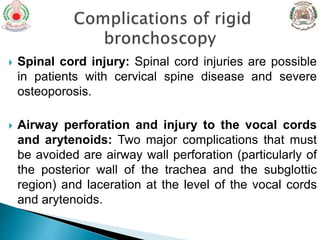
Rigid bronchoscopy is used to visualize the trachea and bronchi and manage airway obstructions. It has a large diameter that facilitates suctioning and removal of debris or placement of stents. It is commonly used for tumor debulking, foreign body removal, stent placement, and ablative treatments. Contraindications include cardiac issues, pulmonary issues, bleeding risks, and inability to cooperate. Direct intubation through the vocal cords using a rigid telescope is preferred but laryngoscopy can also be used. Intubation through an existing tracheostomy is also possible. Complications include hypoxemia, trauma, and swelling. Careful technique is needed to avoid injuries.