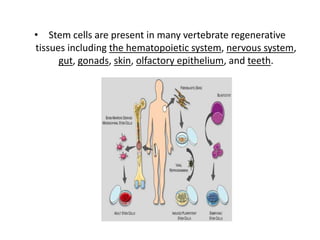
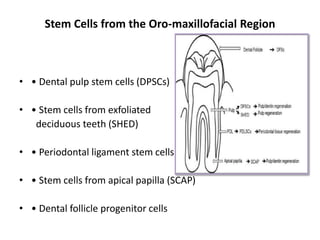
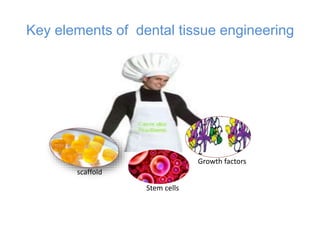
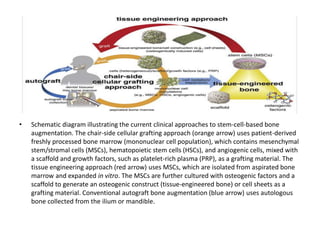
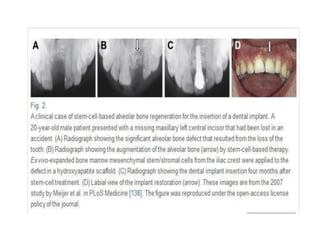
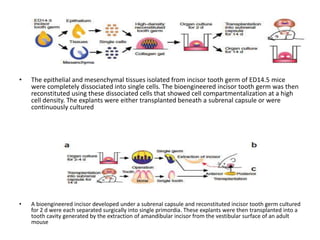
Stem cells have potential applications in dentistry for tissue regeneration. There are several types of stem cells, including embryonic, adult, and induced pluripotent stem cells. Dental tissues contain stem cells that are advantageous for use due to high plasticity and ability to be cryopreserved. Current approaches to stem cell therapy include using stem cells from sources like bone marrow or dental pulp to regenerate bone or develop cell sheets. Research aims to regenerate whole teeth by transplanting bioengineered tooth units constructed from epithelial and mesenchymal stem cells into defects. These techniques could help with problems like root regeneration and prosthodontic treatments.