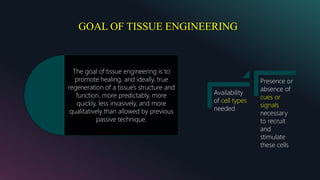
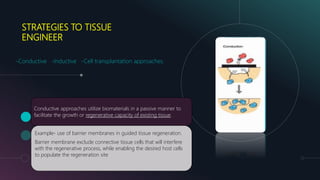
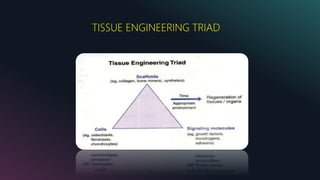
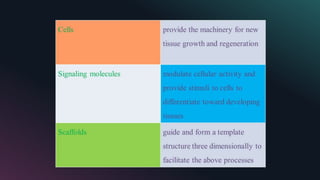
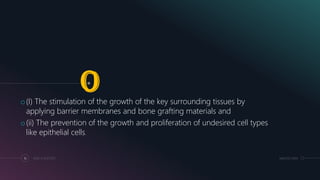
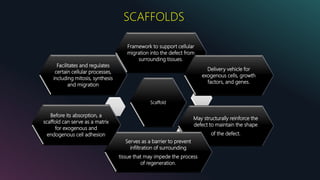
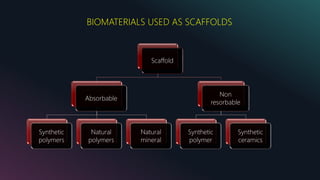
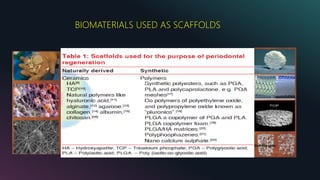
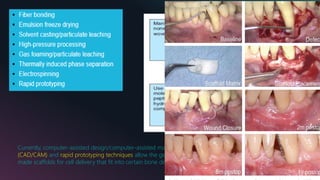
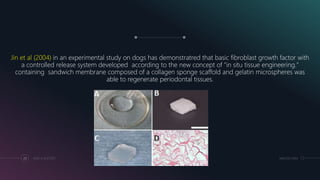
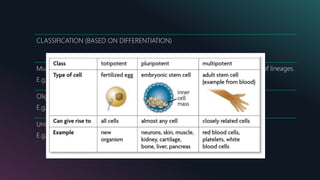
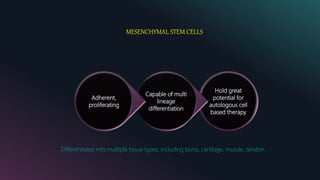
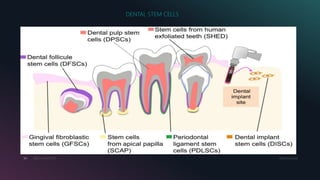
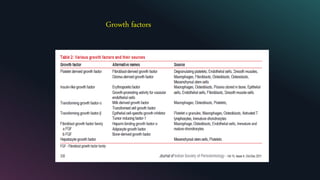
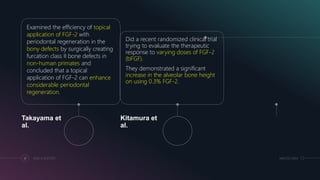
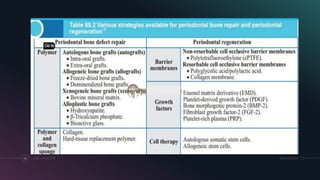
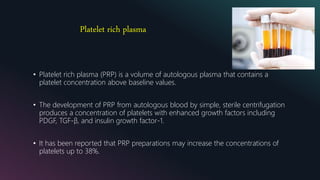
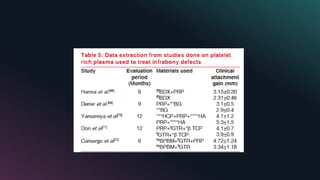
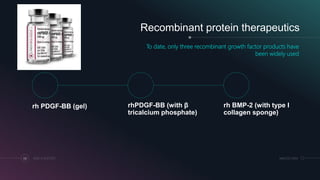
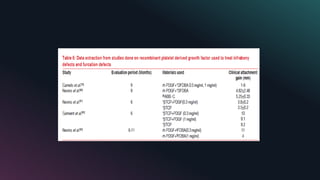
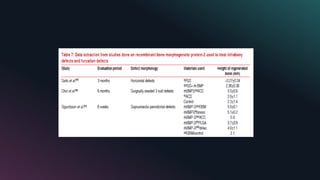
This document provides an overview of tissue engineering as it relates to periodontal regeneration. It discusses the historical perspective of tissue engineering and need for strategies to regenerate lost periodontal tissues. Current strategies employed include using scaffolds, growth factors, and stem cells. Scaffolds provide a framework for cellular migration and integration. Sources of cells for tissue engineering include mesenchymal stem cells and various dental stem cells. Growth factors that have potential for periodontal regeneration include PDGF, IGF, TGF-β, and FGF. Future research directions include whole tooth regeneration using dental progenitor cells and scaffolds.