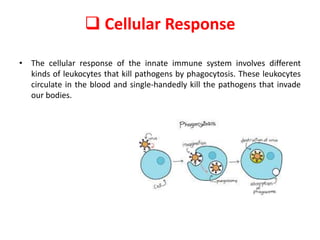
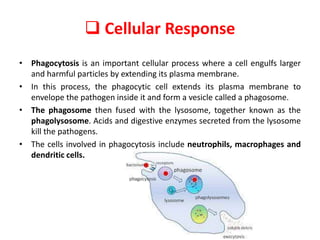
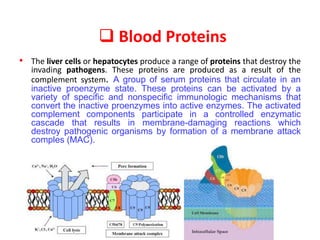
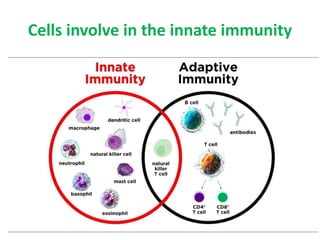
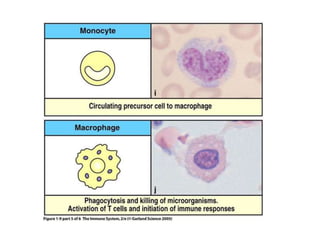
The document discusses the components of the innate immune system. It describes the physical, chemical, biological, and physiological barriers that block pathogens from entering the body. It also explains the cellular responses involving phagocytes that destroy pathogens through phagocytosis. The complement system and inflammatory response are blood proteins and processes that help eliminate pathogens. Key cells of innate immunity discussed are neutrophils, macrophages, dendritic cells, and natural killer cells.