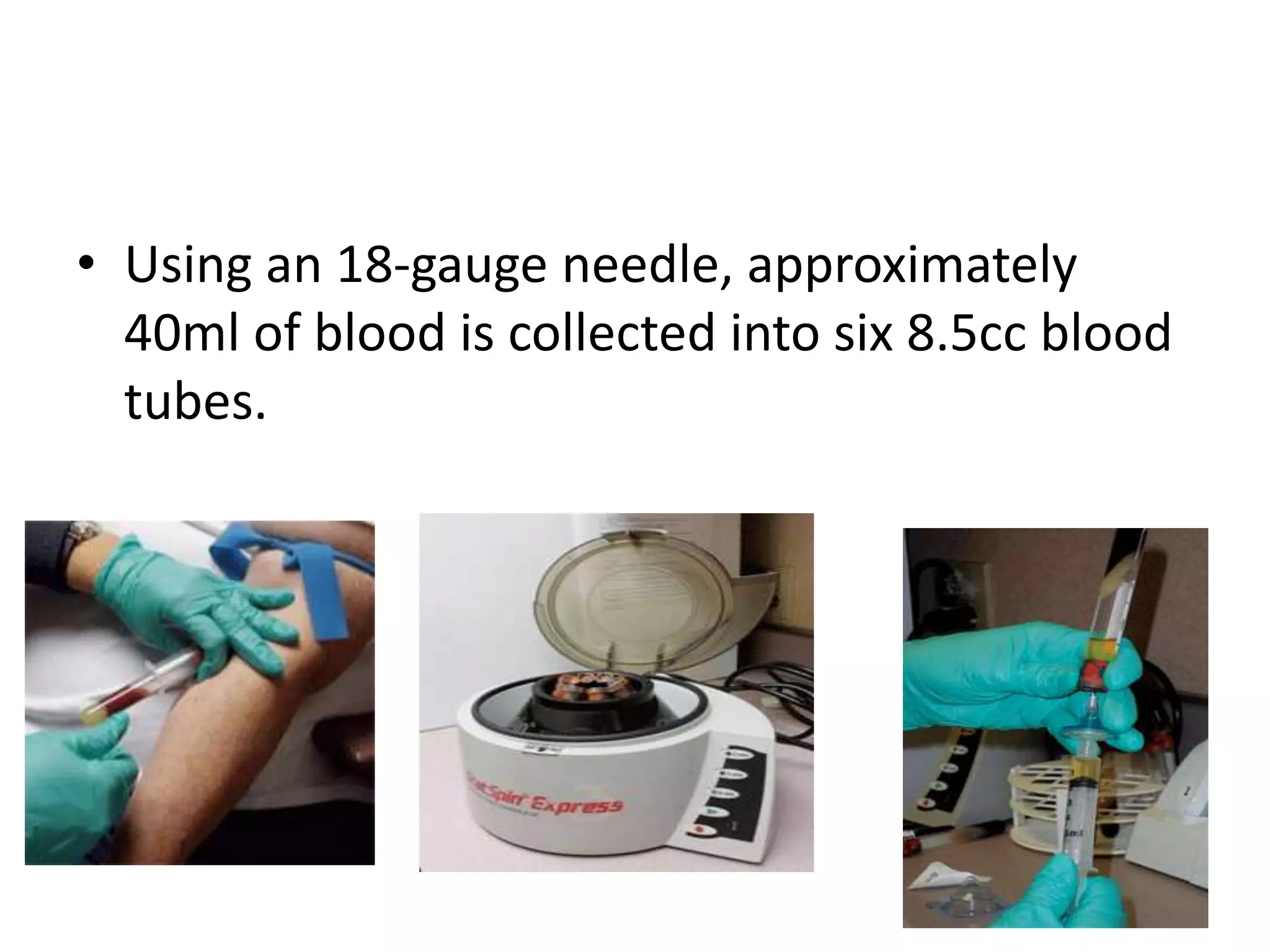
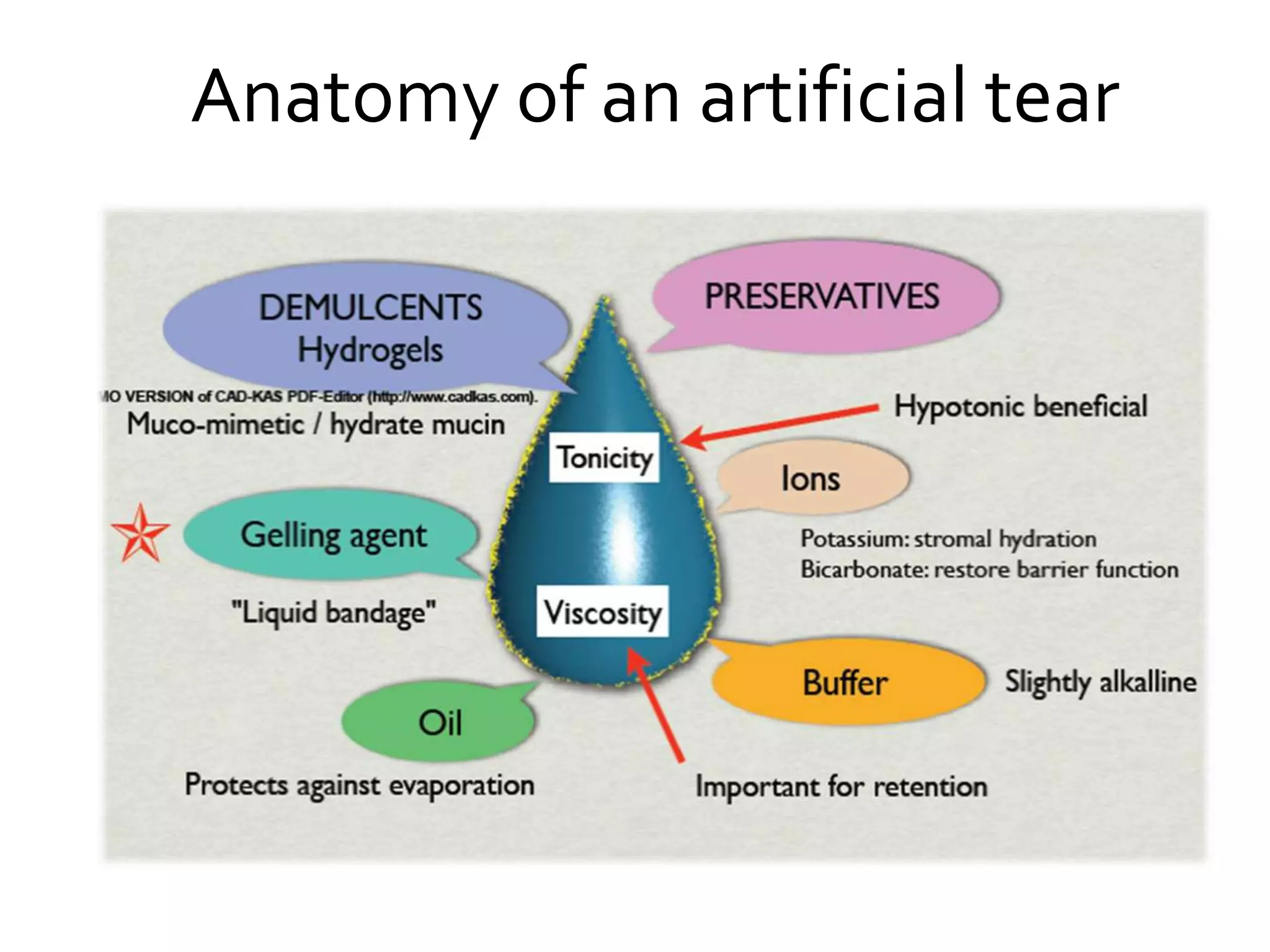
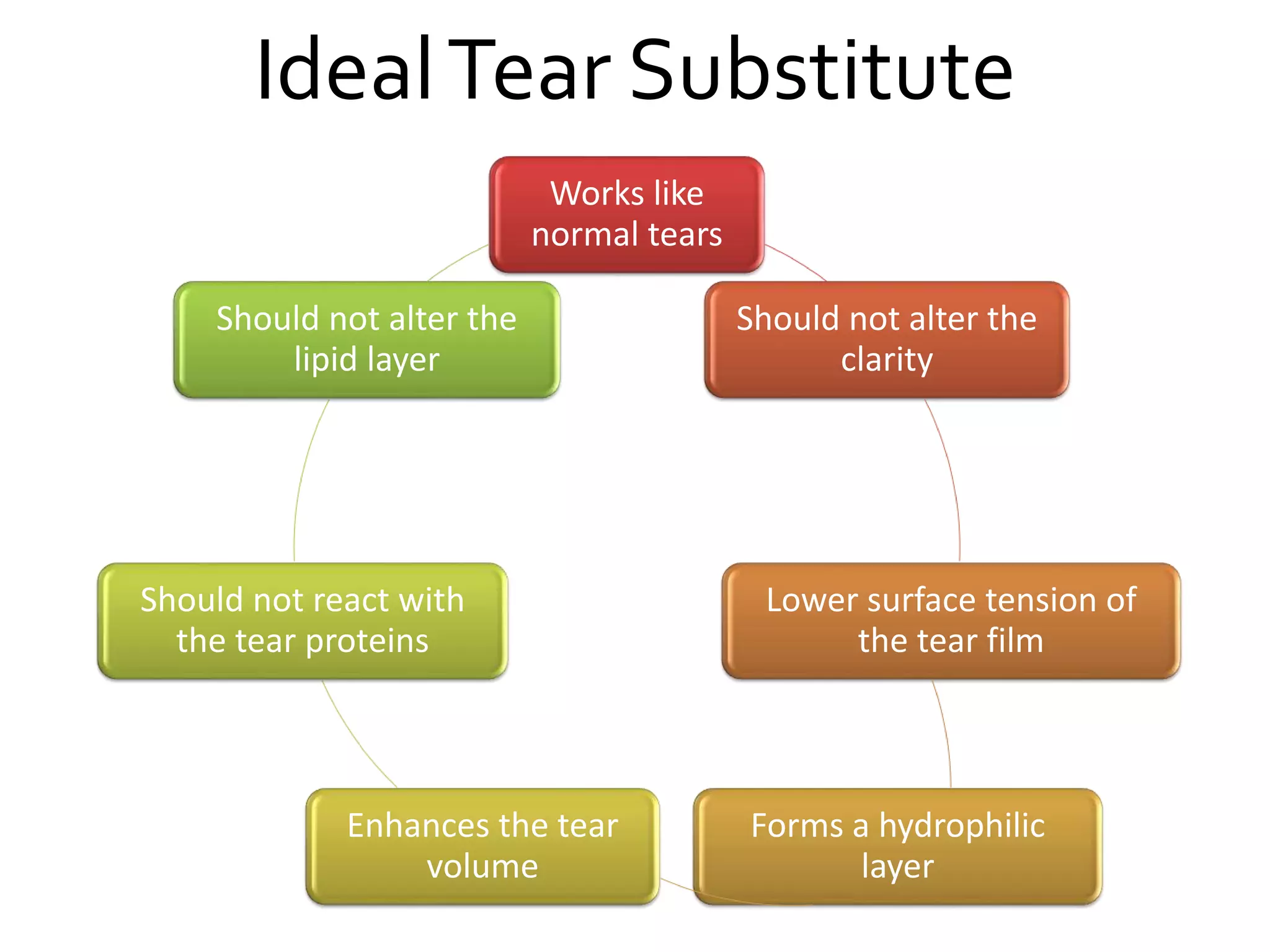
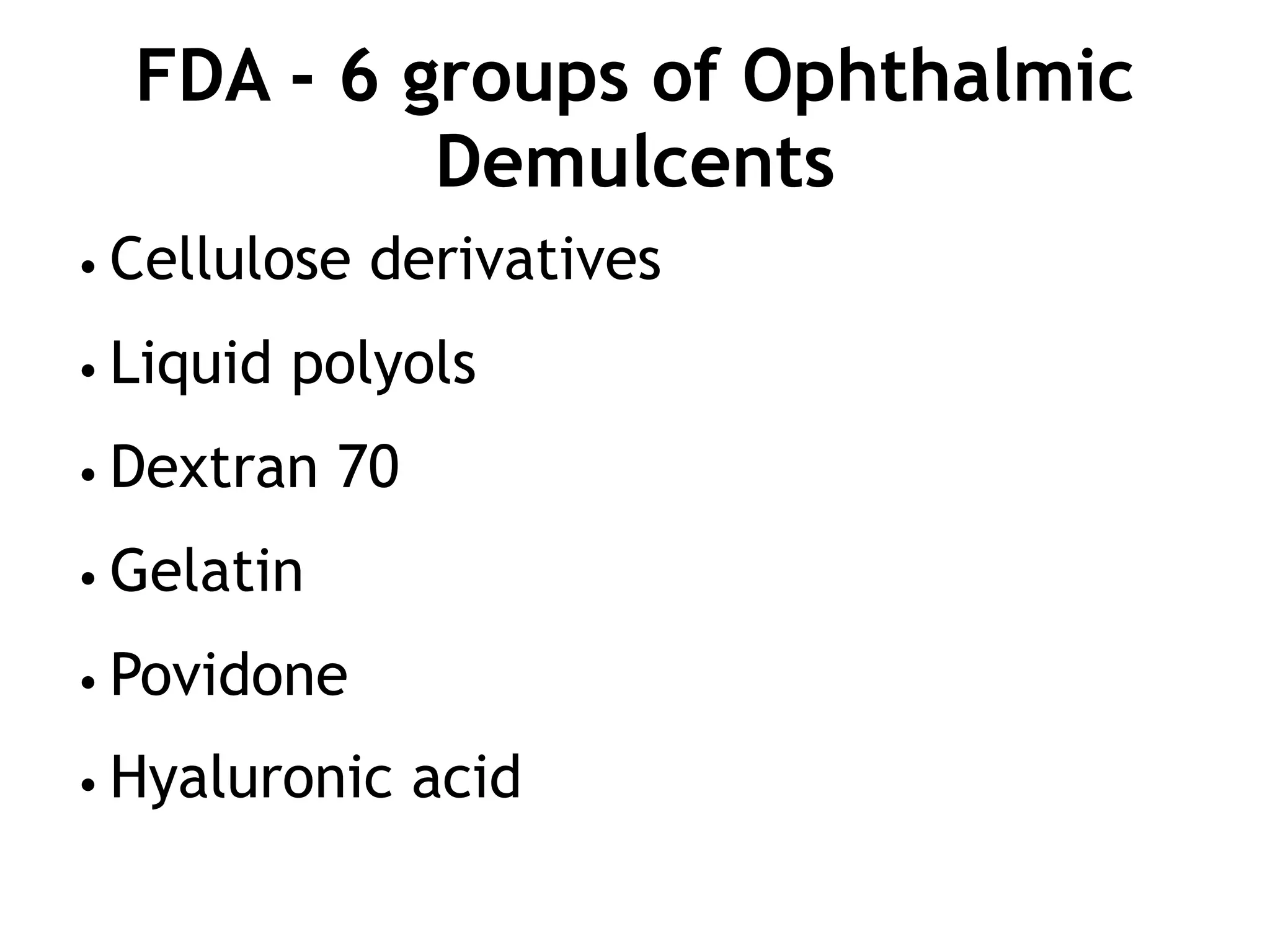
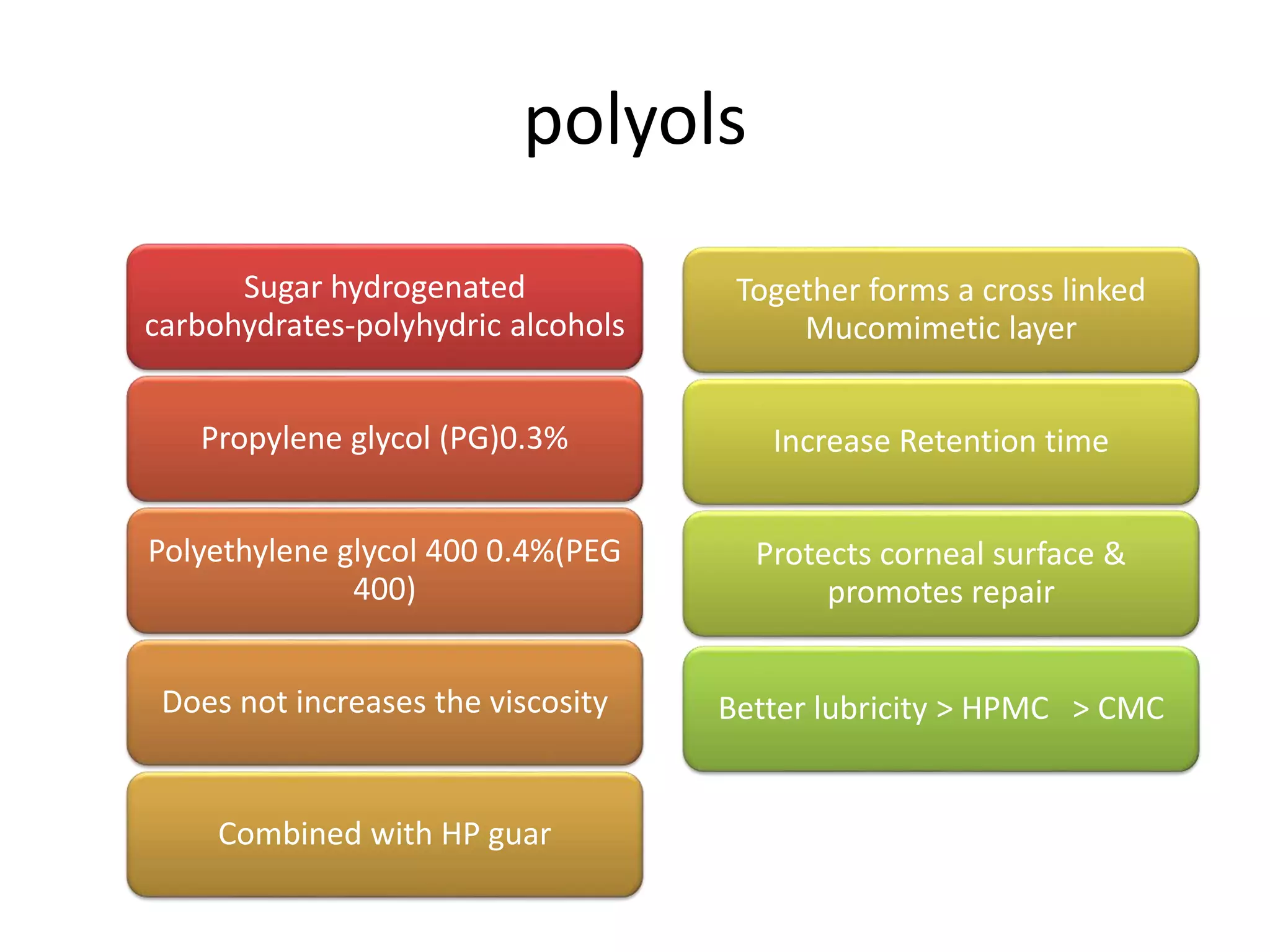
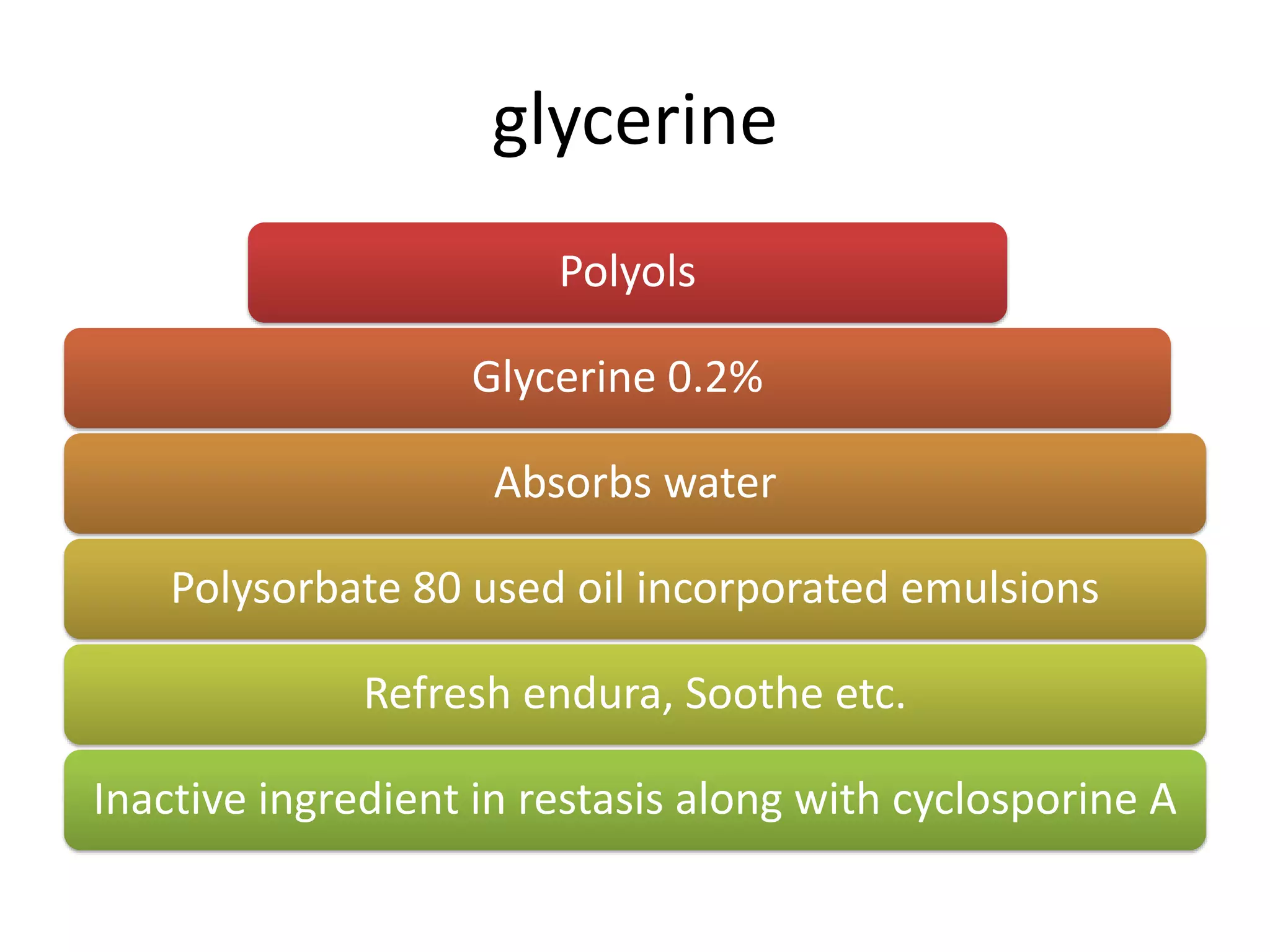
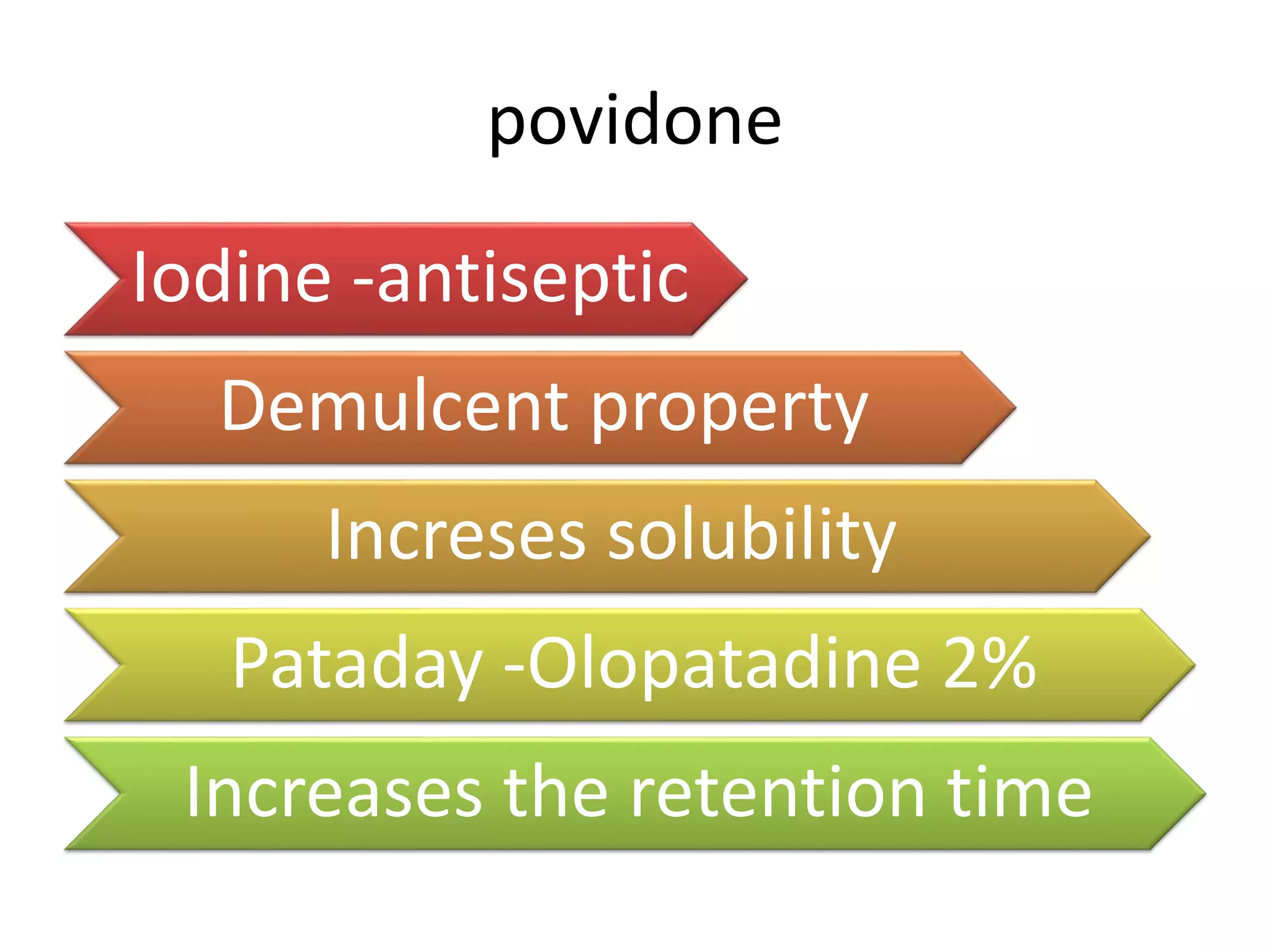
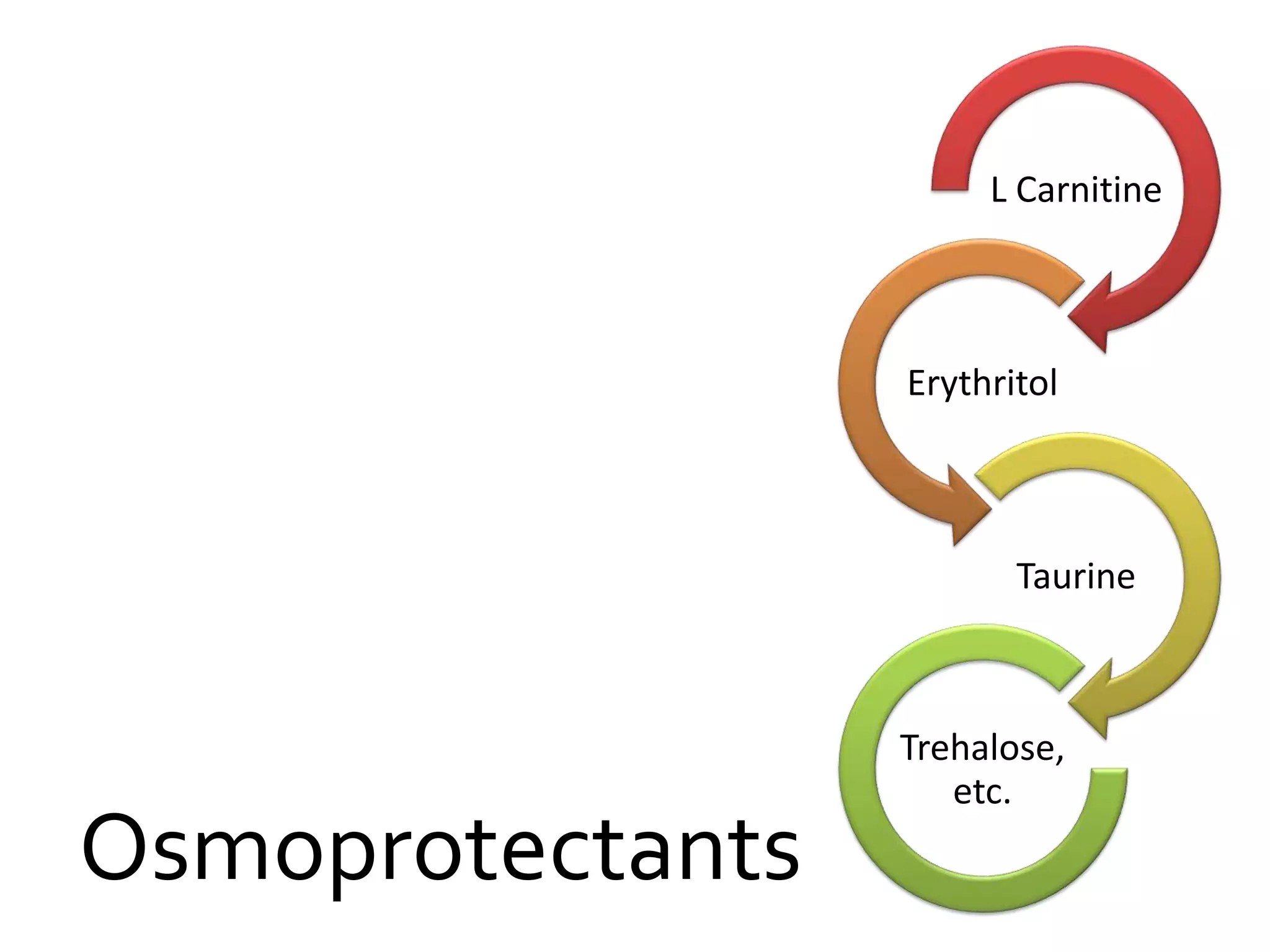
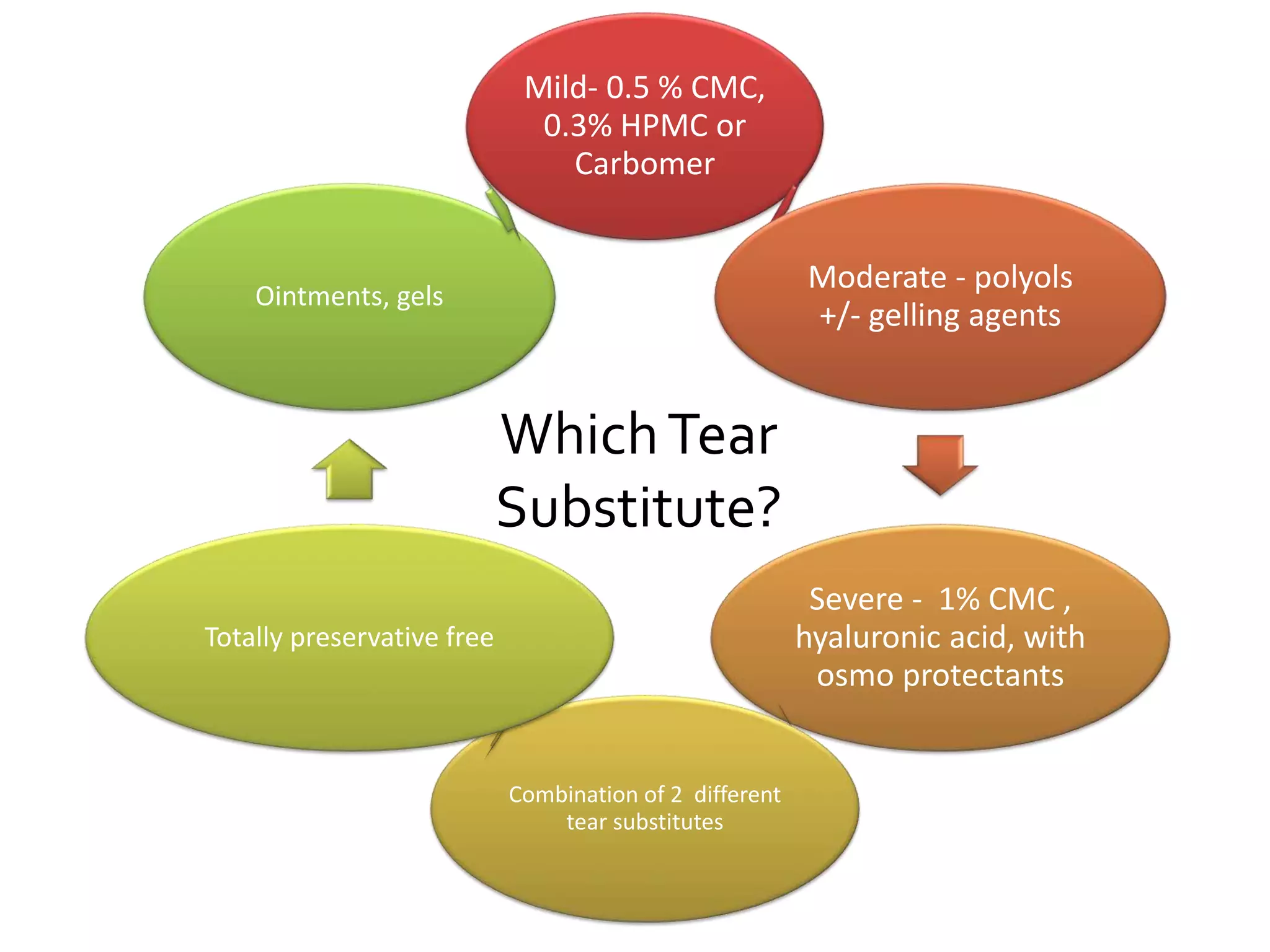
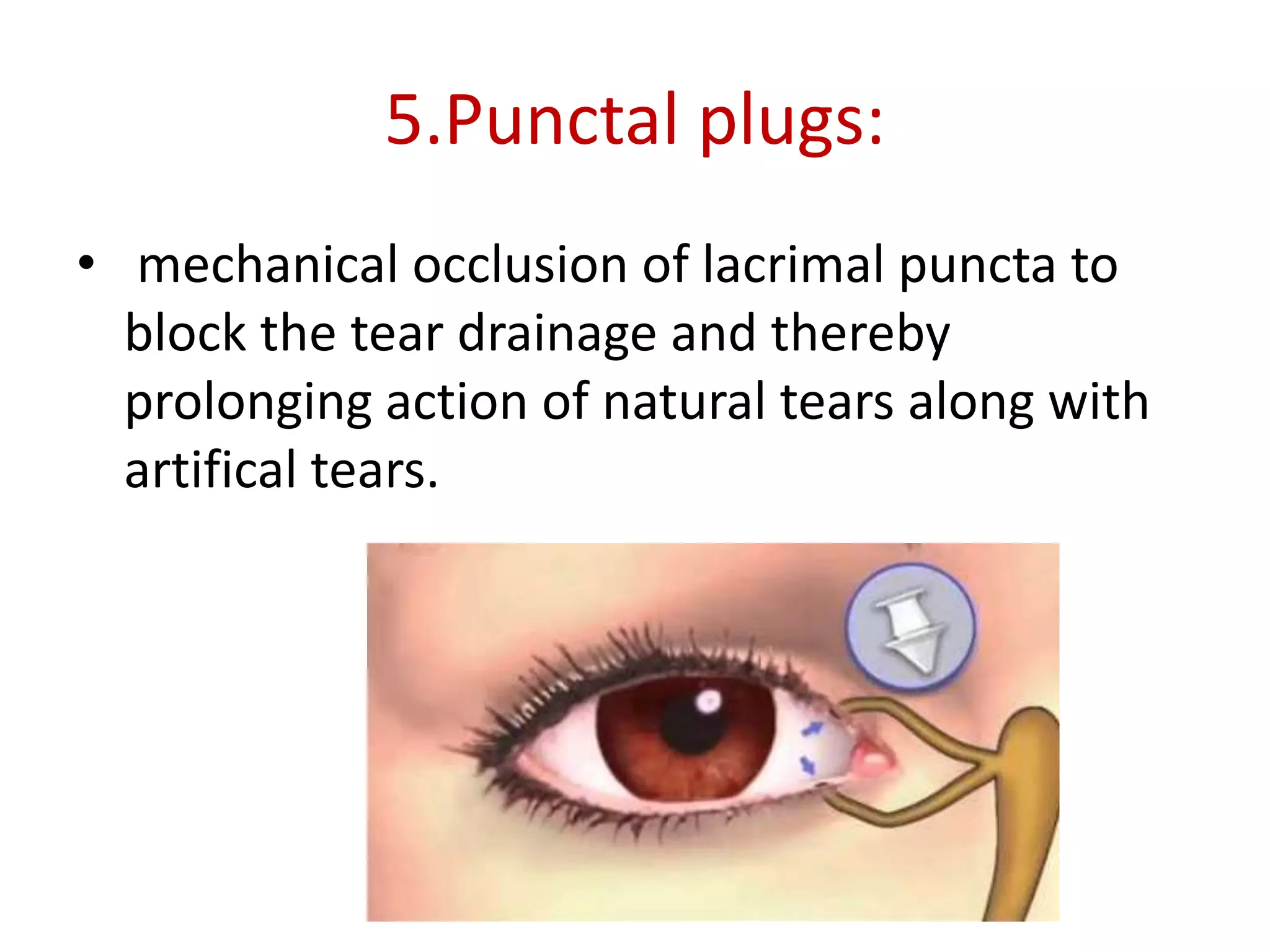
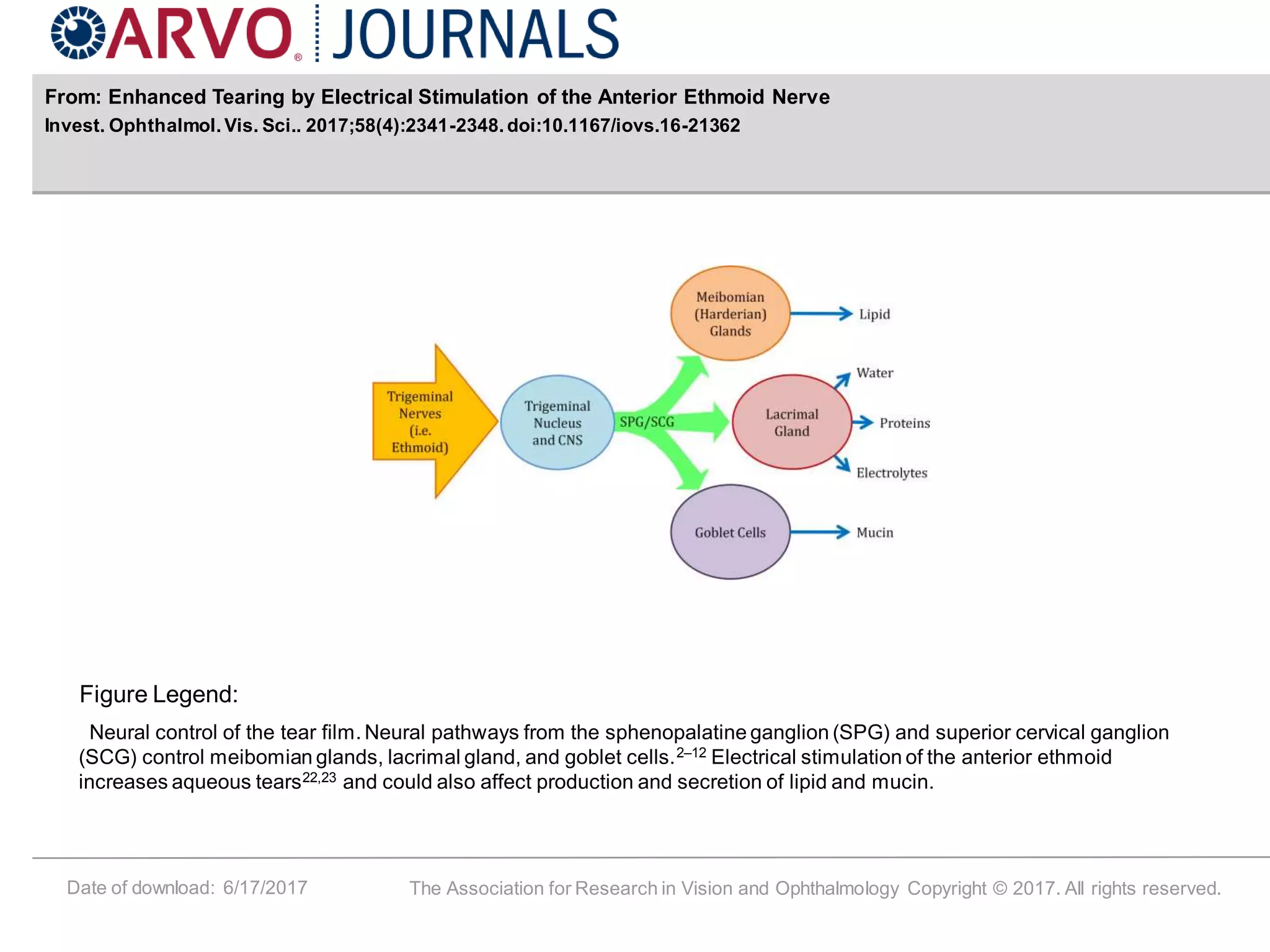
This document discusses various tear substitutes and artificial tears. It begins by covering the history of eye baths and artificial tears dating back to the 16th century. It then discusses different types of artificial tears including autologous serum, various polymers like cellulose derivatives, polyols, dextran 70, and hyaluronic acid. It also discusses newer technologies like punctal plugs, collagen implants, soft contact lenses, and electrical stimulation to increase tear production. The document concludes by discussing various preservatives used in artificial tears and newer disappearing preservatives.