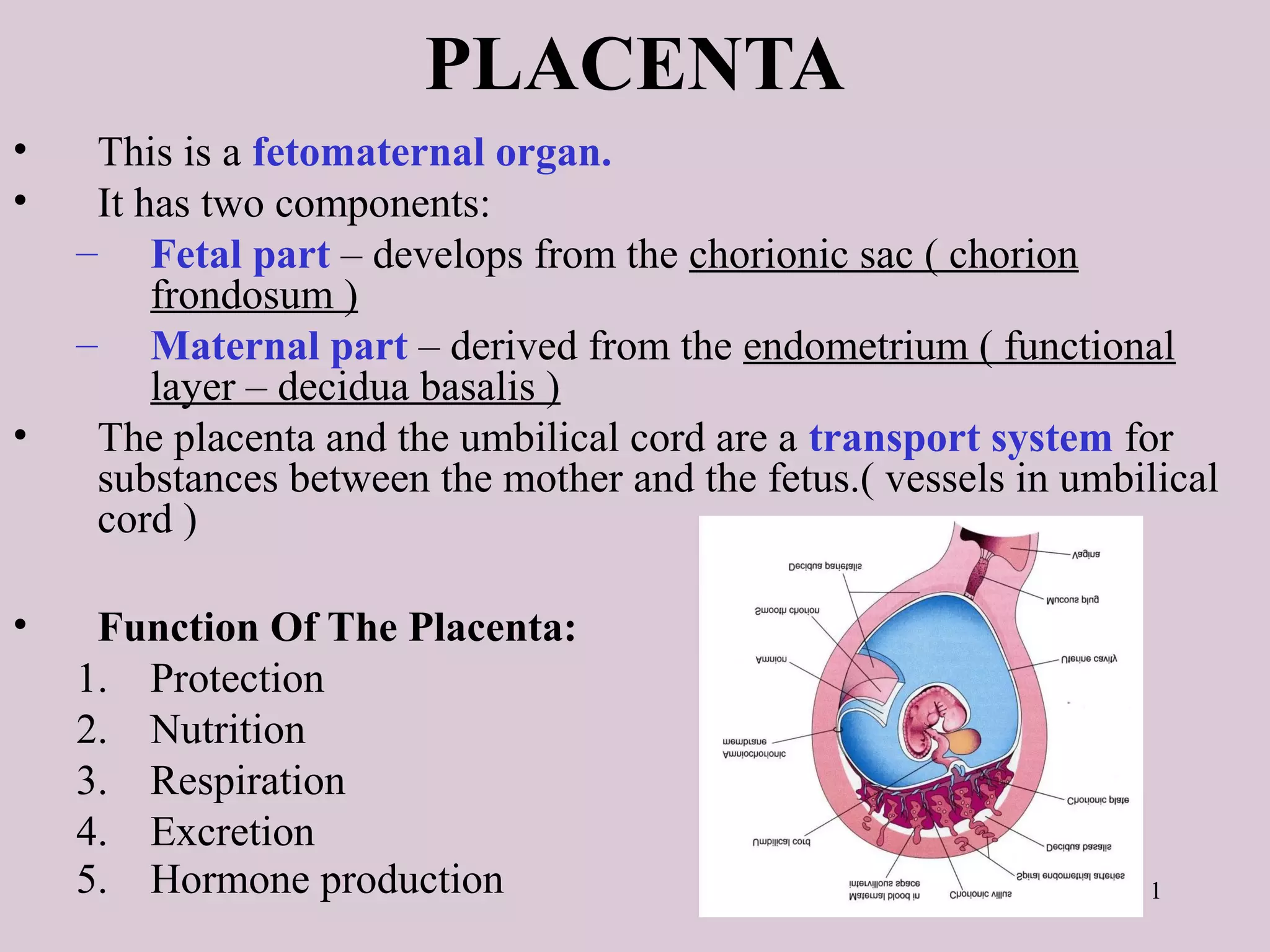
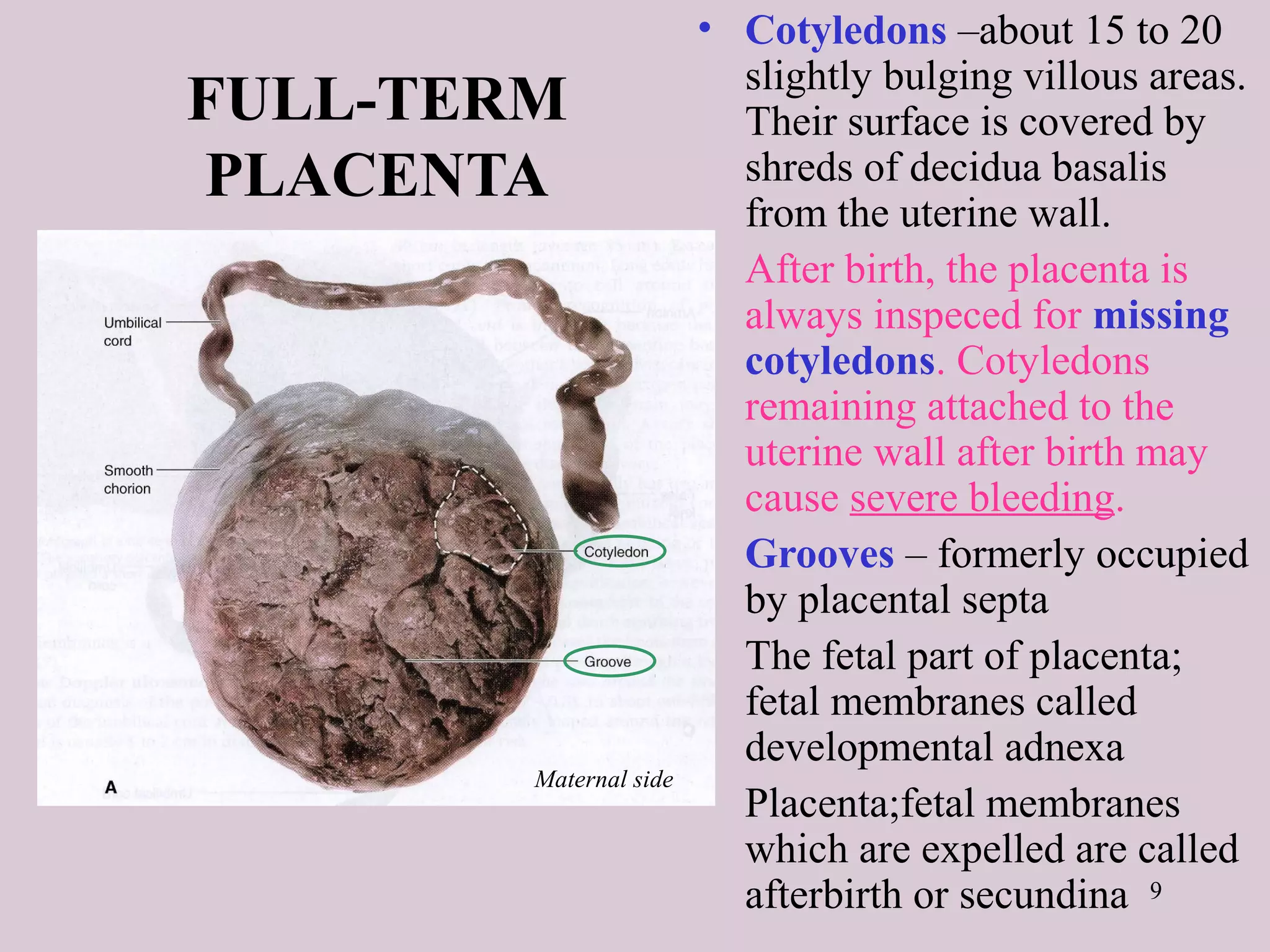
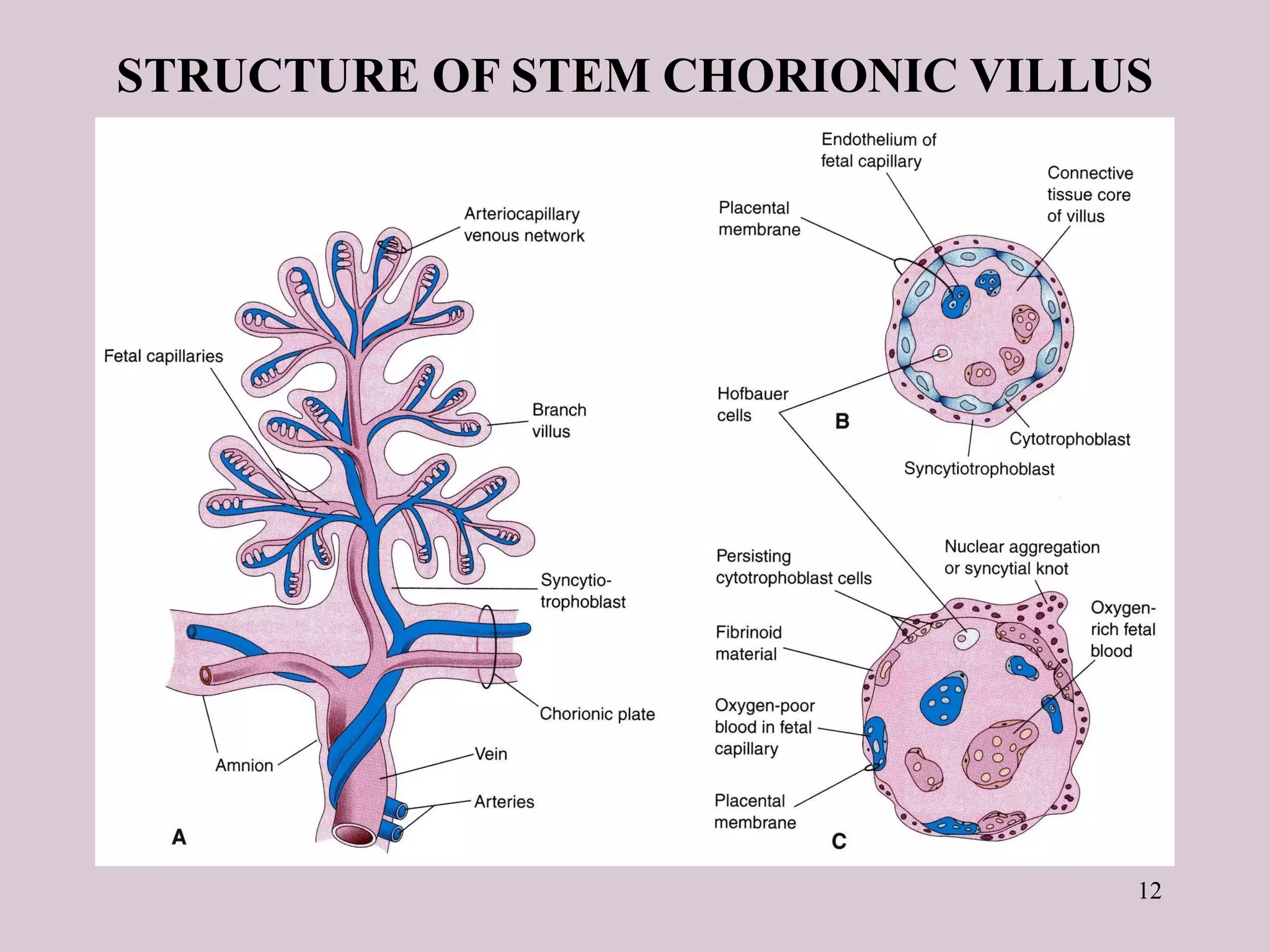
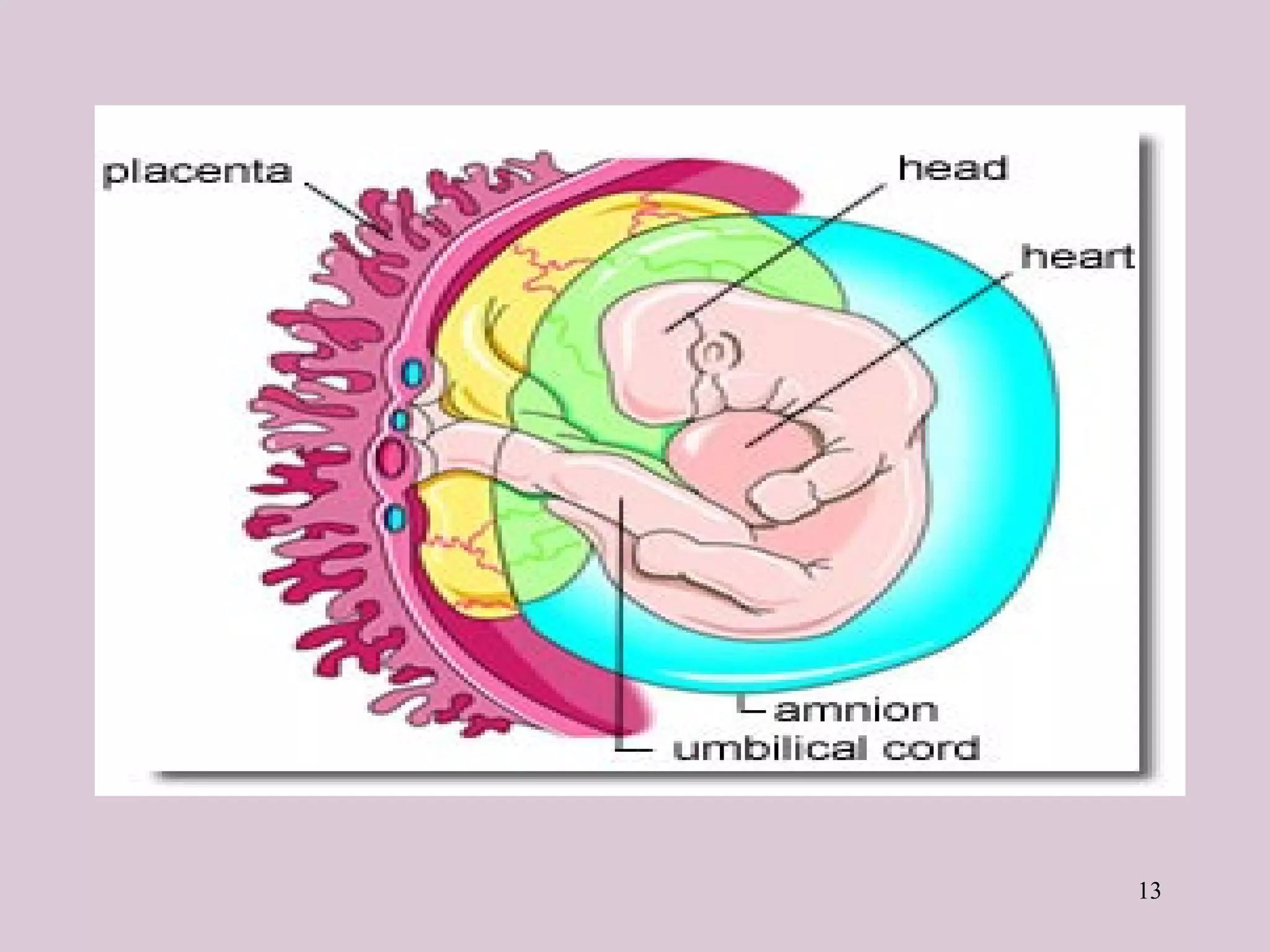
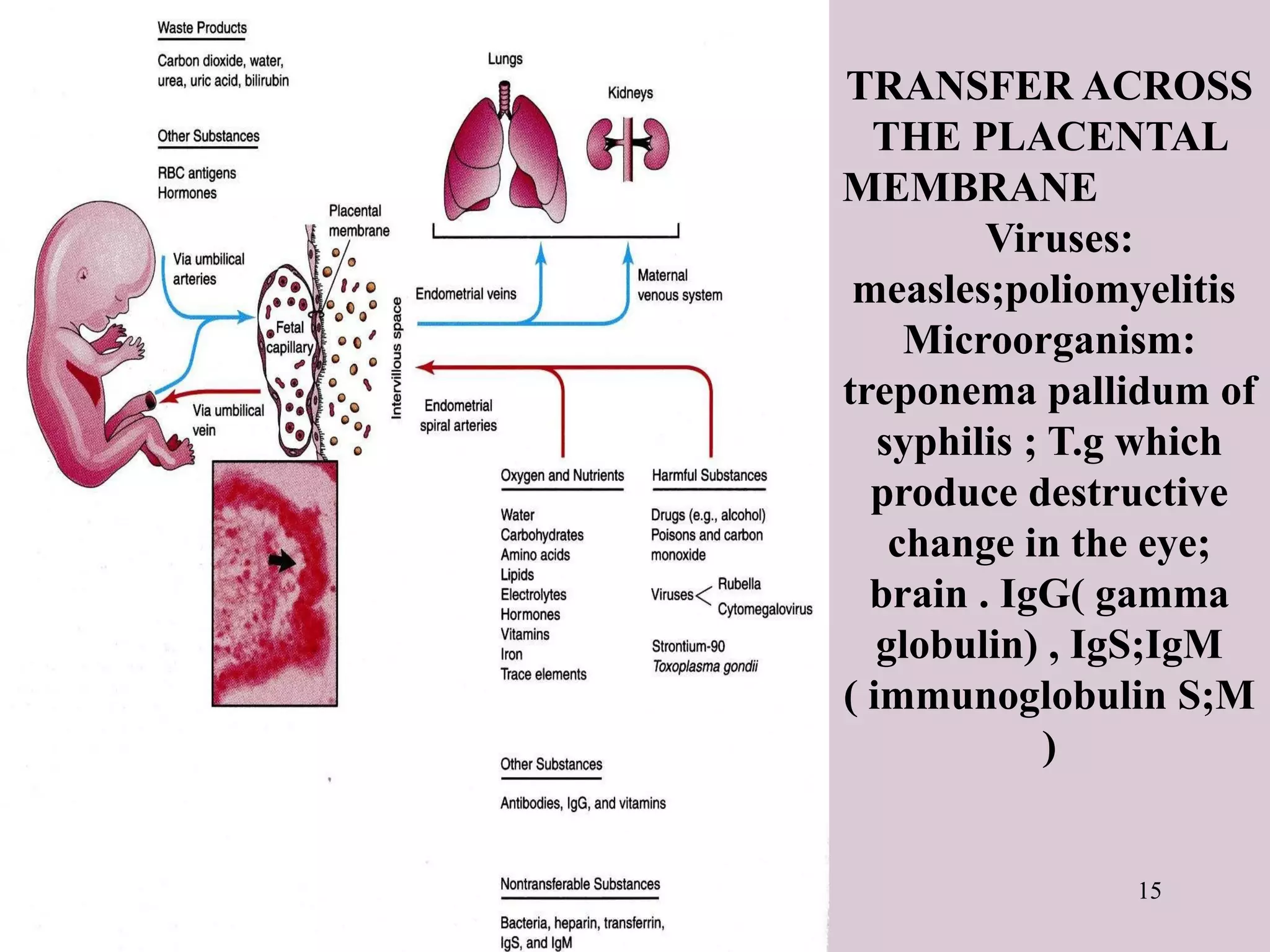
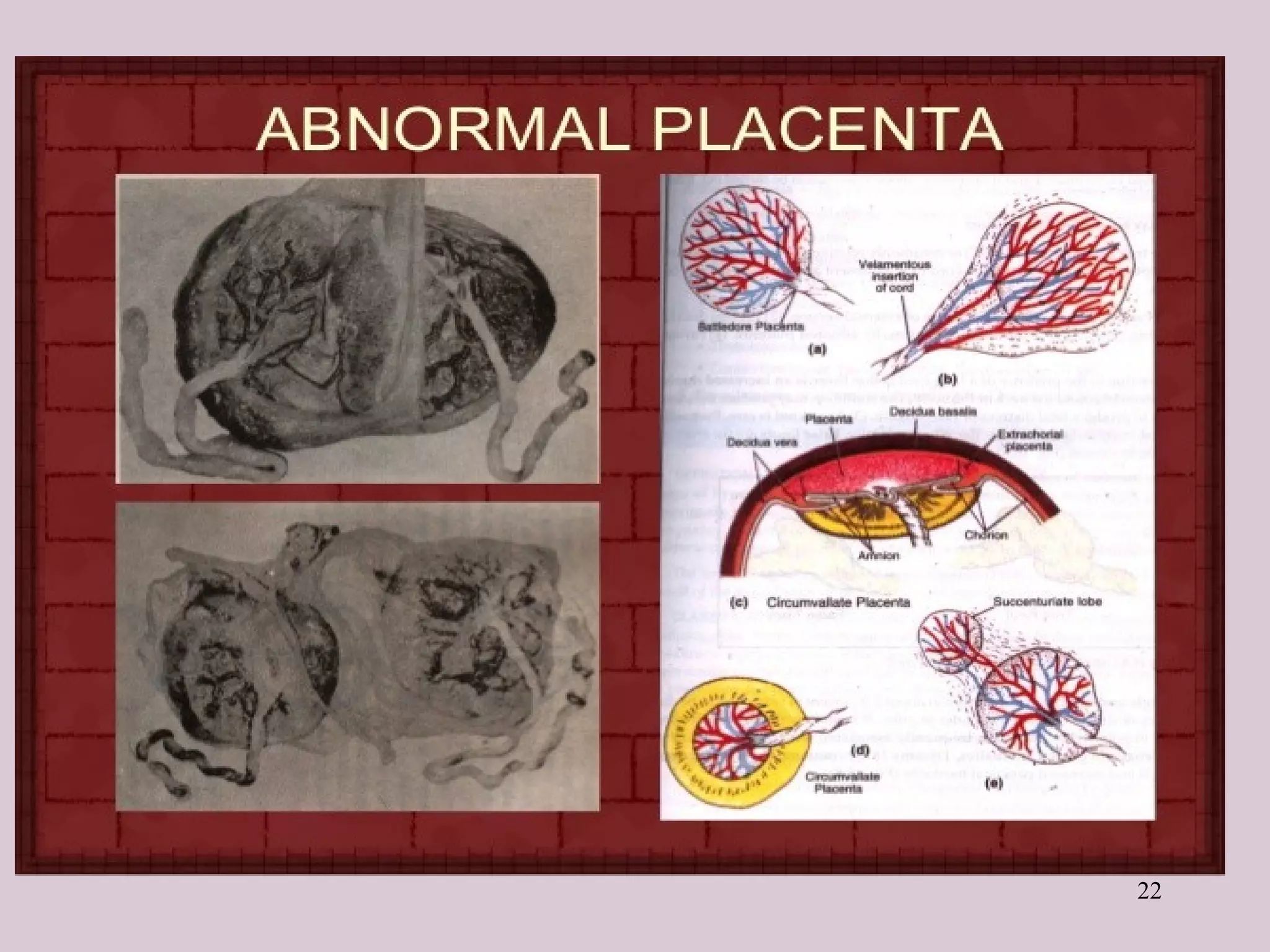
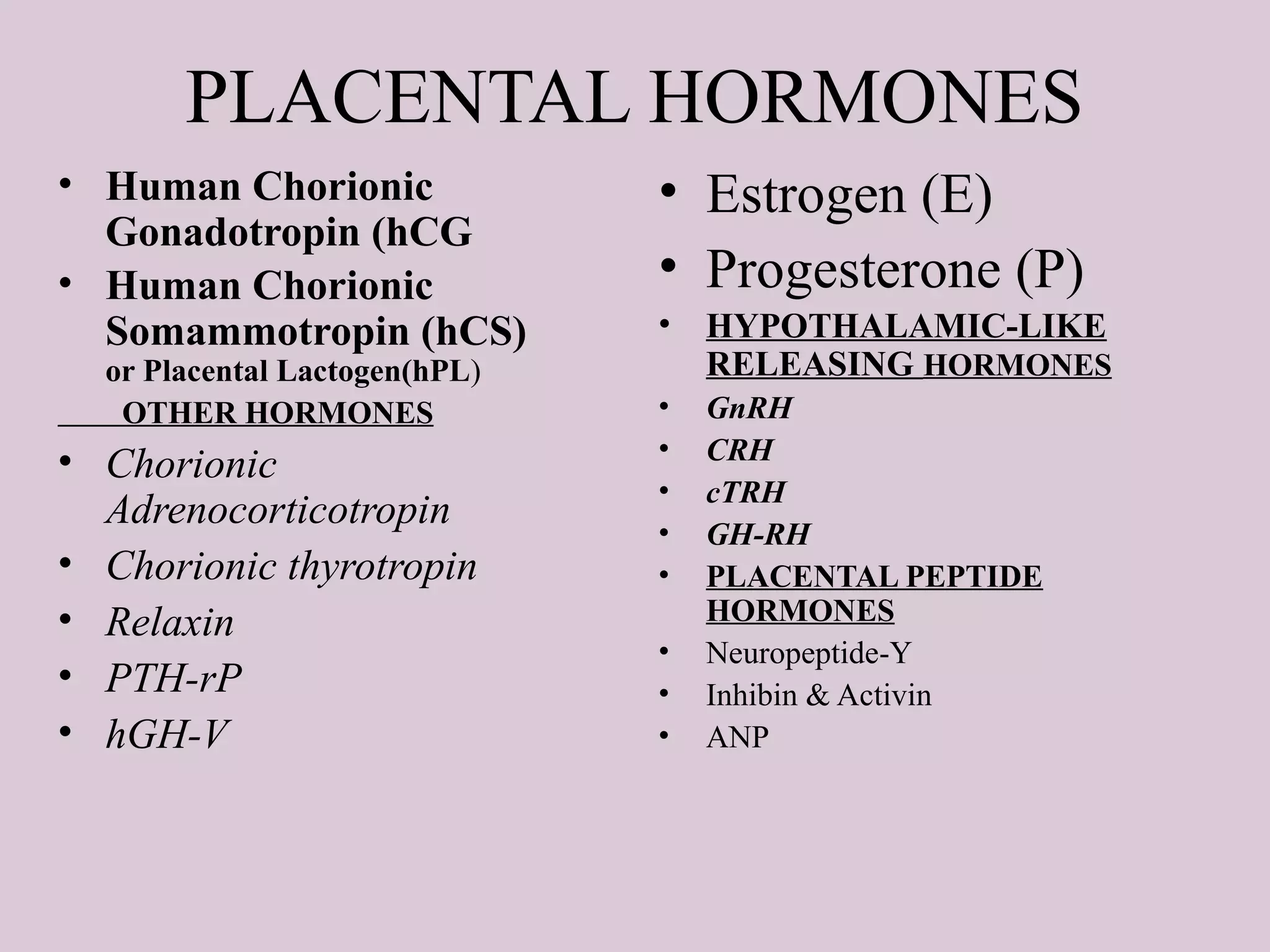
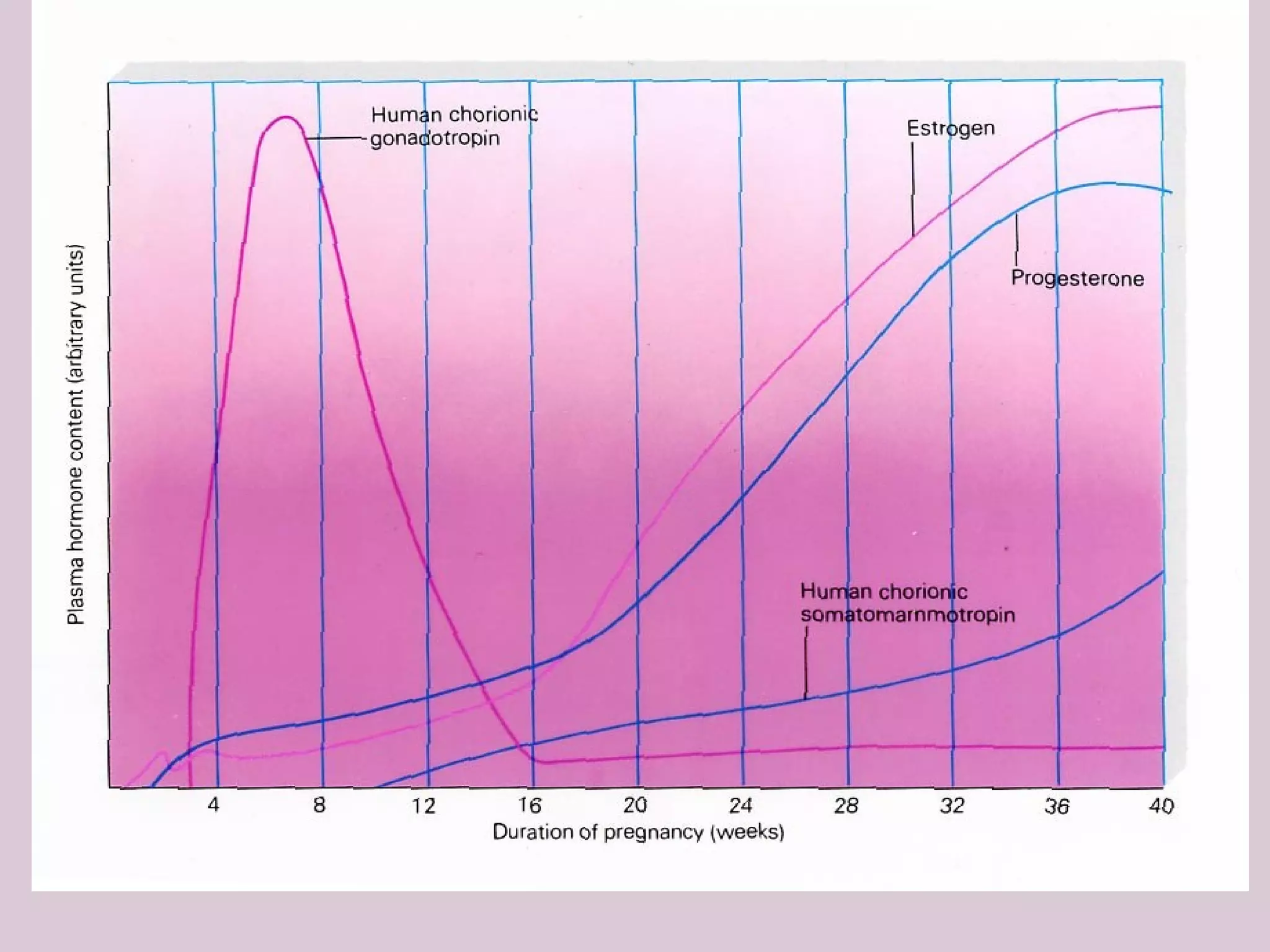
The document provides a detailed overview of the placenta, a fetomaternal organ with essential functions such as protection, nutrition, respiration, excretion, and hormone production. It describes the structural development of the placenta, the transition from the chorionic sac to the functional placenta, and the hormonal roles played by the placenta, including the production of human chorionic gonadotropin and other hormones throughout pregnancy. Additionally, it outlines the immunological and endocrine functions, emphasizing the intricate relationship between maternal and fetal tissues during gestation.