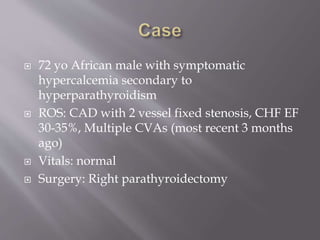
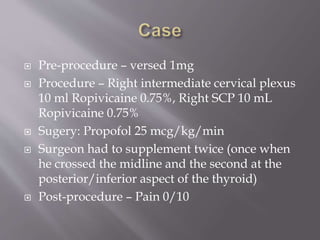
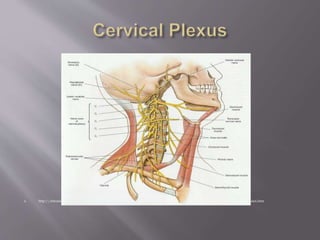
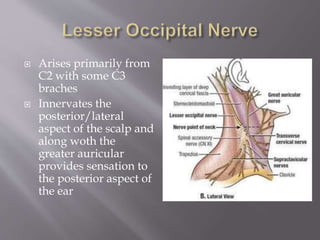
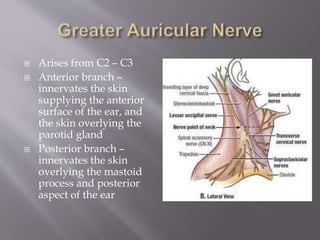
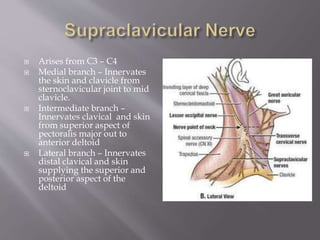
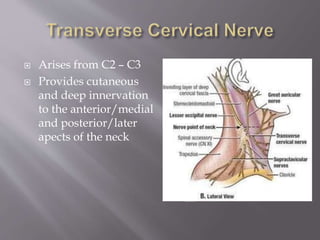
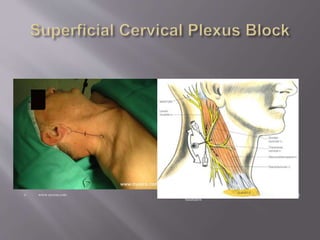
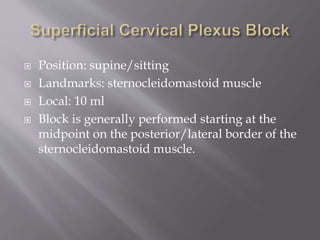
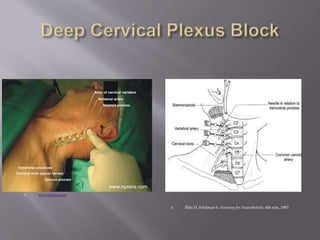
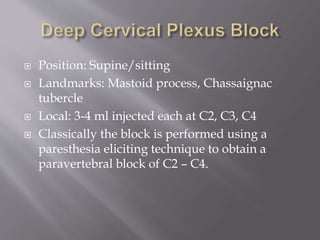
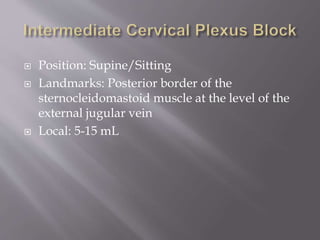
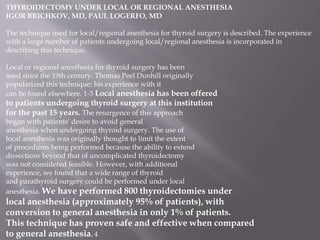
This document summarizes a technique for performing local/regional anesthesia for thyroid surgery. It begins by describing the patient who will undergo a parathyroidectomy due to hypercalcemia from hyperparathyroidism. It then provides background on the history and development of performing thyroid surgery under local/regional anesthesia. It proceeds to describe the relevant anatomy of the cervical plexus and its branches. It concludes by outlining the technique for performing a superficial cervical plexus block, including patient position, landmarks, local anesthetic used, and injection points along the posterior border of the sternocleidomastoid muscle at the level of the external jugular vein. The summary is provided in 3 sentences or less as requested.



![Thyroid. 2012 Jan;22(1):44-52. doi: 10.1089/thy.2011.0260. Epub 2011 Dec 5.
Bilateral superficial cervical plexus block in combination with general anesthesia has a low efficacy in thyroid
surgery: a meta-analysis of randomized controlled trials.
Warschkow R, Tarantino I, Jensen K, Beutner U, Clerici T, Schmied BM, Steffen T.
Source
Department of Surgery, Kantonsspital St. Gallen, St. Gallen, Switzerland.
Abstract
BACKGROUND:
A combination of bilateral superficial cervical plexus block (BSCPB) and general anesthesia is recommended for
thyroid surgery. Proof of the efficacy of this combination remains weak. Furthermore, data on the safety of this
regimen are lacking. Therefore, a meta-analysis of randomized controlled trials (RCT) to evaluate the efficacy and
safety of BSCPB as an adjunct to general anesthesia in patients receiving thyroid surgery was performed.
METHODS:
A meta-analysis of RCT was performed that included interventional groups evaluating the efficacy of BSCPB 6
and 24 hours after thyroid surgery.
RESULTS:
Eight RCT, including a total of 799 patients (463 who underwent BSCPB and 336 controls), were analyzed. A
meta-analysis demonstrated a reduction in pain scores 6 hours (Hedges' g: -0.46 [95% CI: -0.74 to -0.19]; p=0.001)
and 24 hours postoperatively (Hedges' g: -0.49 [95% CI: -0.71 to -0.27]; p<0.001) in patients who had undergone
BSCPB. The relative risk for postoperative nausea and vomiting (PONV) was 0.80 (95% CI: 0.58 to 1.09, p=0.159)
in patients receiving BSCPB. Procedure-related adverse events were reported in three of the 476 patients who had
undergone BSCPB (0.6%; 95% CI: 0.1% to 2.0%). These three patients had transient paresis of the brachial plexus,
combined with a diaphragmatic paresis in one case, and all spontaneously resolved.
CONCLUSION:
The combination of BSCPB and general anesthesia has a significant benefit in reducing pain 6 and 24 hours after
thyroid surgery. However, the effect on pain reduction is too small to be of clinical relevance. Although it is a safe
procedure, the existing evidence allows for no recommendation concerning the application of BSCPB in thyroid
surgery. Further trials should evaluate a dose-response relationship and the incidence of PONV with this
regimen.](https://image.slidesharecdn.com/25820-cervicalplexusblock1-220830095750-f423d6c1/85/25820-Cervical-Plexus-Block-1-pptx-34-320.jpg)