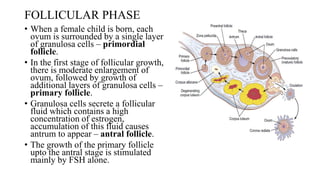
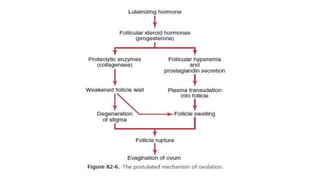
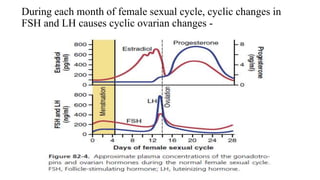
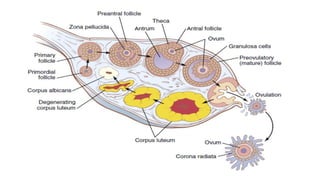
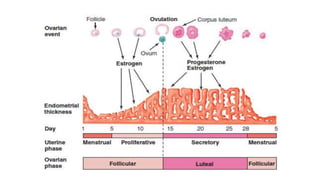
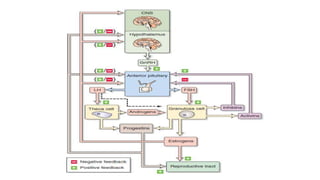
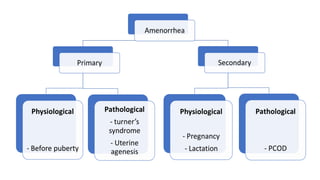
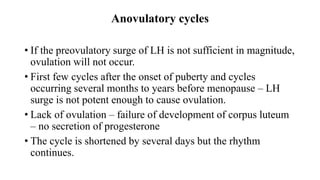
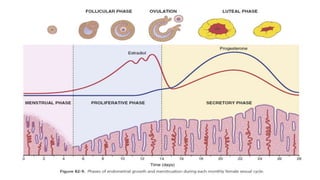
The document summarizes the female menstrual cycle, which occurs approximately every 28 days. It describes the ovarian and uterine cycles, including the follicular phase where an egg matures and is released (ovulation), the luteal phase where the corpus luteum forms, and the proliferative and secretory phases in the uterus. Key hormones like FSH, LH, estrogen, and progesterone regulate the cycle through feedback mechanisms between the hypothalamus, pituitary gland, and ovaries. Abnormalities in the cycle can occur if ovulation does not take place.