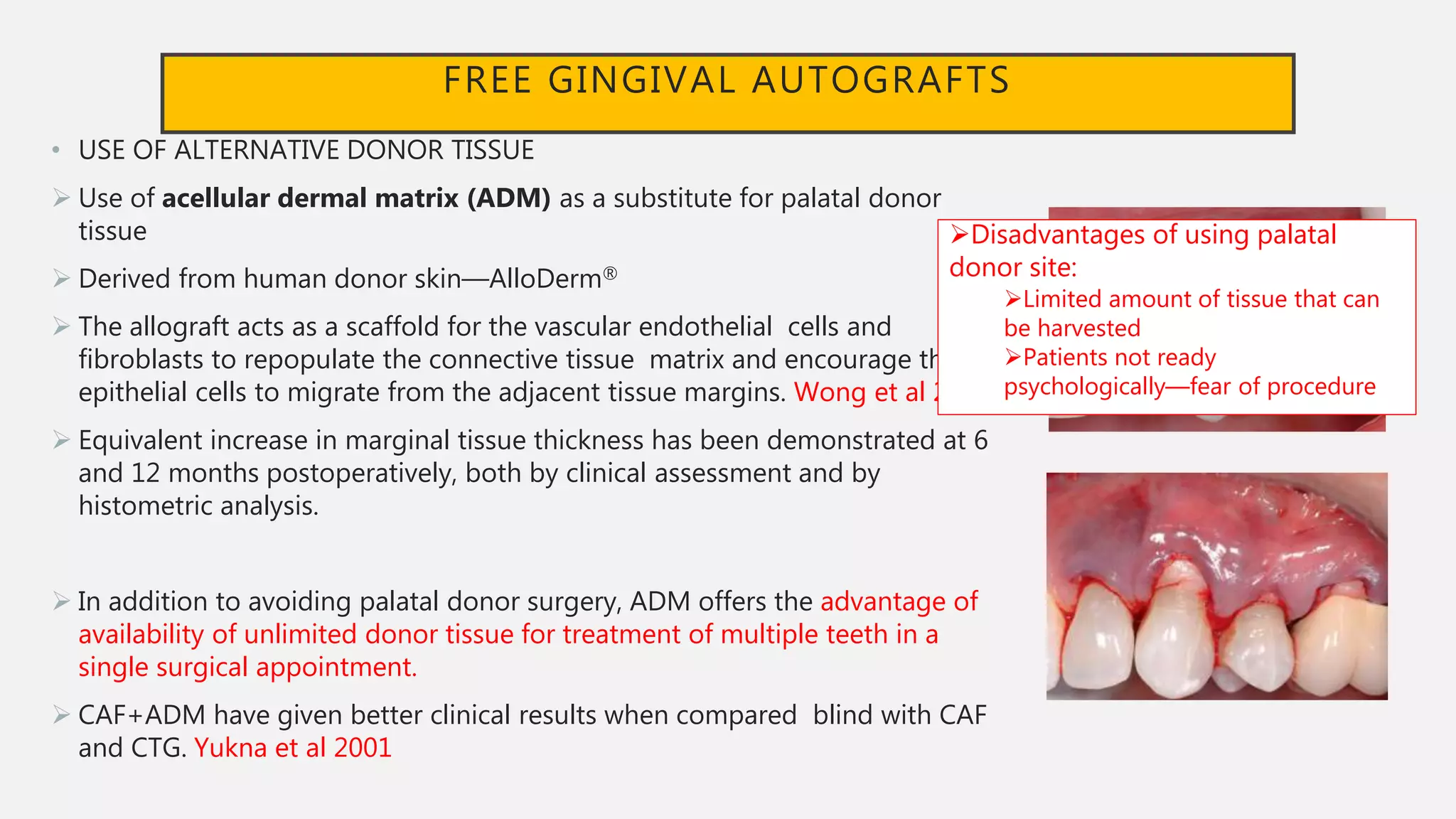
This document provides an overview of periodontal plastic surgeries, specifically focusing on gingival recession and methods to increase the width of attached gingiva. It begins with definitions and classifications of gingival recession. Objectives, indications, and concepts like the tissue barrier are discussed. Decision trees and criteria for selecting techniques are presented. Main techniques to increase the width of attached gingiva like free gingival grafts and connective tissue grafts are described, including variations and the use of alternative donor tissues. Healing processes are summarized. The document provides foundational information on periodontal plastic surgery procedures for gingival recession and attached gingiva augmentation.