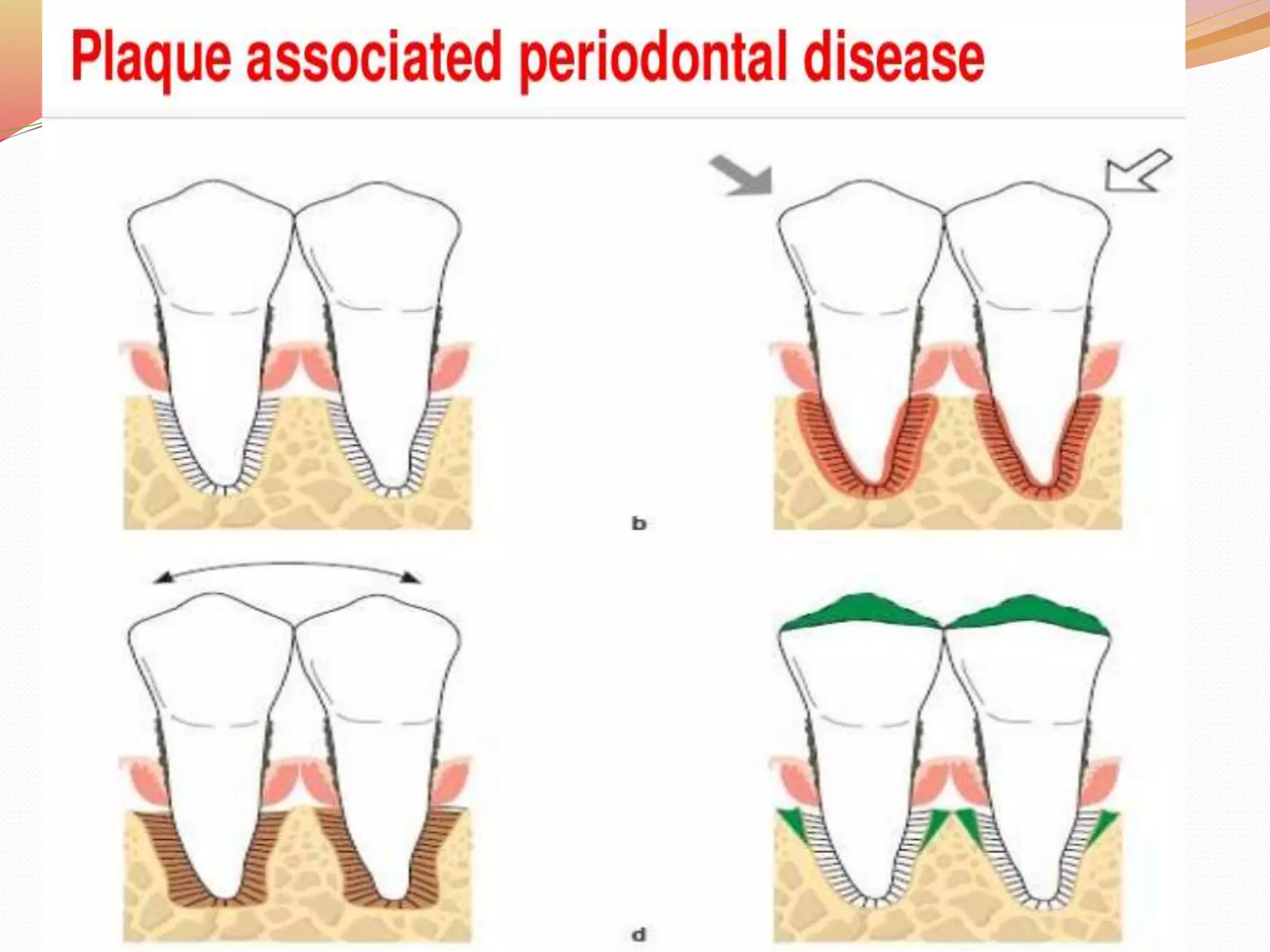
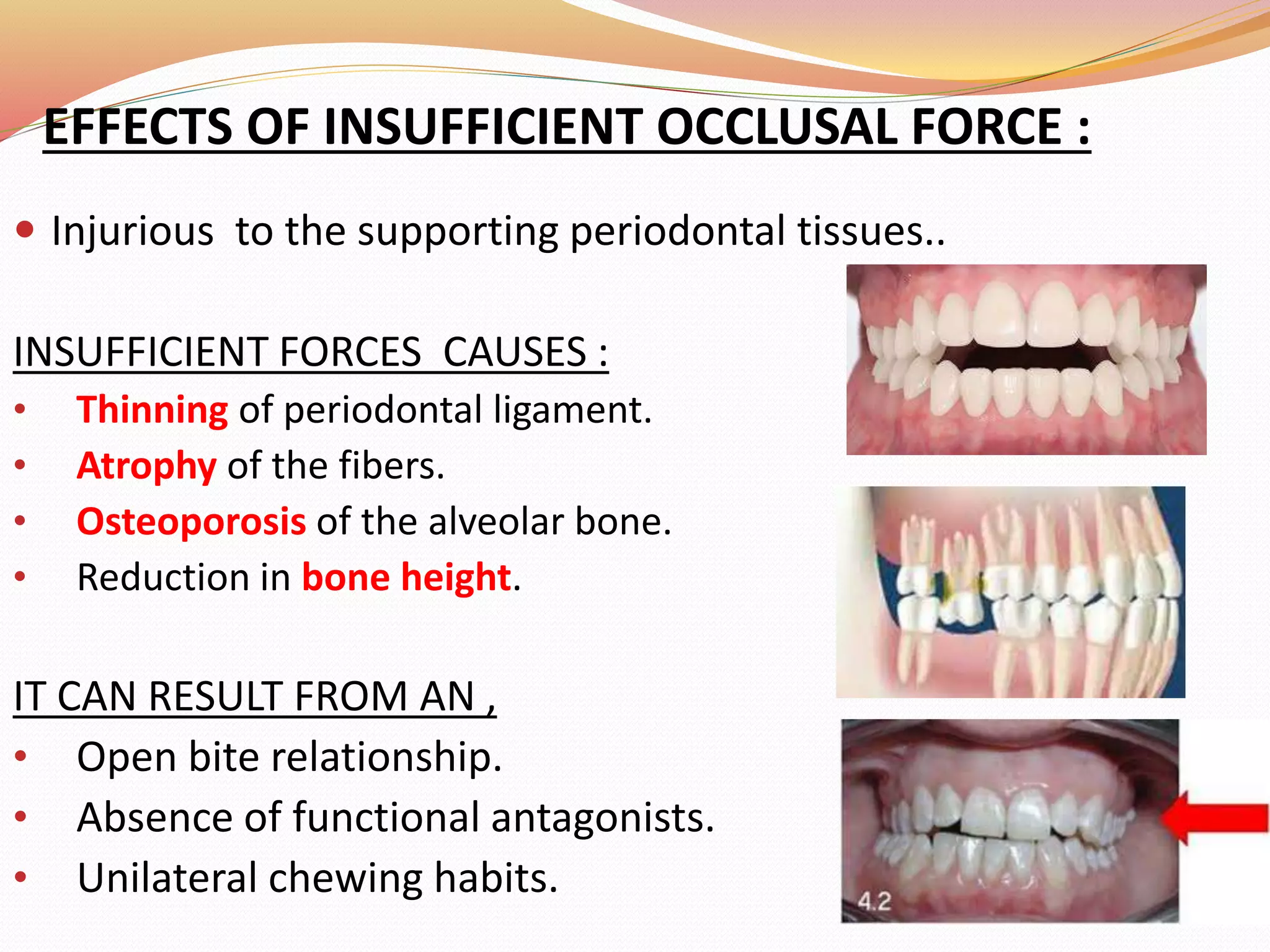
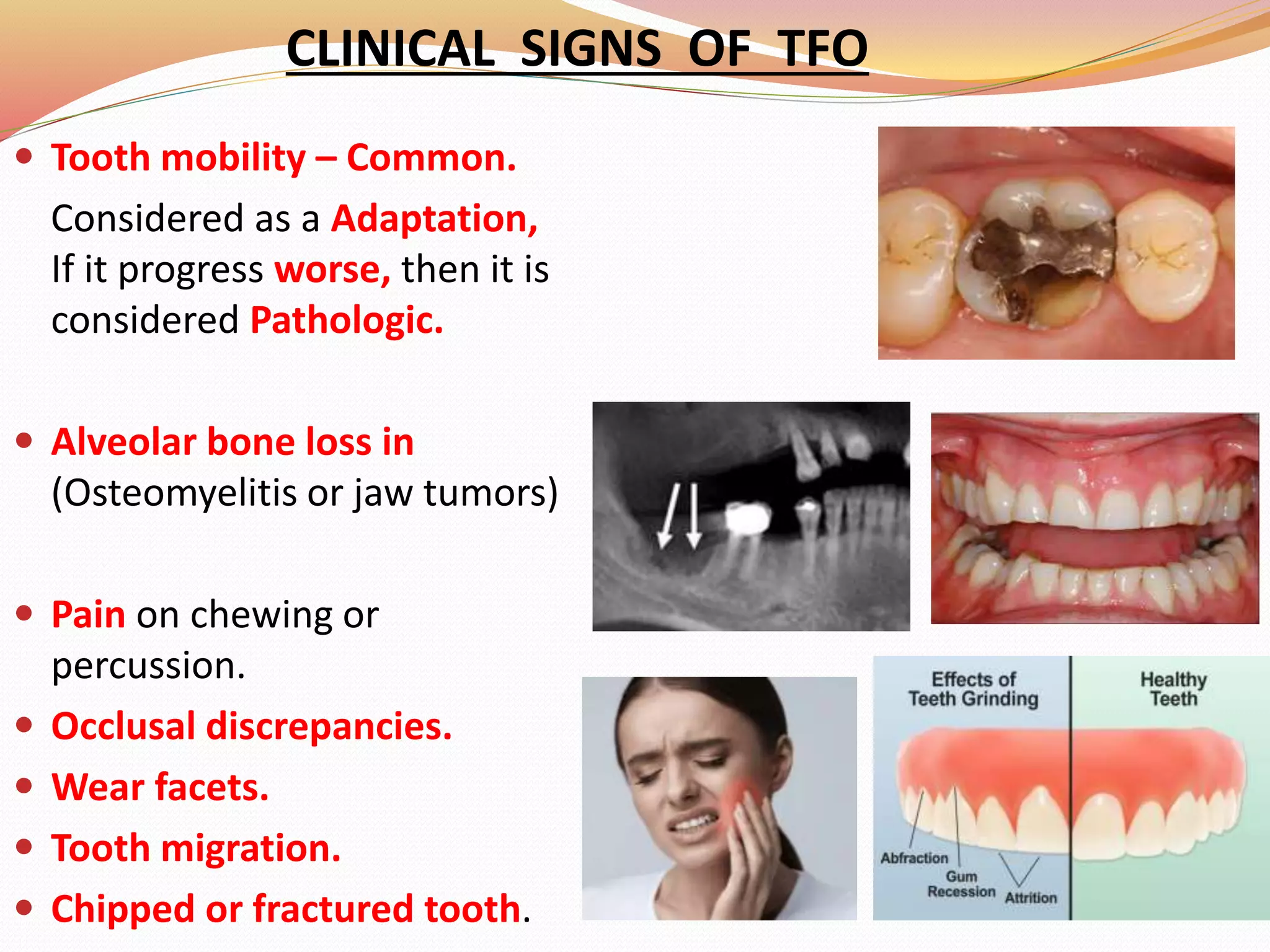
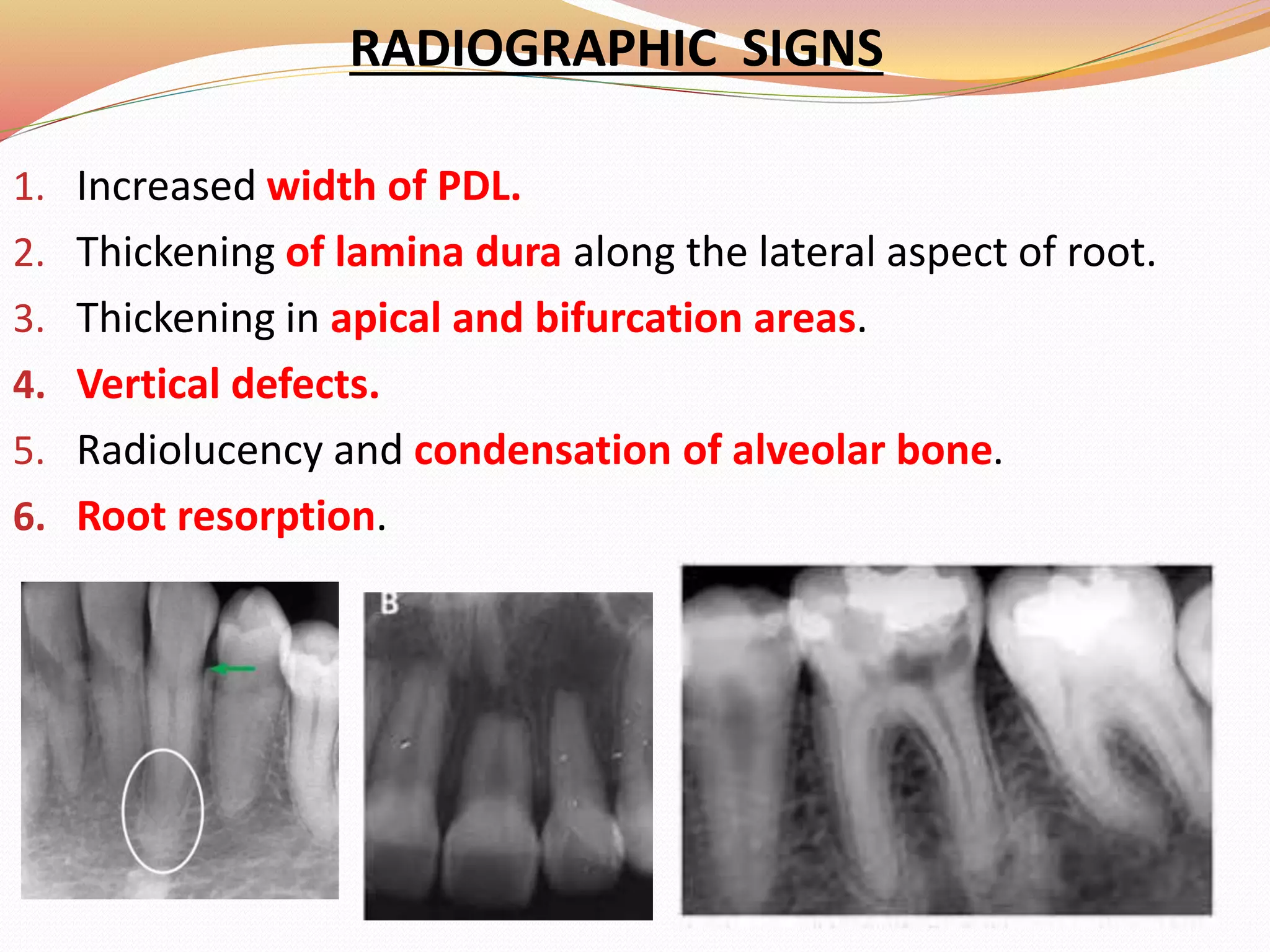
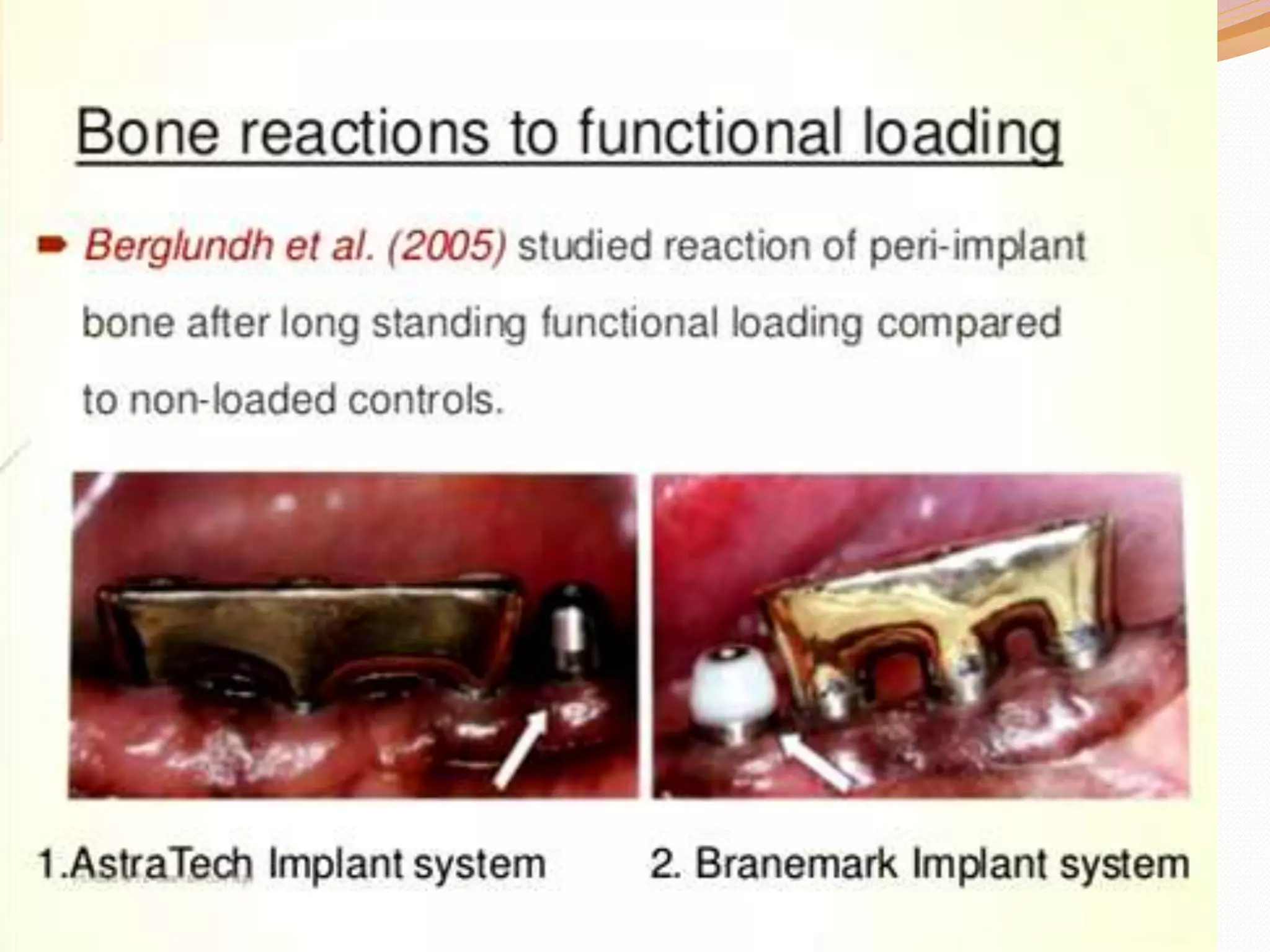
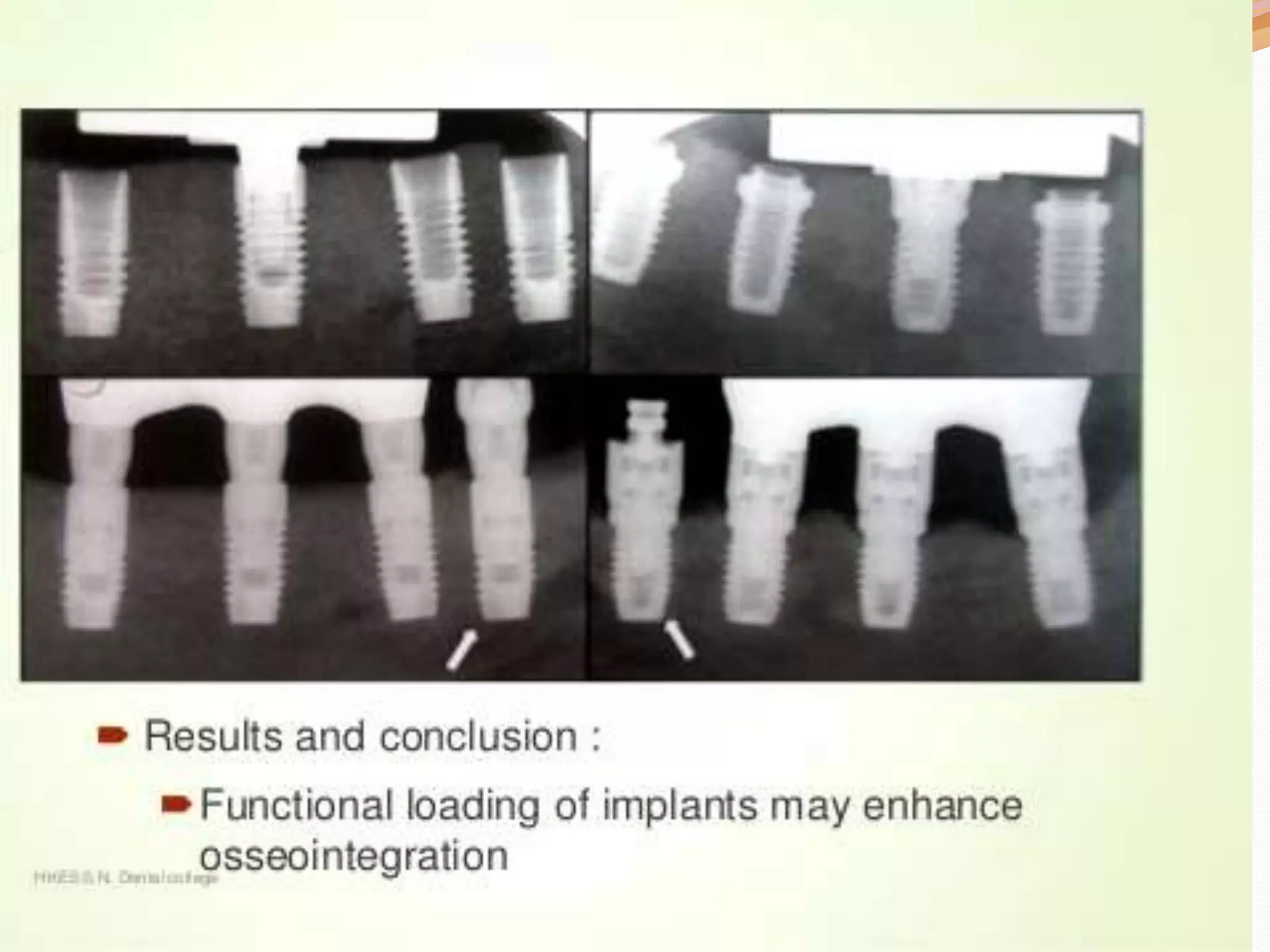
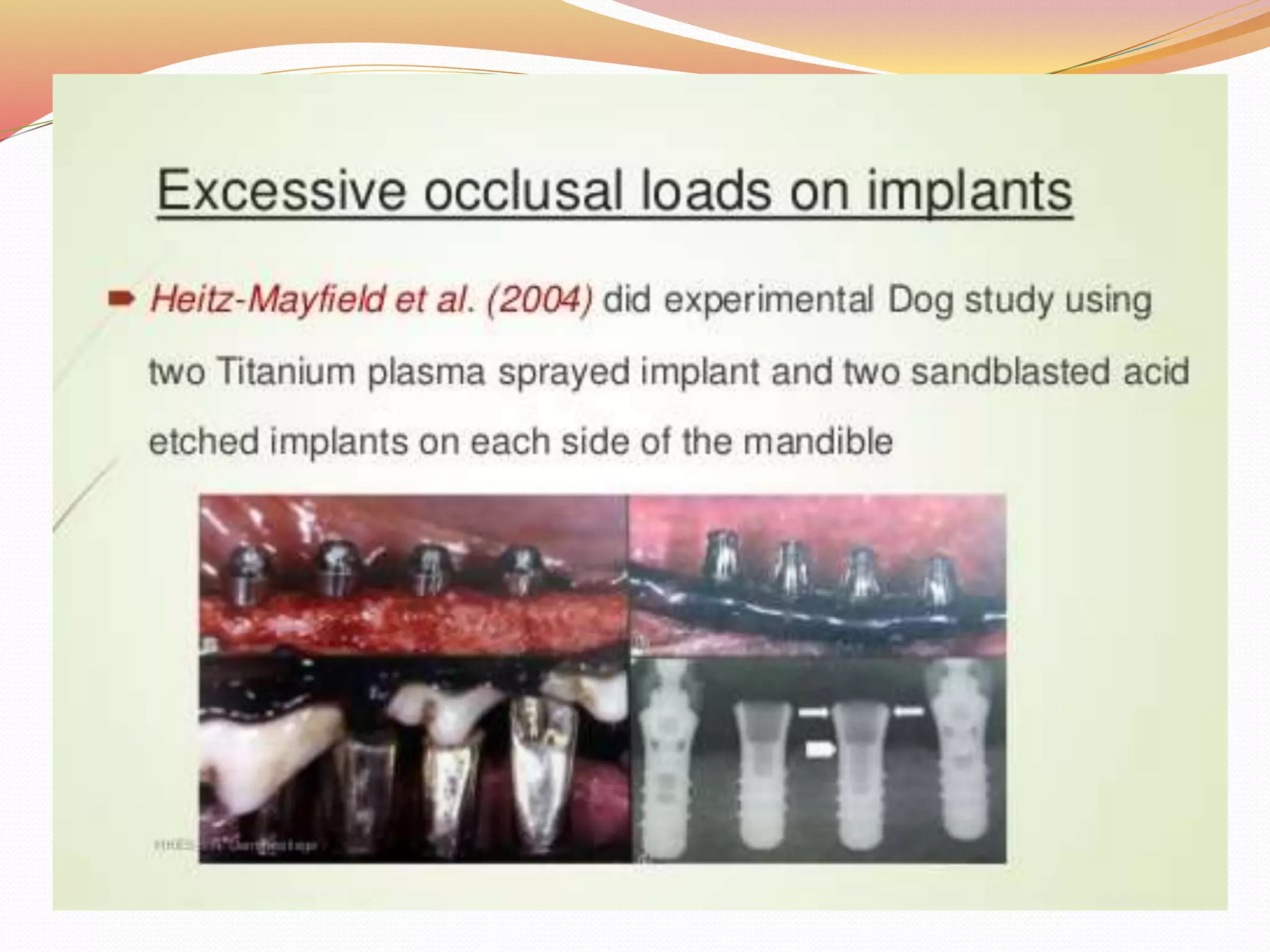
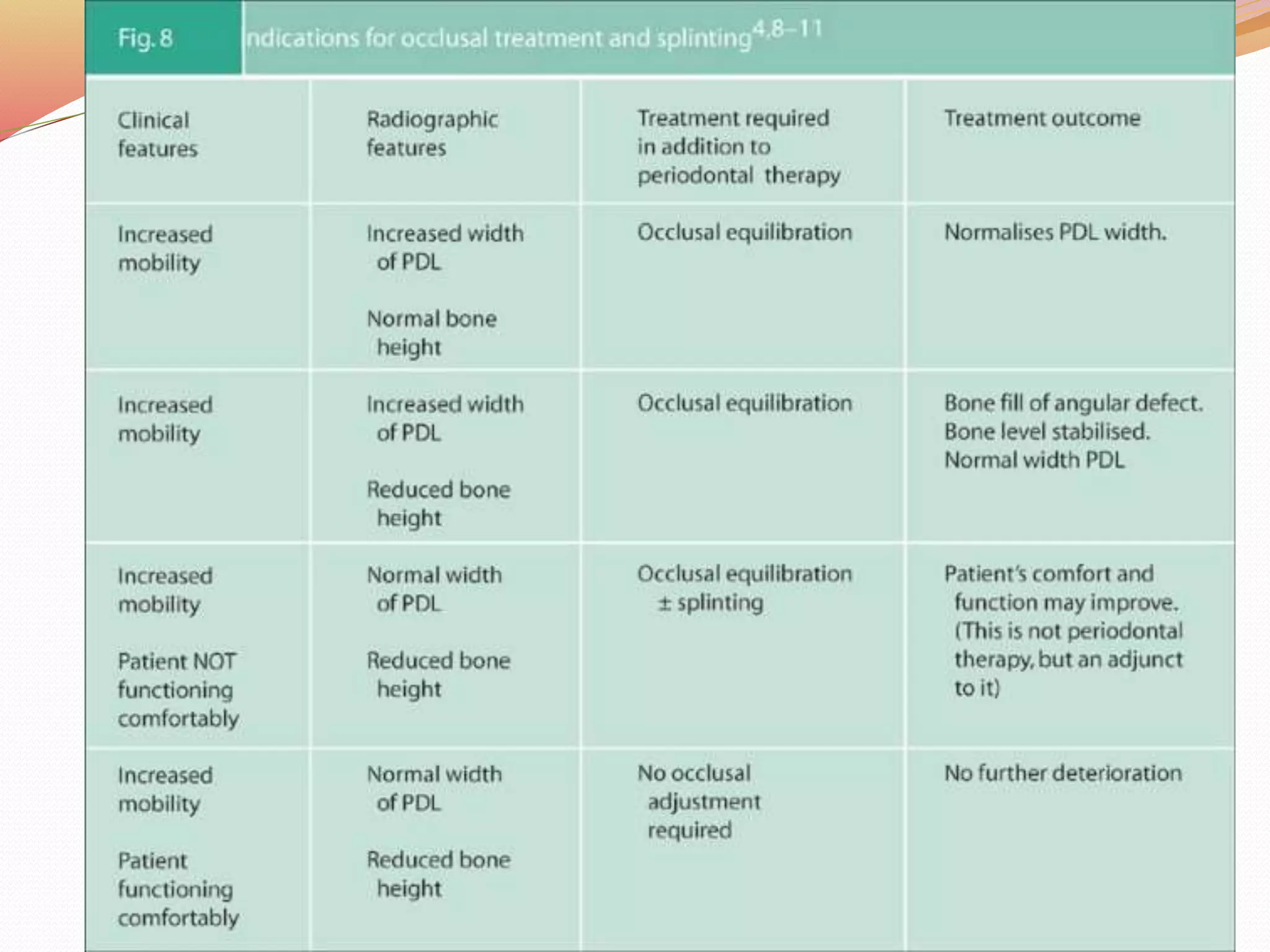
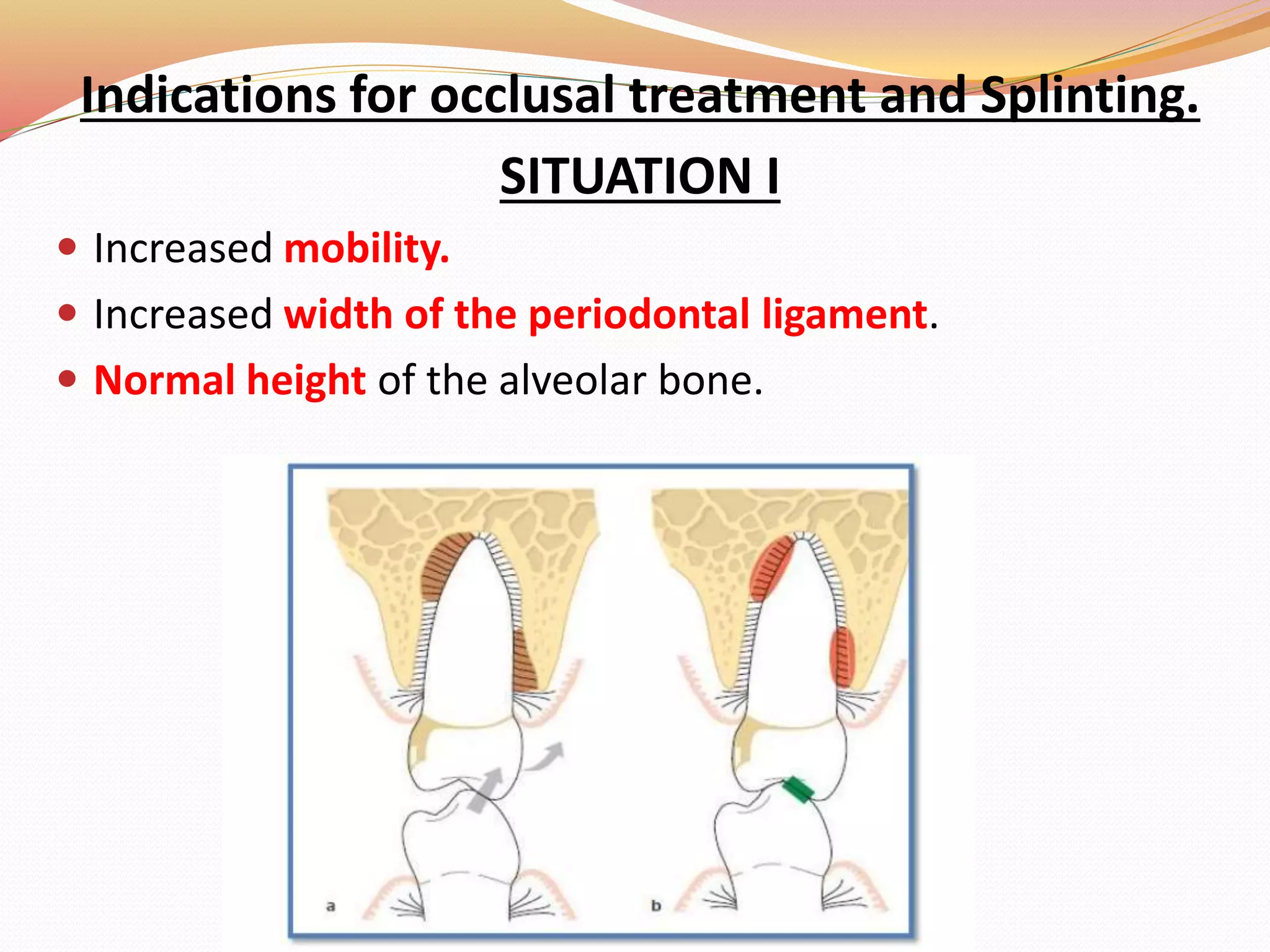
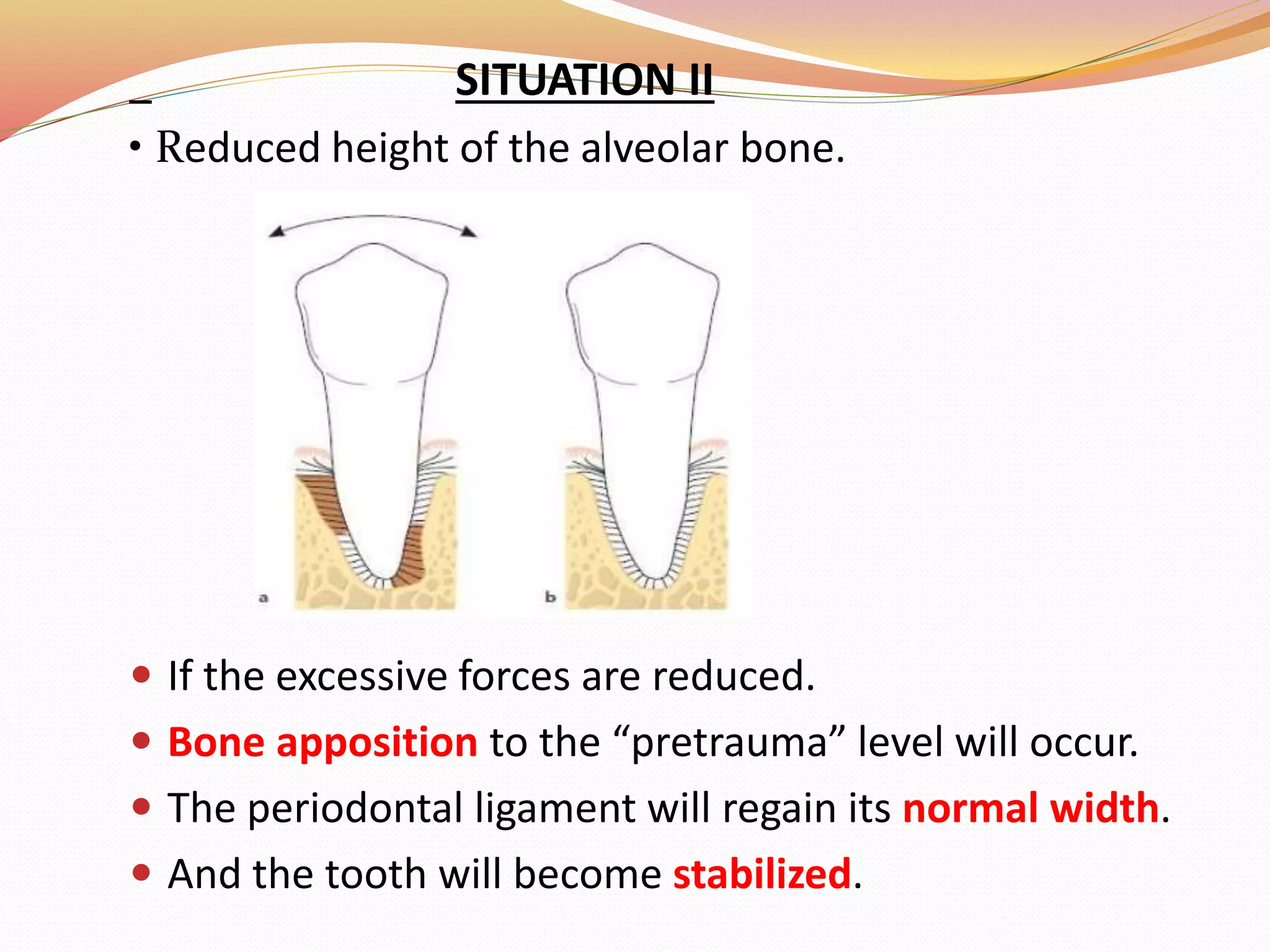
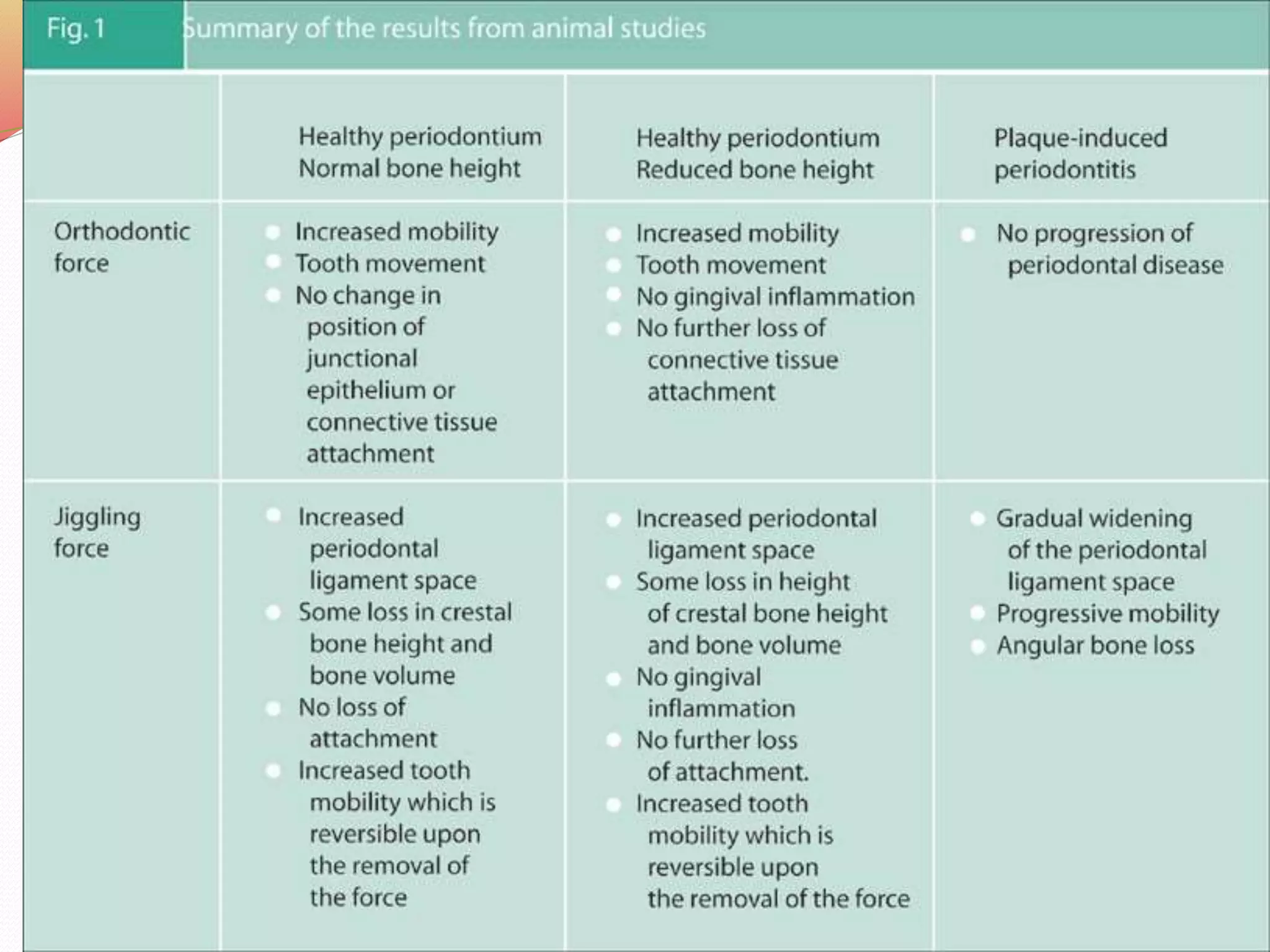
The document discusses occlusal trauma, emphasizing how excessive occlusal forces can lead to injury in the periodontal structures. It provides definitions, classification, clinical features, diagnosis methods, and stages of tissue response to injury related to occlusal trauma. The text also explores the relationship between occlusal trauma and periodontal diseases and outlines treatment considerations for managing these conditions.