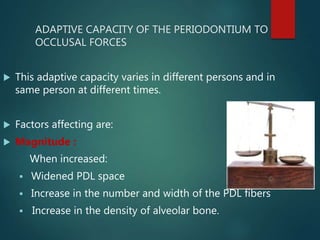
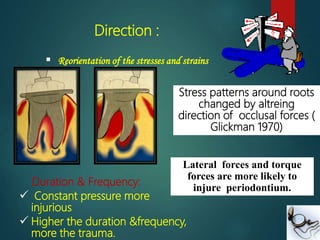
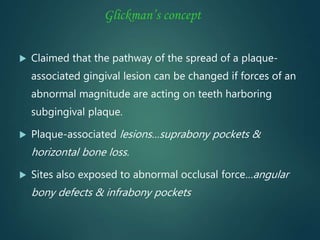
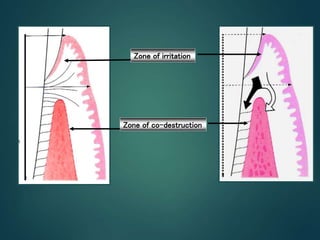
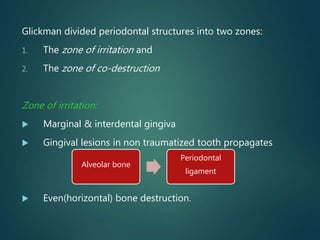
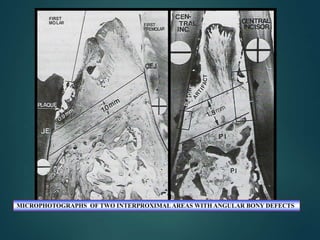
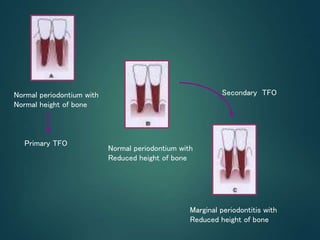
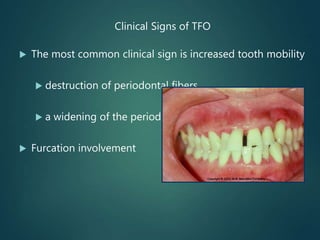
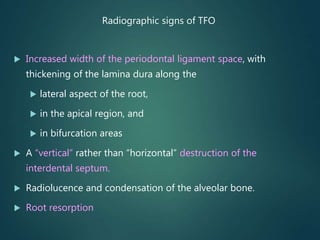
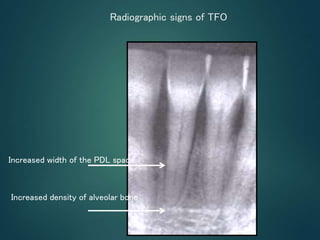
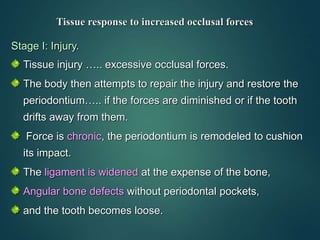
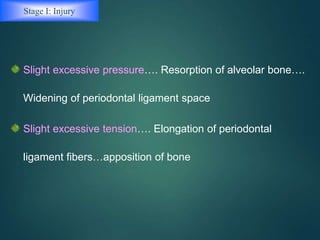
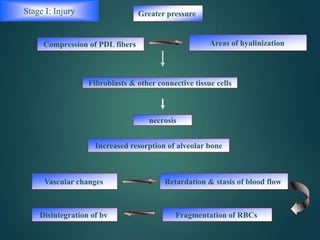
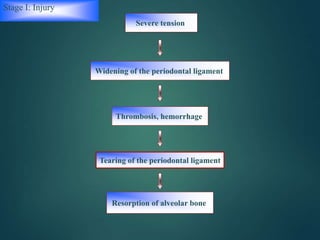
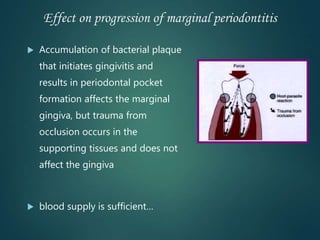
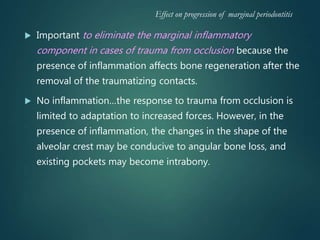
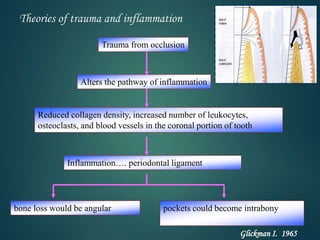
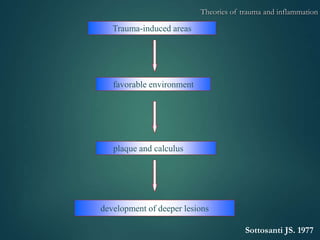
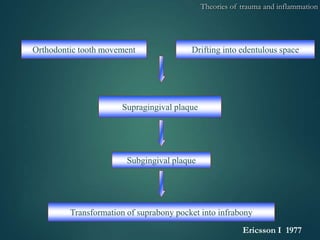
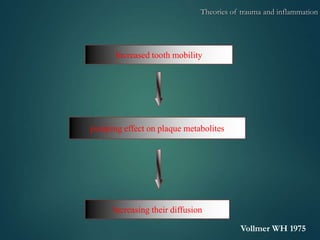
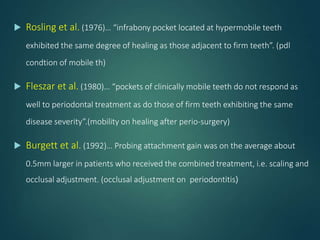
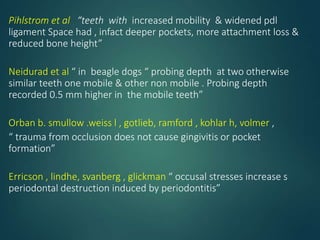
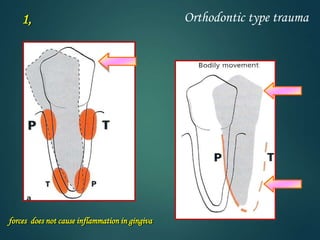
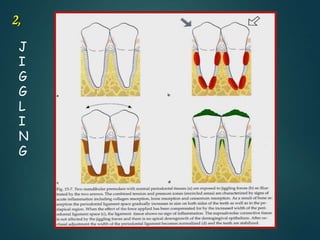
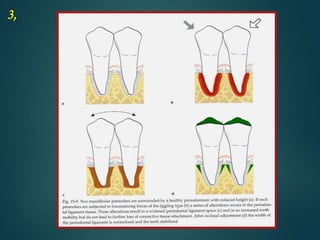
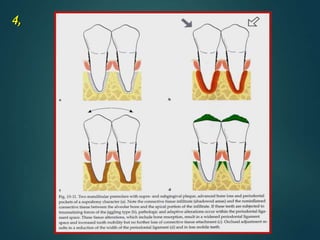
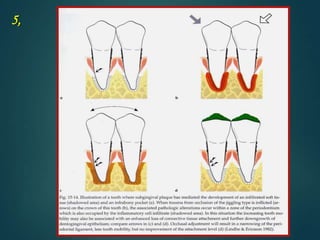
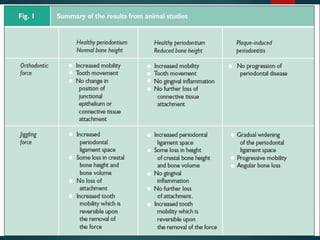
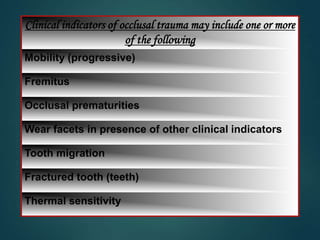
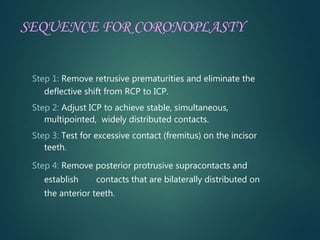
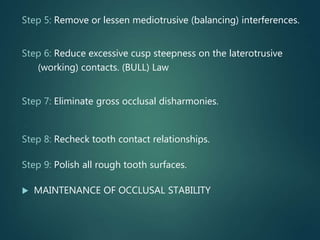
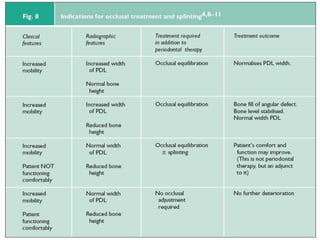
Trauma from occlusion occurs when excessive occlusal forces exceed the adaptive capacity of the periodontium, causing injury. It can be acute from a sudden impact or chronic from gradual changes in occlusion over time. Clinical signs include increased tooth mobility, bone loss, and widening of the periodontal ligament space seen radiographically. Theories suggest trauma alters the pathway of inflammation and may increase periodontal destruction. Treatment involves eliminating traumatic occlusal contacts through procedures like occlusal adjustment and splinting to allow the tissues to heal.