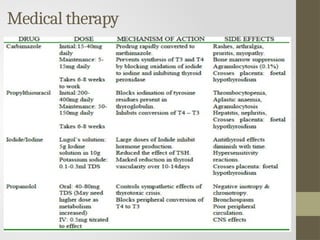
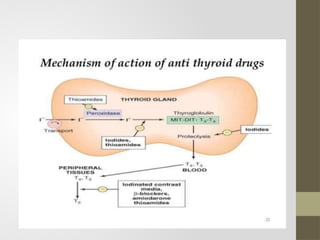
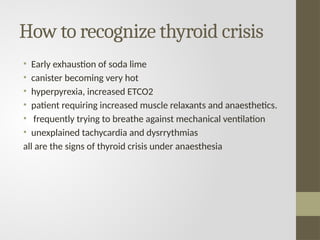
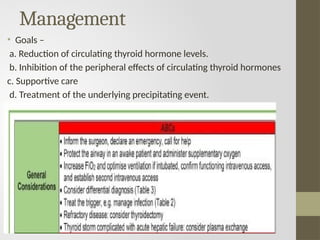
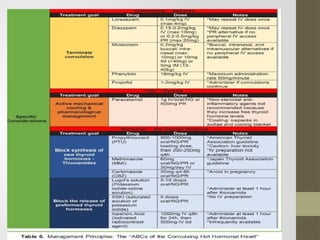
The document discusses the implications of thyroid disorders, particularly hyperthyroidism and hypothyroidism, on anesthesia management. It highlights the risks during anesthesia for thyroidectomy, the need for careful preoperative assessment, and the importance of monitoring cardiovascular and respiratory responses. Various treatment modalities and preoperative preparations for hyperthyroid patients are also detailed to mitigate potential complications during surgery.

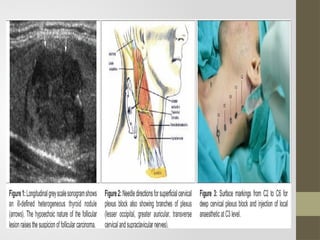
![Pre operative preparation of
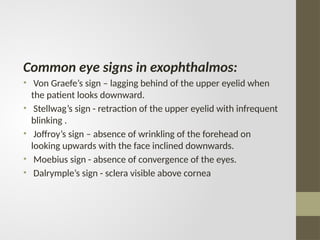
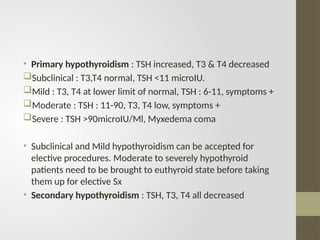
hyperthyroid patient
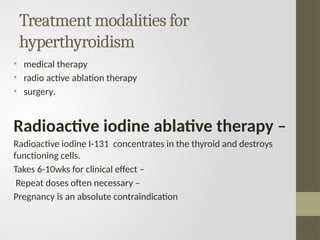
All patients are first treated with anti thyroid drugs for 6-8wks
till made euthyroid.
Beta blockers to be continued –
Lugol’s iodine – 5% iodine in 10% potassium iodide – 8mg
iodide/drop [ Dose – 3-5 drops thrice a day ]
Saturated solution of potassium iodide (SSKI) - 50mg iodide per
drop [Dose – one drop thrice a day].
Iodide decreases T3 & T4 synthesis by inhibiting iodide oxidation
and organification – Wolff –Chai koff effect or thyroid constipation.
Pre-op iodine administration upto 14 days helps in - Reducing the
size of the swelling - Decreases the vascularity - Makes the gland
more firm.
Iodine to be given for not more than 14 days before the surgery. If
given for more days , can produce a recurrence of hyperthyroidism
– Jod Basedow effect or thyroid escape.](https://image.slidesharecdn.com/thyroiddisordersandanaesthesia-240826093351-632c8bba/85/THYROID-DISORDERS-AND-ANAESTHESIA-ppt-1-pptx-21-320.jpg)
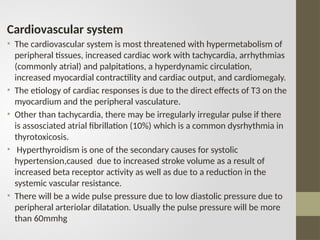
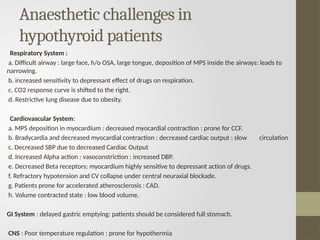
![Anaesthesia for hyperthyroid patient
• Glycopyrrolate as a part of premedication during thyroid surgery can be
immensely helpful .
• Pre-oxygenation with 100% oxygen enhances the functional residual volume
and thus can provide enough time for securing the access to difficult airway.
• Shorter acting opioids such as fentanyl, remi fentanyl, sufentanyl should
preferably be used but the limited availability of these drugs except fentanyl
is a major drawback.
• I.V. induction is the first choice. –
[If difficult intubation is anticipated then inhalational induction is preferred.]
• If patient gives history of obstructive symptoms and snoring, then awake
intubation is preferred.
• Thiopentone is the induction agent of choice because of thio group
producing anti thyroid effect.
• Propofol also can be used. The advantages are - decreased sympathetic
response to laryngoscopy and intubation, antiarrhythmic effect and
decreased incidence of post op nausea and vomiting.
• Ketamine is contraindicated as it increases the HR and BP.](https://image.slidesharecdn.com/thyroiddisordersandanaesthesia-240826093351-632c8bba/85/THYROID-DISORDERS-AND-ANAESTHESIA-ppt-1-pptx-24-320.jpg)
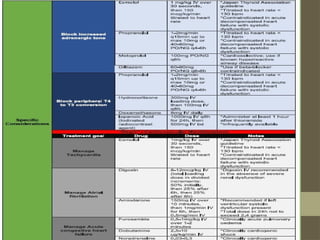
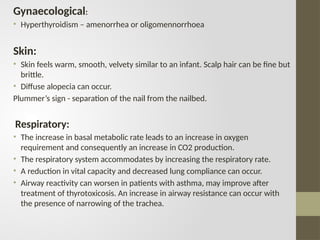
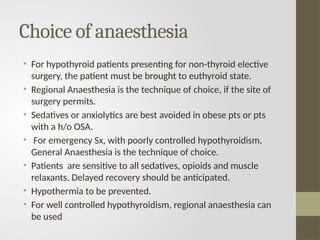
![Atrial fibrillation
• Atrial fibrillation is the most common cardiac complication of
hyperthyroidism. It occurs in up to 15% of hyperthyroid patients compared
with 4% in the general population, and is more common in men and in
patients with triiodothyronine (T3) toxicosis, and its incidence increases
with advancing age.
PATHOPHYSIOLOGY
1]Autoantibody formation against β1-adrenergic and M2-muscarinic
receptors has been known to occur in hyperthyroidism and may trigger Atrial
fibrillation prior to thyroid dysfunction.
2]A genetic susceptibility to atrial fibrillation may be linked to
hyperthyroidism.](https://image.slidesharecdn.com/thyroiddisordersandanaesthesia-240826093351-632c8bba/85/THYROID-DISORDERS-AND-ANAESTHESIA-ppt-1-pptx-39-320.jpg)
![REFERENCES
• Miller’s Anaesthesia, 9th edition
• Barash, Paul G, Clinical Anaesthesia, 6th edition
• Stoelting RK, Dierdorf SF., Anaesthesia and Co-
Existing Disease, 3rd edition
• Harrison’s Textbook of Internal Medicine, 18th
edition
• Elshimy G, Chippa V, Correa R. Myxedema. [Updated
2023 Aug 14].
• Bajwa SJ, Sehgal V. Anesthesia and thyroid surgery:
The never ending challenges. Indian J Endocrinol
Metab. 2013 Mar;17(2):228-34. doi: 10.4103/2230-
8210.109671. PMID: 23776893](https://image.slidesharecdn.com/thyroiddisordersandanaesthesia-240826093351-632c8bba/85/THYROID-DISORDERS-AND-ANAESTHESIA-ppt-1-pptx-70-320.jpg)
