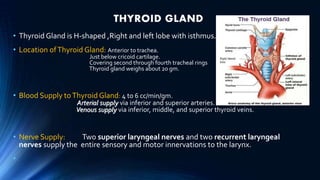
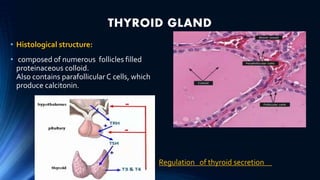
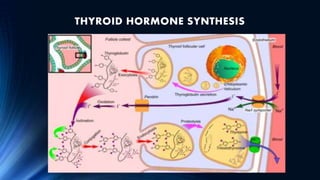
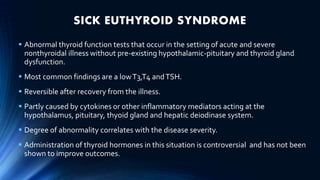
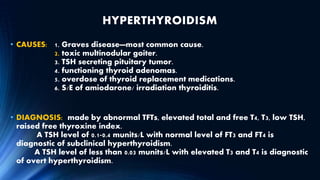
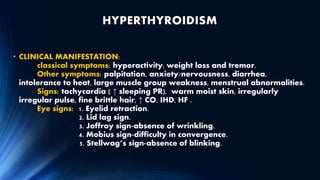
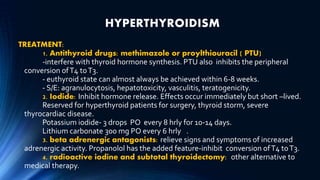
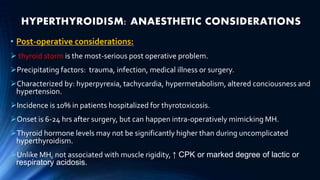
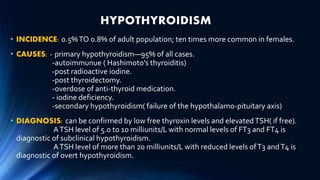
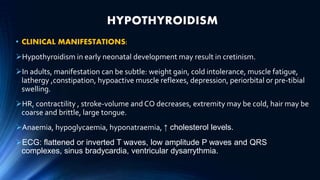
The document discusses thyroid disorders including hyperthyroidism, hypothyroidism, and thyroid storm and their implications for anesthesia such as increased sensitivity to drugs, risks of tachycardia and arrhythmias, and need for careful monitoring of cardiac and respiratory function. It provides guidance on preoperative preparation, intraoperative management, and postoperative care for patients with thyroid disorders undergoing surgery.












![Thyroid ppt [autosaved]](https://image.slidesharecdn.com/thyroidpptautosaved-170310134424/85/Thyroid-ppt-autosaved-24-320.jpg)