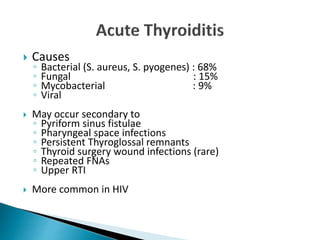
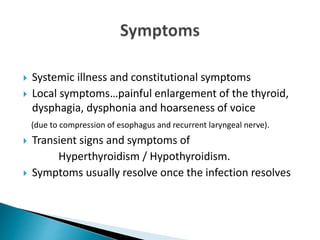
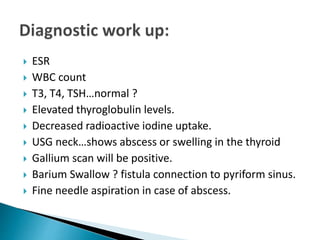
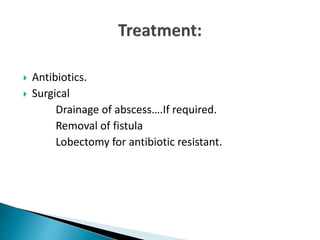
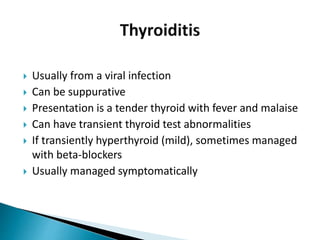
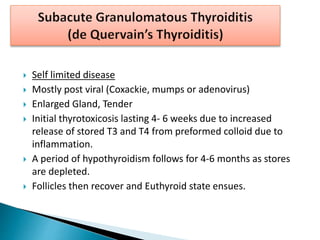
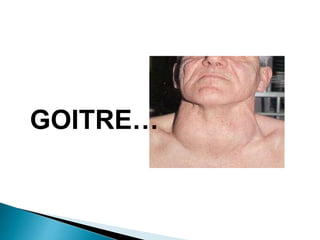
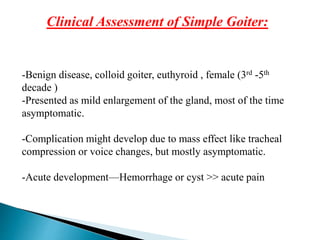
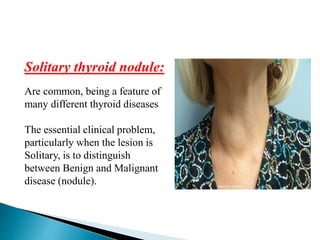
A 28-year-old female presents with a one-week history of low-grade fever, throat pain, and muscle aches. On examination, she has swelling on both sides of her neck that is tender to touch and worsens with swallowing or coughing. Tests show an enlarged, inflamed thyroid. The diagnosis is acute thyroiditis, which is usually self-limiting inflammation of the thyroid that can cause temporary thyroid dysfunction but resolves with treatment of the underlying infection or inflammation.