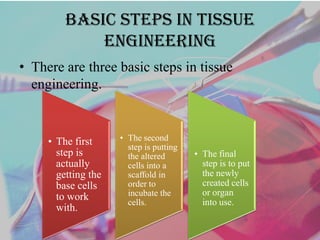
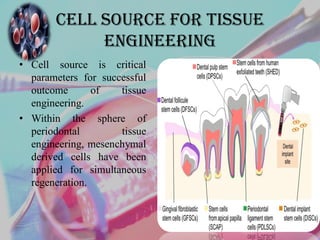
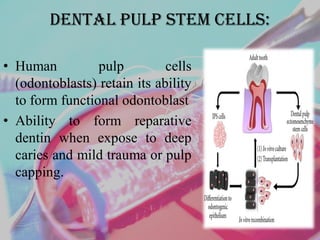
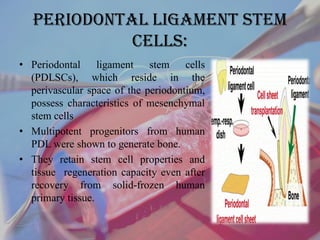
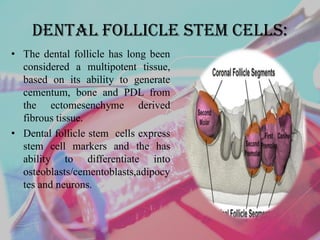
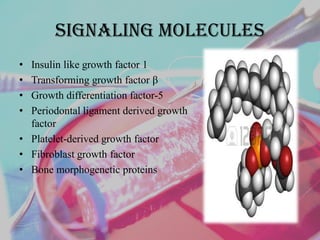
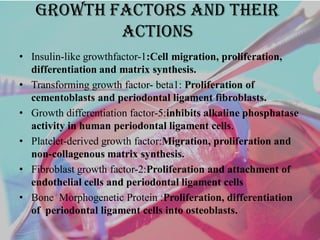
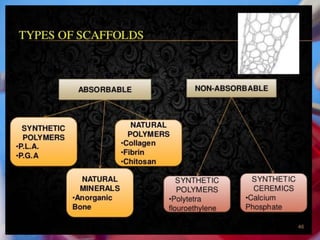
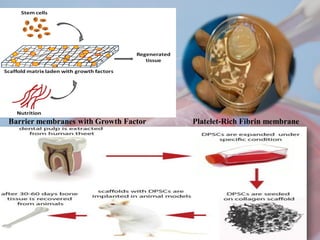
Tissue engineering aims to recreate healthy tissues to replace diseased or damaged ones. There are three basic steps: obtaining cells, putting them on a scaffold to incubate, and implanting the new tissue. Sources for periodontal tissue engineering include dental pulp stem cells, periodontal ligament stem cells, and dental follicle stem cells. Signaling molecules like growth factors are incorporated into scaffolds to facilitate their sustained release and support cell proliferation and differentiation. Scaffolds provide a structure for cell adhesion, migration, and production of extracellular matrix. Recent advances include antimicrobial and bioactive membranes, electrospun membranes, and platelet-rich fibrin membranes. Tissue engineering opens new possibilities for periodontal regeneration and restoration of oral function.