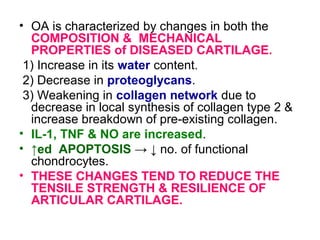
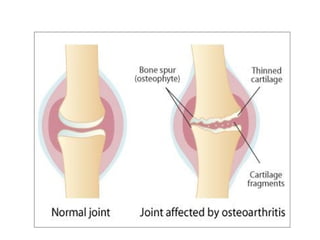
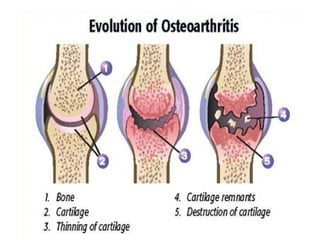
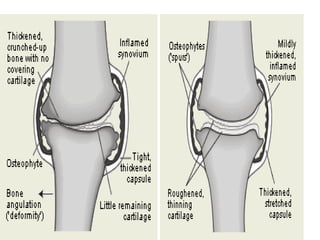
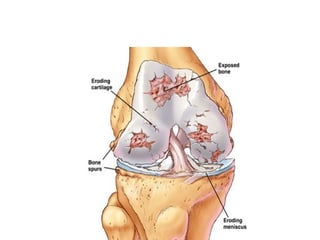
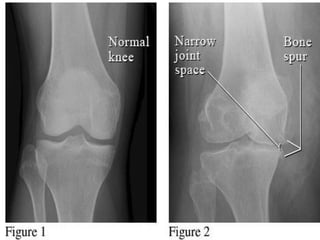
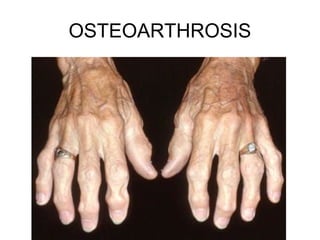
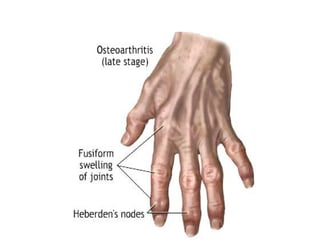
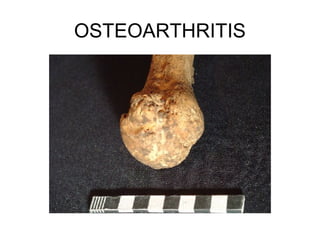
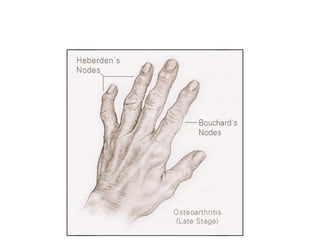
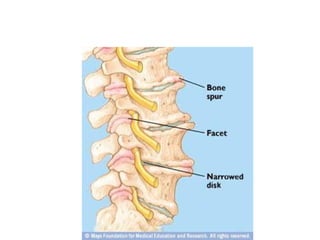
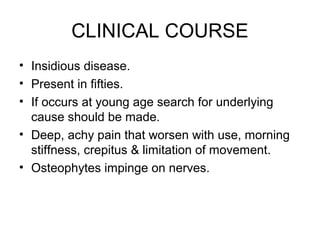
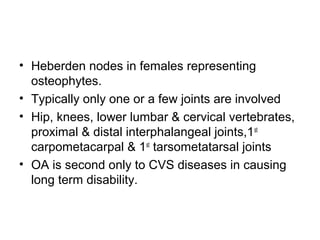
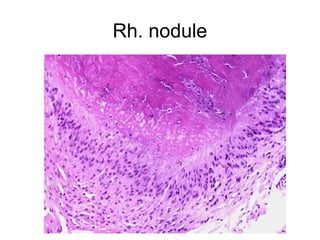
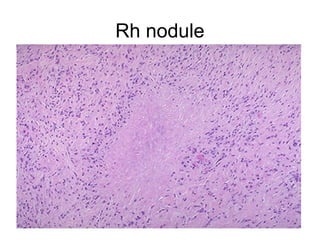
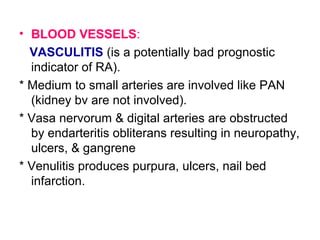
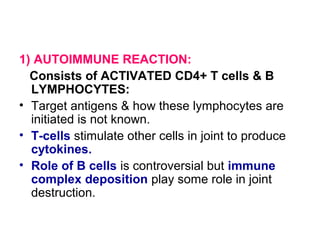
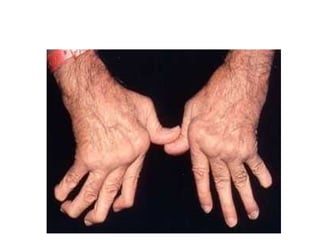
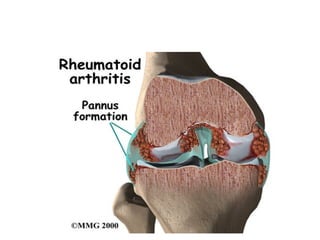
This document summarizes diseases of joints, including normal joint structure and function. It describes osteoarthritis and rheumatoid arthritis in detail. Osteoarthritis is characterized by erosion of articular cartilage in weight-bearing joints. Risk factors include age, mechanical stress, genetics, and bone density. Rheumatoid arthritis is a systemic inflammatory disease that principally attacks synovial joints, causing synovial inflammation and destruction of cartilage and bone. It is mediated by autoimmune reactions involving T cells, B cells, and cytokines like TNF and IL-1.