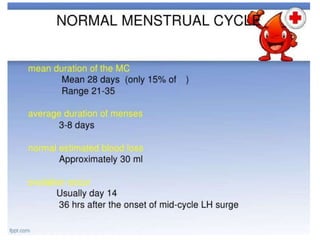
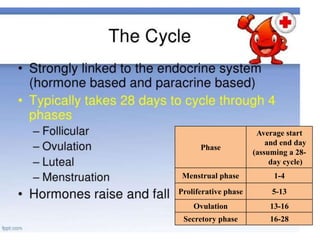
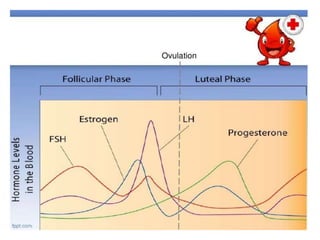
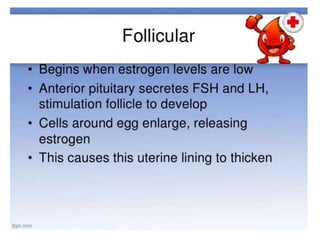
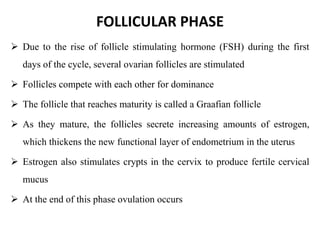
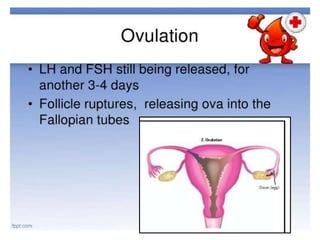
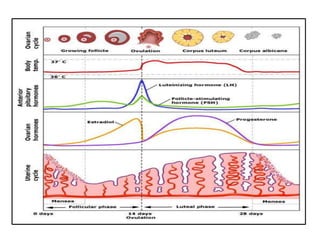
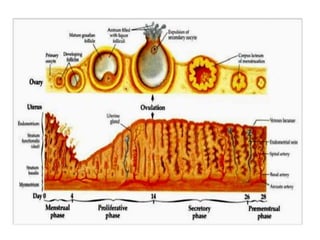
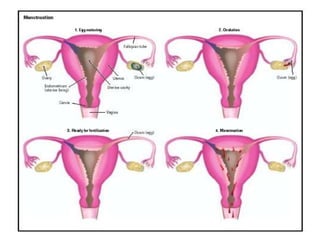
The menstrual cycle is the process in which females ripen and release one mature egg each month under control of the endocrine system. The average cycle is 28 days long and includes the menstrual, proliferative, ovulatory, and secretory phases. During ovulation, a mature egg is released from the ovaries. If the egg is not fertilized, menstrual bleeding occurs and the cycle repeats. The cycle allows for reproduction and continues monthly from menarche to menopause unless interrupted by pregnancy.