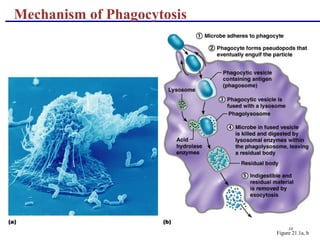
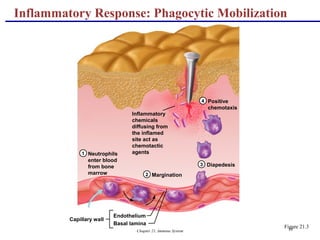
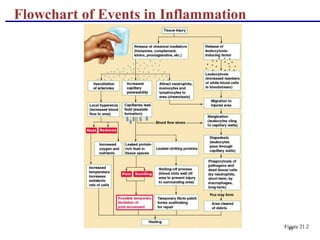
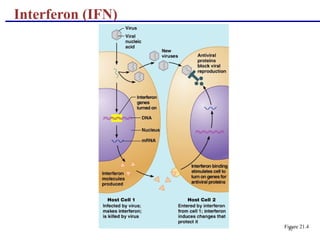
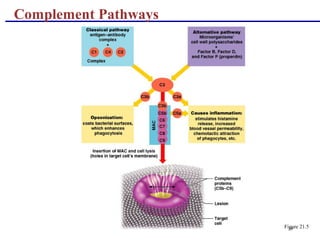
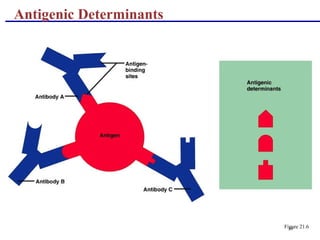
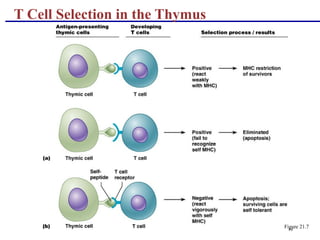
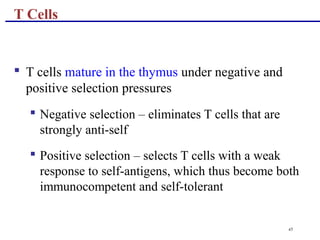
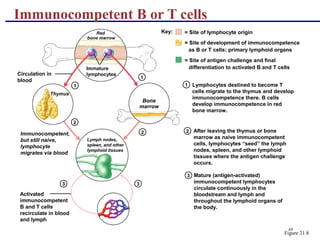
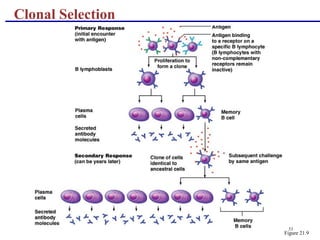
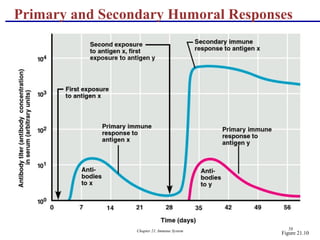
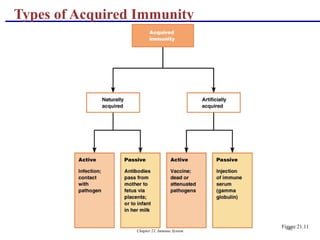
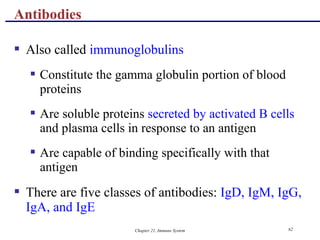
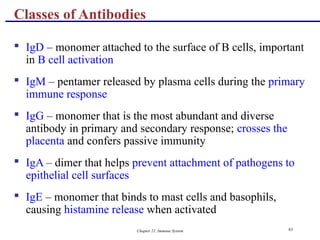
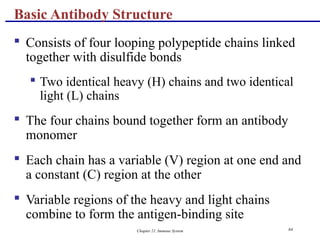
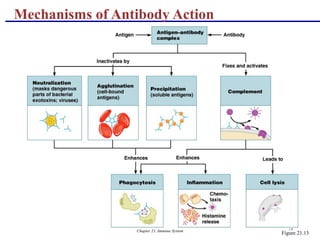
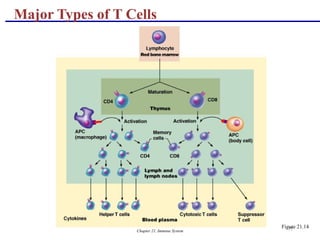
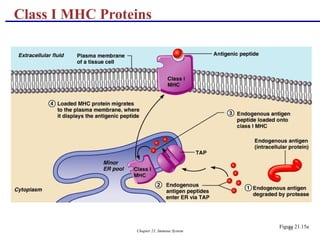
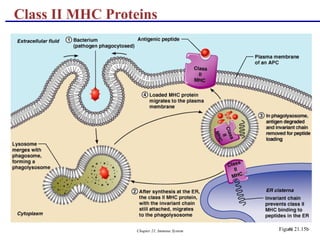
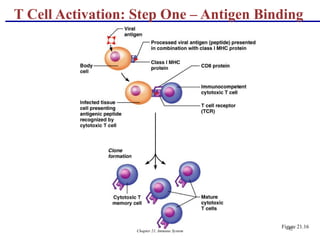
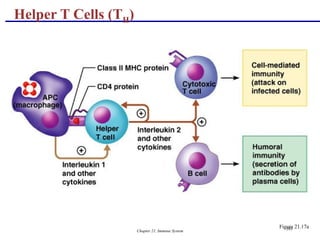
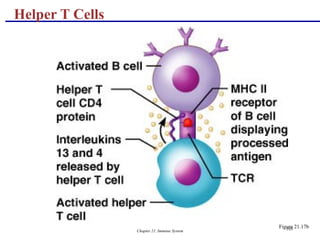
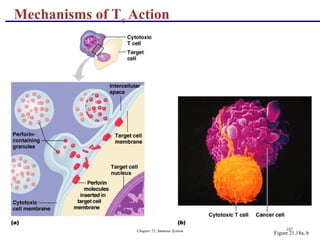
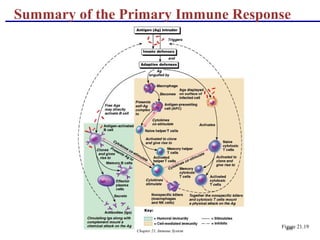
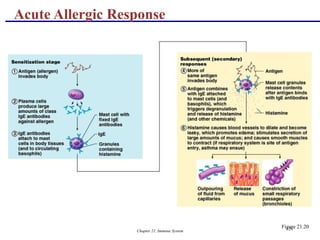
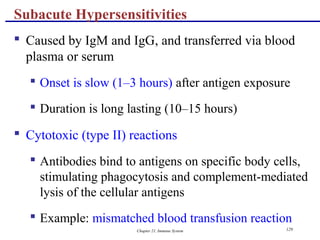
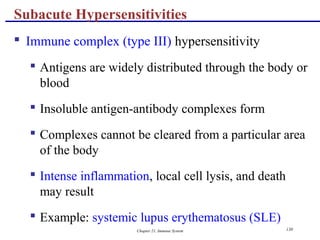
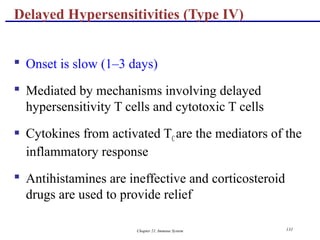
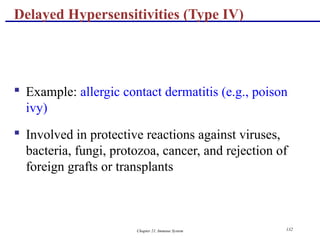
The document outlines the immune system's two defense mechanisms: innate (nonspecific) and adaptive (specific) immunity. Innate immunity includes physical barriers like skin and chemical responses such as phagocytosis and inflammation, while the adaptive immune response targets specific antigens and develops memory against them. It details the roles of various immune cells, cytokines, and the processes involved in inflammation and immune response activation.