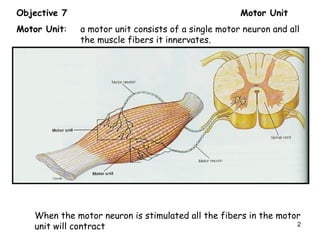
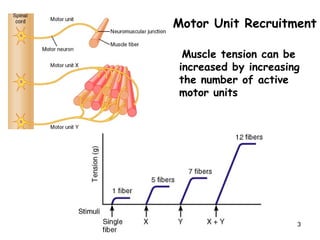
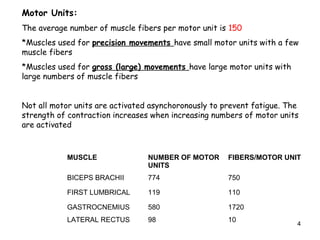
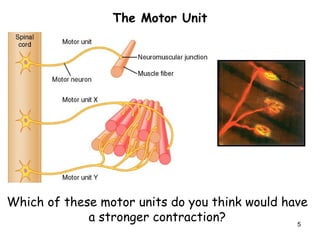
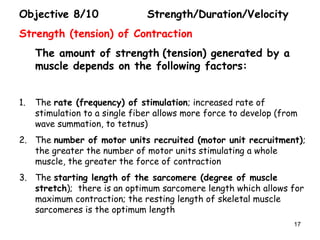
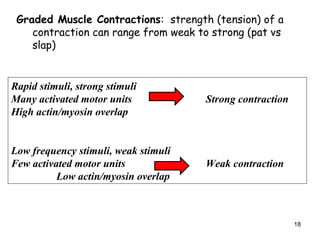
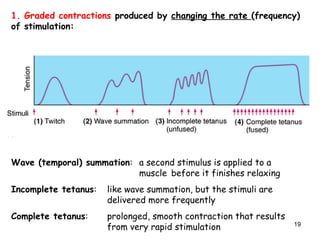
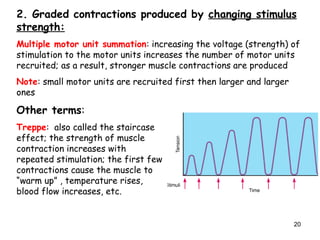
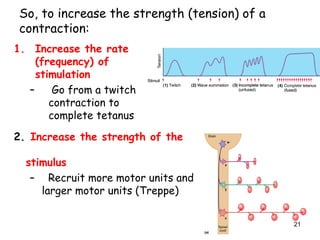
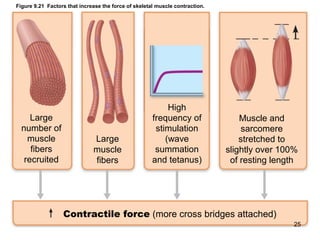
Motor units consist of a single motor neuron and the muscle fibers it innervates. Muscle tension can be increased by recruiting more motor units through increasing the rate and strength of stimulation. Muscles are made up of motor units of varying sizes, with small motor units having few fibers used for precision movements and large motor units having many fibers used for gross movements.