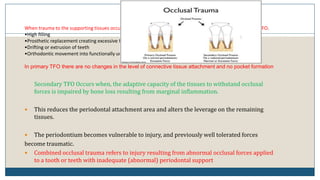
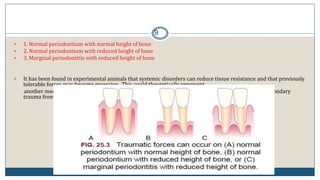
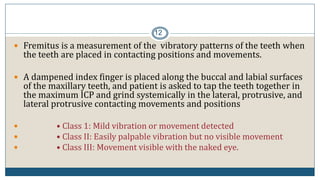
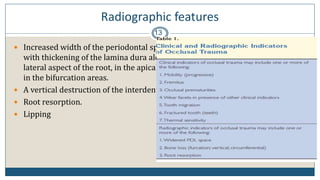
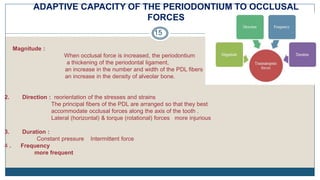
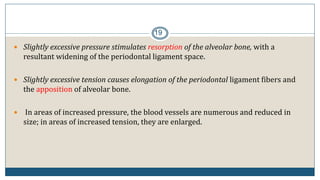
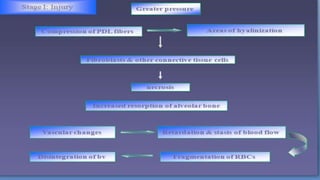
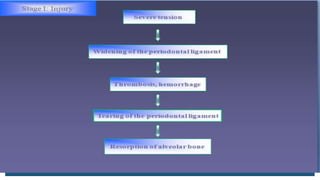
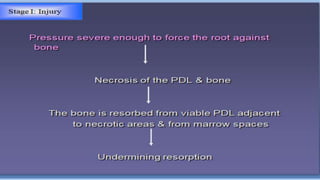
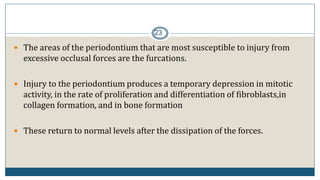
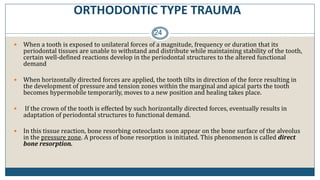
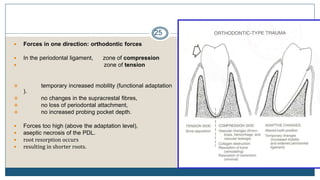
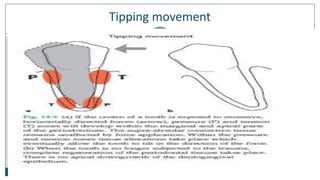
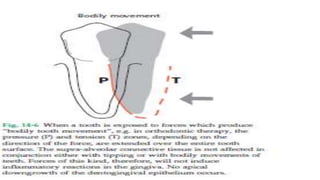
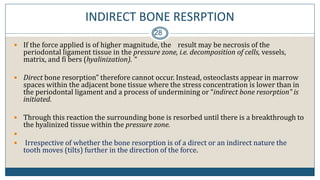
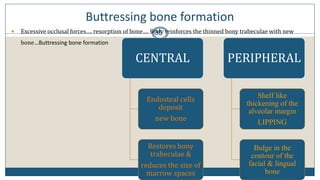
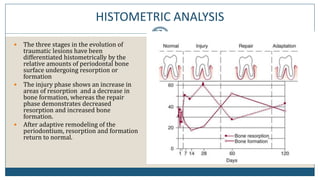
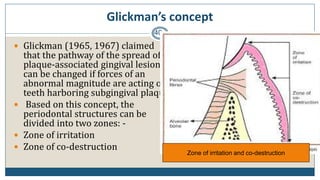
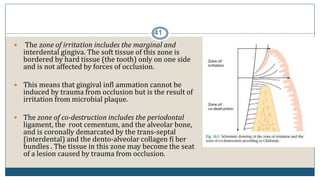
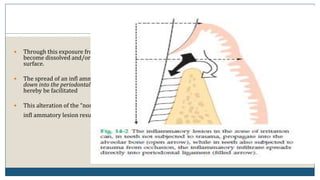
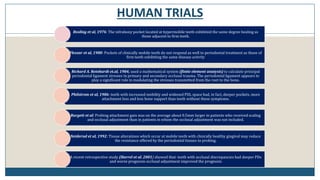
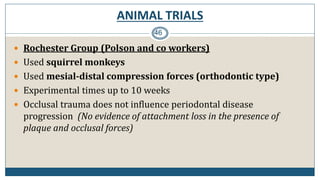
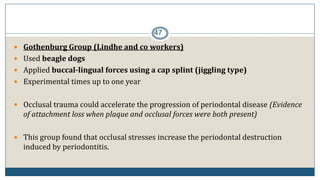
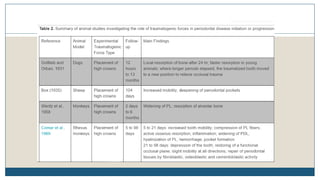
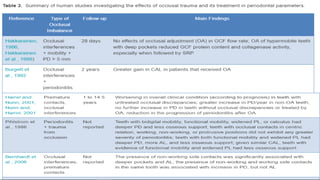
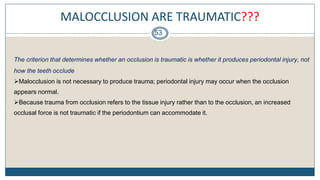
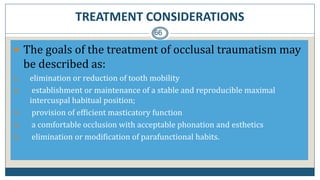
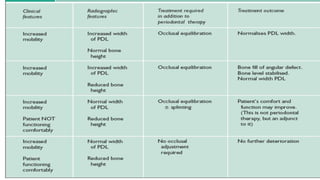
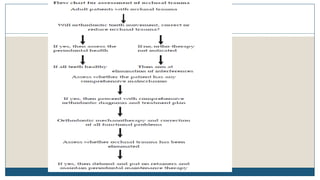
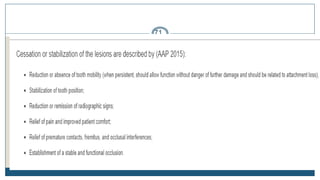
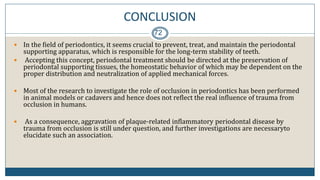
This document discusses trauma from occlusion (TFO), which refers to pathologic alterations or adaptive changes in the periodontium resulting from excessive occlusal forces. It covers the historical understanding of TFO, definitions, classifications, clinical features, and the periodontal response and adaptation to excessive forces. It also examines Glickman's concept of co-destruction between TFO and plaque-associated periodontal disease. The document provides details on injury, repair, remodeling processes in the periodontium in response to TFO.