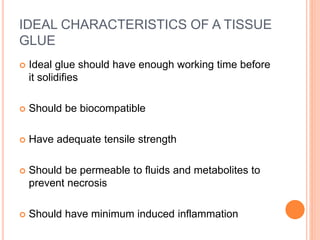
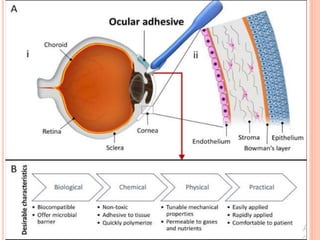
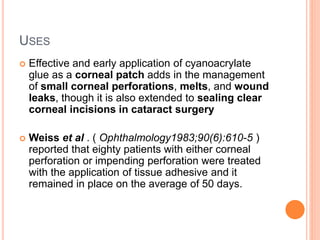
Tissue adhesives are being used increasingly in ophthalmic surgery as alternatives to sutures. The main types discussed are cyanoacrylate glues and fibrin glues. Cyanoacrylate glues polymerize on contact with moisture and have bacteriostatic properties. Fibrin glues are biological adhesives that mimic the coagulation cascade. Both have advantages over sutures like ease of use and patient comfort, but also limitations like potential toxicity and induced inflammation. The document discusses properties, applications, and techniques for applying various tissue adhesives.









































![IN GLAUCOMA
It is used as an effective method of achieving
conjunctival wound closure after all drainage procedure.
Its successful use has also been reported in the
management of post trabeculectomy hypotony due to
leaking bleb.
It is considered as a safe substitute for the sutures used
in glaucoma drainage device [GDD] surgery.
It does not alter intra ocular pressure control, reduces
post-operative conjunctival inflammation and surgical
time.
However, further studies are needed to better
understand the role of the glue in GDD implantation.](https://image.slidesharecdn.com/tissueadhesives-210126173223/85/Tissue-adhesives-63-320.jpg)