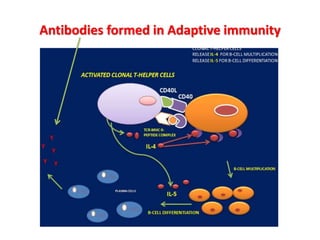
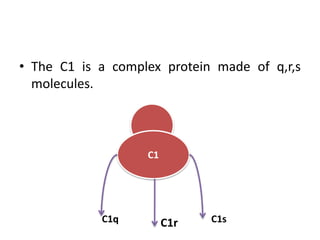
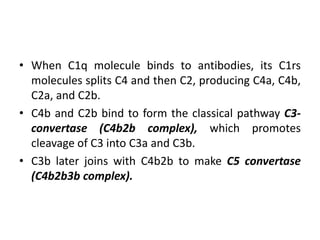
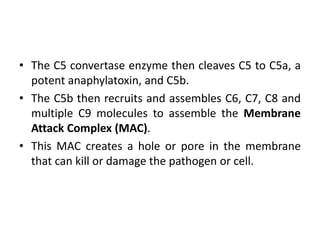
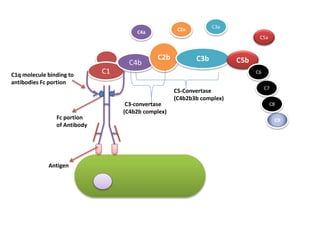
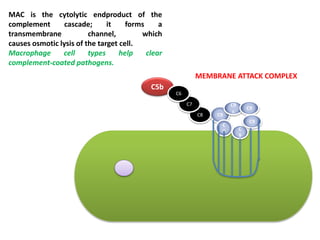
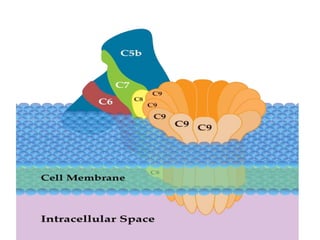
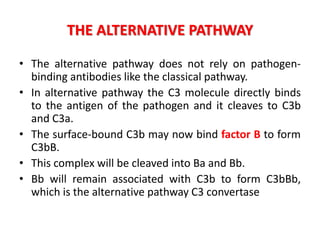
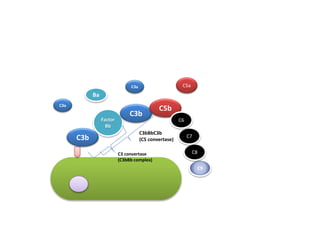
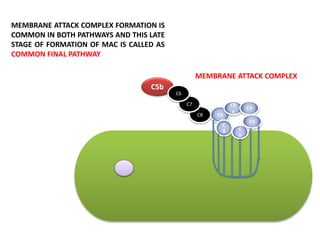
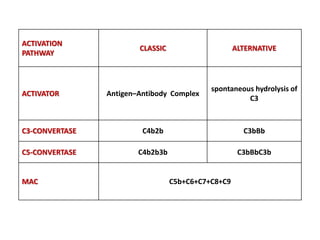
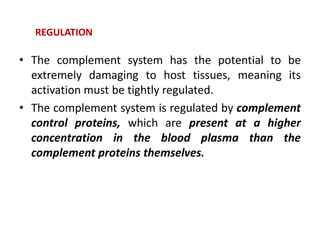
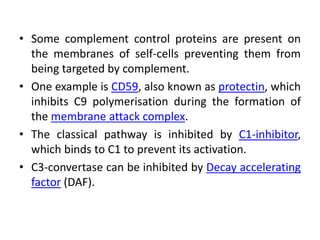
The complement system is part of the innate immune system and consists of over 20 proteins that complement the function of antibodies and immune cells. It can be activated via the classical pathway by antibodies binding to pathogens or via the alternative pathway through direct binding of C3 protein to pathogens. Both pathways result in the formation of the membrane attack complex that creates pores in the pathogen's membrane to kill it. The complement system is tightly regulated to prevent damage to host cells and deficiencies can increase susceptibility to certain infections.